Filamentary Keratitis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
- Filamentary Keratitis ICD-9 370.23
Disease
Filamentary keratitis is a condition in which strands (“filaments”) composed of degenerated epithelial cells and mucus develop on and adhere to the corneal surface causing pain and foreign body sensation.
Etiology
The etiology of filamentary keratitis is related to an alteration in the components of the tear film and/or abnormalities of the corneal surface. It is associated with a number of ocular surface diseases and conditions.
Risk Factors
Any alteration of the tear film or corneal surface can increase the risk for filamentary keratitis.
Common risk factors include:
- Aqueous tear deficiency as in keratoconjunctivitis sicca (or dry eye)
- Corneal exposure (e.g. seventh nerve palsy)
- Occlusion abnormalities such as blepharoptosis
- Ocular surgery (e.g. keratoplasty)
- Systemic diseases with effects on the ocular surface (e.g. Sjogren’s syndrome)
- Extended use of anticholinergic medications
- Superior limbic keratoconjunctivitis
- Other ocular surface abnormalities.
General Pathology
In filamentary keratitis, there is often an increase in the tear film mucus to aqueous ratio. This is commonly due to a decrease in aqueous tear production, but may also be due to increased production or accumulation of the mucinous component. This alteration in tear film makeup sets the stage for formation of mucoid filaments. Small defects in the corneal epithelium provide an anchoring surface for the filaments. Mucin attaches to the epithelial defect and loose epithelial strands are incorporated into the mucin strand attached to the surface. Filaments may be small sessile adhesions or longer strings that cause irritation and discomfort.
Pathophysiology
It is hypothesized that the initial step in the development of filamentary keratitis is damage to basal epithelial cells, epithelial basement membrane, or Bowman’s layer leading to focal detachments of the epithelial basement membrane. Blinking causes these areas of detachment to become elevated leading to irritation, inflammation, and increased mucus production. The sites of epithelial damage provide the scaffold for filaments to develop. A postmortem analysis of a cornea in a patient with this condition revealed inflammatory cells and fibroblasts just beneath the basal epithelium.
Primary Prevention
