Eye Banking
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Overview
According to the Eye Bank Association of America (EBAA) (Fig. 1), eye banks can be defined as “a non-profit organization that obtains, medically evaluates and distributes eye tissue for transplant, research, and education” [1]. Ideally, an eye bank should function autonomously and not be part of a medical organization[2].
Eye banks feature a wide range of functions and specializations. Its operation may be based on: retrieval, storage, tissue evaluation, donor eligibility assessment, processing and distribution of transplant parts[1]. In relation to their specialization, they may work only with eyes, eyes and tissues or be part of an organ procurement organization[1]. In addition, several of these institutions work for the advancement of medicine, operating as research centers on issues related to eye storage and the restoration of sight.
Structurally, eye banks should have communication facilities, access to equipment such as a slit lamp and laminar flow hood, surgical instruments, sterilization facilities, a serology laboratory, preservation facilities and an adequate transport system. The division of functions basically takes place through two sectors: medical and administrative. The medical sector is coordinated by a medical director, who is usually an experienced corneal surgeon, and by professionals in the area who are responsible for supervising and carrying out technical procedures. The administrative sector, on the other hand, is coordinated by a team that is responsible for the institution's bureaucratic issues. Specifically, the medical ward handles tissue collection and its evaluation, preservation, and distribution. On the other hand, the administration is responsible for public awareness programs, contacting government and voluntary and health agencies, and fundraising[2].
History
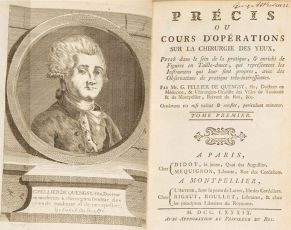
The history of the emergence of eye banks is directly related to the development of corneal transplantation and tissue storage techniques. Corneal transplantation was conceptualized in the late 18th century by Guillaume Pellier de Quengsy[3] (Fig. 2), but it took more than 100 years until the first transplant in humans was performed by Eduard Zirm in 1905[4] (Fig. 3). Despite advances, who made possible the idealization of the first eye banks was Vladimir Filatov (Fig. 4) who, in the 1930s, documented[5] and popularized the use of human cadaver corneas in well-done transplants. The eyes were enucleated within a maximum of a few hours after the donor's death, as the corneas were stored in ice boxes at 4°C and used in the interval between 20h-56h post-mortem[5]. This feat made it possible for the donor tissues to be stored and the first eye banks to emerge.
Eye banks began in the 1940s, when Dr. R. Townley Paton inaugurated the first eye bank in the US - the Eye Bank for Sight Restoration, founded in New York in 1944[6]. The storage techniques, at the principle, were very rudimentary, being restricted to small glass bottles where the eyes were under a condition of humidity and controlled temperature[7] (Fig. 5). In order to preserve the corneal endothelium, it was necessary for the transplant to take place within a maximum of 48 hours after the death of the donor[6]. Furthermore, quality control uses only the appearance of the cornea and the post-mortem time as a criterion, with no control over the transmission of possible infectious diseases[7].
In the early 1970s, McCarey and Kaufman[8] developed new techniques for preserving ocular tissues with the aim of maintaining the viability of the corneal endothelium. They used a standard culture medium with very low levels, supplemented with dehydrating agents and antibiotics. This technique allowed the conservation of the cornea for a period of 7 to 10 days[8]. Currently, new research and advances in storage techniques are allowing the donated tissue to be viable for a longer period. In organ culture, for example, the cornea can be preserved for up to about 5 weeks[9].
Eye Banks in North America (USA)
In 1961, the Eye Bank Association of America (EBAA) was founded by the eye bank committee of the American Academy of Ophthalmology and Otolaryngology (AAO&O) with the role of acting as the organization's medical board, promoting and systematizing the practice of storage eyes [10] [11]. The formation of the EBAA had worldwide repercussions, as in addition to being the first eye bank association in the world, it was also the first organization to represent transplant professionals of any type of tissue and organs [11] and to establish medical protocols, accreditation procedures and technical certificates to its members [10].