Filamentary keratitis generally occurs in association with an underlying condition. The primary preventative measure is lubrication in the setting of dry eye.
Diagnosis
History
Patients with filamentary keratitis complain of foreign body sensation. They may also have redness, epiphora, blepharospasm, and photophobia.
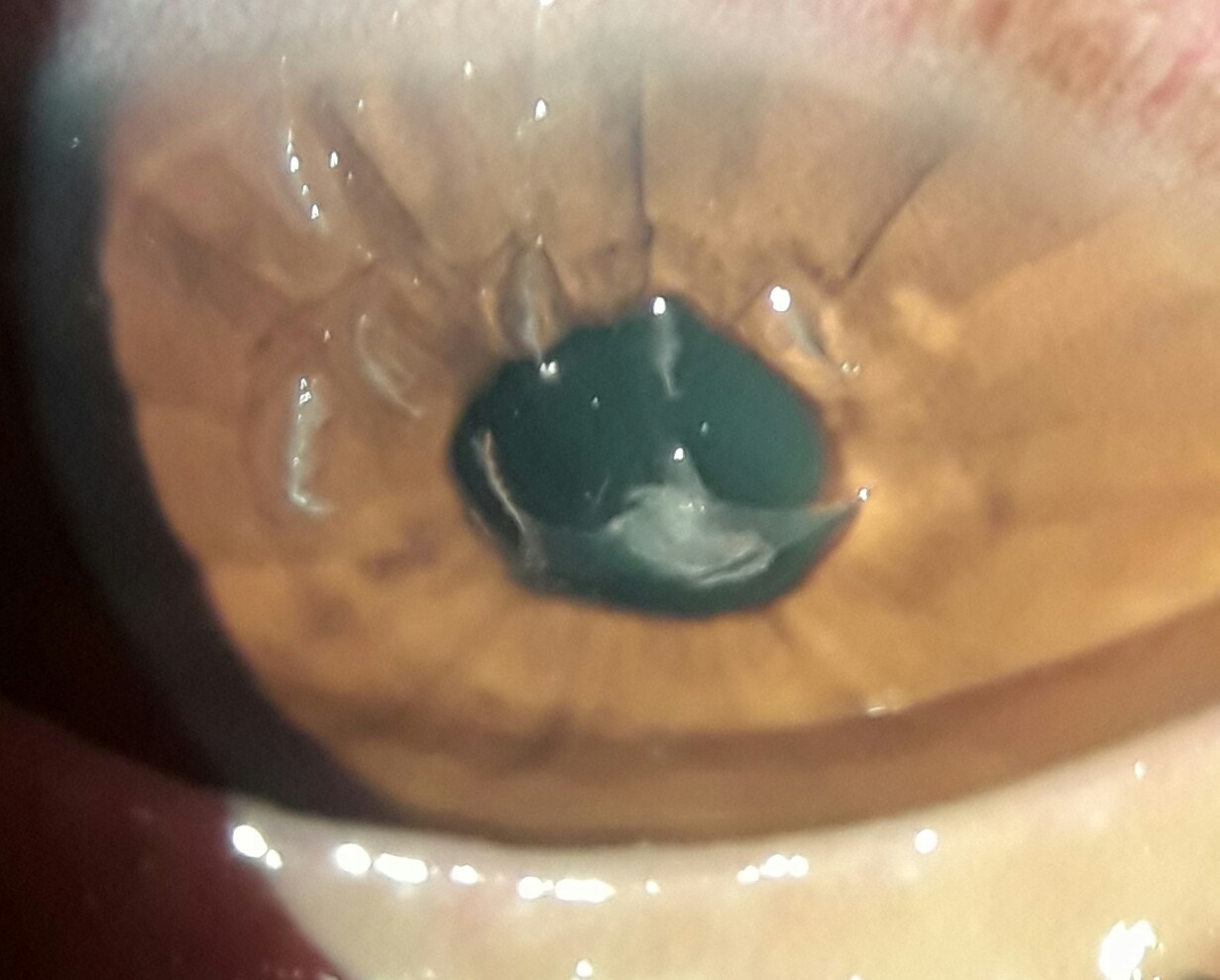
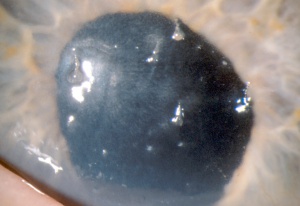
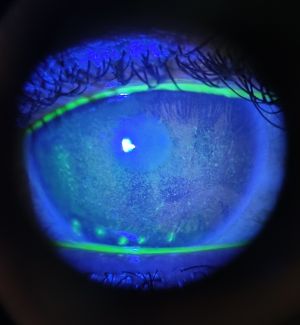
Physical Examination
Slit lamp examination reveals filaments (‘mucoepithelioid” strands) adherent to the corneal surface. The filaments can vary from 0.5mm to 10mm in length. A gray colored subepithelial opacity can sometimes be seen at the base of the filament. Blinking causes painful traction on the filaments and may detach them, leaving behind an epithelial defect. Filaments stain best with rose Bengal, but can be seen with fluorescein as well. The location of the filaments can help determine the underlying cause. Filaments due to dry eye syndromes tend to be found in the interpalpebral space, those due to ptosis superiorly, and those due to surgery at the site of the wound or surgical trauma
Signs
Signs include multiple filamentary attachments firmly adherent to the corneal surface, decreased aqueous tears, increased mucin in the precorneal tear film, subepithelial opacities at the base of filaments, or frank corneal epithelial defects.
Symptoms
Symptoms can vary from mild to severe foreign body sensation that is exacerbated by blinking and is associated with photophobia, blepharospasm, and epiphora. The patient may also complain of a red eye.
Clinical diagnosis
The diagnosis of filamentary keratitis is made clinically with history and slit lamp exam.
Diagnostic procedures
Slit lamp exam demonstrates firmly adherent filaments on the corneal surface. A Schirmer test may be helpful in establishing the diagnosis of a dry eye syndrome.
Laboratory test
There is no specific laboratory testing indicated for filamentary keratitis. However, if suspicion is high for underlying systemic disease (such as Sjogren's Syndrome) that has not yet been diagnosed, a systemic work-up may be indicated.
Differential diagnosis
Corneal filaments are pathognomonic for this condition, but there is a broad differential for the underlying cause of filamentary keratitis. The differential for underlying disease includes tear film abnormalities, lid malpositions, previous ocular surgery, and toxic keratopathies.