In June 1980, during the EBAA Annual Meeting, the first EBAA Medical Standards [10] was launched, which aimed to standardize procedures for tissue collection, preservation and distribution. This document aimed at balancing practical and scientific knowledge, having been written by a group of experienced corneal surgeons who formed the Medical Advisory Board. In order for these quality standards to be followed by the members of the organization, in 1981 the EBAA Accreditation Program [10] was created, which consisted of an inspection and accreditation program, in which teams formed by technicians and physicians carried out regular visits to the eye banks members of the association. The high quality level of this program made this practice recognized by the United States Food and Drug Administration (FDA) [11]. As a result of this growing evolution of the EBAA, in 1981 the profession of Certified Eye Bank Technician (CEBT) [10] emerged, which increased the quality of both the eye banks and the workforce in these locations. This title can be achieved by passing the certificate exam created by the Certification Board that establishes the necessary requirements for the certification of technicians [11].
One of the most striking results of the systematization of the quality of procedures performed by eye banks in the USA was demonstrated by the 2016 Global Survey of Corneal Transplantation and Eye Banking [12] which indicated that the country was the world leader in corneal transplantation, having a index of 366/100,000 corneal donors per capita. Currently, the EBAA represents all eye banks in the United States, but does not restrict its membership to US borders, allowing the adherence of eye banks from Canada and other countries abroad [11], which must meet the requirements of safety and performance required by the institution.
References
- ↑ 1.0 1.1 1.2 What is an eye bank? - Eye Bank Association of AmericaEye Bank Association of America. Accessed November 8, 2021. https://restoresight.org/cornea-donation/understanding-cornea-donation/what-is-an-eye-bank/
- ↑ 2.0 2.1 Rao GN. What is eye banking? Indian J Ophthalmol. 1996;44(1):1. Accessed November 8, 2021. https://www.ijo.in/article.asp?issn=0301-4738;year=1996;volume=44;issue=1;spage=1;epage=2;aulast=Rao
- ↑ Pellier de Quengsy G: Précis au cours d'opérations sur la chirurgie des yeux. Paris, Didot, 1789.
- ↑ Zirm E. Eine erfolgreiche totale Keratoplastik [translated from the German by Chris Sandison, Technical Translations from German, Bath]. Graefes Arch Ophthalmol 190664580–593.
- ↑ 5.0 5.1 FILATOV VP, Sitchevska O. TRANSPLANTATION OF THE CORNEA. Arch Ophthalmol. 1935;13(3):321-347. doi:10.1001/ARCHOPHT.1935.00840030011001
- ↑ 6.0 6.1 Güell JL, El Husseiny MA, Manero F, Gris O, Elies D. Historical Review and Update of Surgical Treatment for Corneal Endothelial Diseases. Ophthalmol Ther. 2014;3(1-2):1-15. doi:10.1007/s40123-014-0022-y
- ↑ 7.0 7.1 Bredehorn-Mayr T, Duncker G, Armitage WJ. Corneal Grafting and Banking. Dev Ophthalmol Basel, Karger. 2009;43:1-14.
- ↑ 8.0 8.1 McCarey BE, Kaufman HE. Improved corneal storage. Invest Ophthalmol. 1974;13(3):165-173.
- ↑ Pels L. Organ culture: the method of choice for preservation of human donor corneas. Br J Ophthalmol. 1997;81(7):523-525. doi:10.1136/BJO.81.7.523
- ↑ 10.0 10.1 10.2 10.3 10.4 History of EBAA and Eye Banking - Eye Bank Association of AmericaEye Bank Association of America. Accessed December 7, 2021. https://restoresight.org/history-of-ebaa-and-eye-banking/
- ↑ 11.0 11.1 11.2 11.3 11.4 The Evolution of Eye Banking in the United States: Landmarks in the History of the Eye Bank Association of America - The International Journal of Eye Banking. Accessed December 7, 2021. https://eyebankingjournal.org/article/evolution-eye-banking-united-states-landmarks-history-eye-bank-association-america/
- ↑ Gain P, Jullienne R, He Z, et al. Global Survey of Corneal Transplantation and Eye Banking. JAMA Ophthalmol. 2016;134(2):167-173. doi:10.1001/JAMAOPHTHALMOL.2015.4776
Observation: Ana Vega and Gustavo Correia worked together on this publication and contributed equally to it.