Management
General treatment
The treatment of filamentary keratitis can be challenging and is often chronic. Paramount in the overall treatment of filamentary keratitis is management of underlying conditions such as dry eye syndrome, medication toxicity, and blepharoptosis.
Medical therapy
Management of filamentary keratitis relies on identifying and controlling predisposing factors. First line treatment includes topical therapy with lubricant drops and ointment. Low water-content bandage contact lenses may be helpful temporarily in cases that do not respond to lubrication alone. The bandage contact lens should be used in combination with artificial tears and prophylactic topical antibiotic. A mucolytic agent such as 10% N-Acetylcysteine can be used topically to decrease the viscosity of the mucinous component of the tear film. Topical sodium chloride drops and ointments may also help by increasing hydration and promoting adherence of the epithelial cells to the underlying corneal tissue preventing formation of filaments. Adjunct treatment with botulinum toxin may be considered in refractory cases.[1] There are case reports and small case series that demonstrate the efficacy of sutureless amniotic membrane grafts to manage this condition. [2] Another possible treatment for refractory keratitis is autologous serum eye drops. [3] Anti-inflammatory treatments such as topical steroids (pulse or chronic), cyclosporine, and lifitegrast and topical NSAIDs[4] may be helpful but potential benefits must be weighed against possible risks.
Medical follow up
Patients should be re-examined shortly after the initiation of medical therapy. Bandage contact lenses should be left in place for no more than one month.
Surgery
Surgery is not indicated for filamentary keratitis; however, there are maneuvers and procedures that can be very helpful. Filaments can be removed at the slit lamp using jeweler’s forceps. Care should be taken to avoid disrupting the epithelium at the base of the filament if possible. Manual removal of the filaments may help in alleviating symptoms temporarily but is only a temporizing measure and is not successful without concurrent medical treatment. Punctal occlusion, using either punctal plugs or punctal cauterization, may be helpful in cases of underlying aqueous tear deficiency.
Complications
Infectious keratitis is a potential complication, especially when a bandage contact lens is used for therapy or when filaments break off leaving epithelial defects behind.
Prognosis
Prognosis depends upon effectiveness in managing the predisposing condition, but is generally good. Patience is often required in the chronic management of this condition. Remission is most difficult to achieve in filamentary keratitis due to brain lesions.
References
- Davidson RS, Mannis MJ. Filamentary Keratitis. In: Krachmer JH, Mannis MJ, Holland EJ, editors. Cornea. Vol 1. 3rd ed. Philadelphia: Elsevier/Mosby; 2011. P. 1093-96.
- Van Meter WS, Katz D, Cook BG. Filamentary Keratitis. In: Holland EJ, Mannis MJ, Lee WB, editors. Ocular Surface Disease: Cornea, Conjunctiva, and Tear Film. Philadelphia: Elsevier Saunders; 2013. P. 213-16.
- Zaidman GW, Geeraets R, Paylor RR, et al. The histopathology of filamentary keratitis. Arch Ophthalmology 1985; 103: 1178-81.
- Tanioka H, Yokoi N, Komuro A, et al. Investigation of the corneal filament in filamentary keratitis. Invest Ophthalmol Vis Sci 2009; 50:3696-702.
- ↑ Gumus K, Lee S, Yen MT, Pflugfelder SC. Botulinum toxin injection for the management of refractory filamentary keratitis. Arch Ophthalmol. 2012 Apr;130(4):446-50. doi: 10.1001/archophthalmol.2011.2713. PMID: 22491914.
- ↑ Case report on biotissue website; Harthan JS, Sicks LA, "Sutureless Amniotic Membrane (Prokera) for Filamentary Keratitis: A Case Series, J Dry EyeOcc Surf Dis Vol 2(SP1):e10-e16; May 9, 2019
- ↑ Read et al, "Treatment of Refractory Filamentary Keratitis with Autologous Serum Tears,: Eye Contact Lens, 2017 Sep;(43)5:e16-e18.
- ↑ Weiss M, Molina R, Ofoegbuna C, Johnson DA, Kheirkhah A. A review of filamentary keratitis. Surv Ophthalmol. 2022 Jan-Feb;67(1):52-59. doi: 10.1016/j.survophthal.2021.04.002. Epub 2021 Apr 20. PMID: 33862042.