Exophthalmometry
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Exophthalmometer is an instrument used to determine axial globe position in relation to the orbital rim.
Introduction
Exophthalmometry is a technique used to provide a quantitative clinical measurement of the anterior position of the globe in relation to the orbital rim.[1] It measures the distance between two lines, one passing through the lateral orbital margin and the other passing through the apex of the cornea while the eye is in the primary position. The relational measurement between the corneal apex from the lateral rim is measured in millimeters to determine globe axial position. Multiple methods of exophthalmometry exist such as clinical, radiologic, and digital photography. Clinical exophthalmometry is the most commonly used technique in practice.
Clinical Exophthalmometry
To perform clinical exophthalmometry, a portable exophthalmometer is used to measure the axial position of the globe. If an instrument is utilized that provides for bilateral measurements, a base is recorded in addition to the axial measurements for each eye. This allows for the same base to be used between measurements across time to ensure accuracy in comparing changes over time. Due to ease of use and portability, clinical measurements can be readily obtained and monitored over time, allowing the physician to track the progression of conditions such as enophthalmos or proptosis. There are different types of clinical exophthalmometers including the Hertel, Luedde, Naugle, and Mourits. The instruments most commonly used in practice are the Hertel and the Luedde exophthalmometers.
Hertel Exophthalmometer
The Hertel exophthalmometer measures the globe position of the eye by calculating the distance from the lateral orbital rim to the surface of the cornea. This device is composed of a horizontal calibrated bar with carriers holding sliding mirrors and a scale reading at both ends. The mirrors are inclined at 45 degrees to enable visualization of both the scale reading and the apex of the cornea. Notches at the front of the carriers that hold the mirrors are placed on the bony part of the lateral orbital rim of a patient, using the smallest base possible without distorting the eyelids or causing patient discomfort. While the patient is looking straight and fixated on a point, the examiner can visualize and measure the apex of the cornea by using the millimeter scale reading aligned with the eye in the carrier.
Additionally, the distance on the horizontal bar is recorded as the baseline measurement for the distance of the bilateral lateral orbital rims, which can be used for future comparisons.[2] The Hertel exophthalmometry is simple, convenient, and easy to use, but it has been shown to produce low accuracy, user variability. and poor reproducibility.[3][4][5] For example, if strabismus is present, the examiner should ask the patient to fixate with the measuring eye one at a time, as a large strabismic deviation may give false readings.
It is also important to be aware that facial trauma patients with misalignment of the bony orbital rim (such as in ZMC fractures) will give unreliable measurements. The reproducibility can be improved by using a standardized protocol using the same exophthalmometer and the same base distance.[6]
Luedde Exophthalmometer
The Luedde exophthalmometer measures the globe position unilaterally from the lateral orbital rim by using a transparent ruler calibrated in millimeters. Similar to the Hertel exophthalmometer, the end of the ruler is notched to fit in the bony prominence of the lateral orbital margin. While the patient looks straight fixated at one point, the examiner stands at the side of the patient and measures how much the apex of the cornea protrudes through the transparent ruler.[2] In addition, the Luedde exophthalmometer is easier to use and relatively cheaper than the Hertel exophthalmometer. However, it does not allow simultaneous measurement of both eyes and the distance between the eyes.
Naugle Exophthalmometer
The Naugle exophthalmometer measures the globe protrusion using the superior and inferior orbital rims as reference structures. This type of instrument is useful in a patient with lateral orbital displacement, inflammation from a trauma with poor lateral rim landmark, or a patient status post a lateral orbital decompression surgery. It provides the most accurate measurement for patients with lateral rim fractures or defects. This device can also provide measurement for both hyperglobus and hypoglobus with a vertical scale from the center of the pupil.[7]
Mourits Exophthalmometer
The Mourits exophthalmometer is a newly developed standard device in 2015 similar to the Hertel, except that Mourits is parallax-free. Parallax free uses one reflective prism instead of two as found in the Hertel exophthalmometer. The main drawback of the Hertel is parallax error, which causes inaccurate and shifted perception of the position of an object when viewed from different angles. Using a single mirror, the Mourits has been shown to eliminate this parallax error, providing more consistent measurements.[8][3]
To use the Mourits meter, the instrument is placed horizontally against the lateral orbital margins. The examiner looks through the prism on each side to align the black marking and the red line on the prism and then moves the prism until the red line reaches the image of the apex of the cornea. When looking through the prism, the anterior globe position of the right eye should be measured using the examiner’s left eye and vice versa.[3]
Interpretations
The normal range is 12-21mm, however interpreting the measurement should be done with caution as it can vary with different racial and age groups. The mean normal protrusion measurements in Caucasians were 16.5 mm in males and 15.4 mm in females, whereas the same measurements were higher in African Americans (AA) at 18.5 mm in males and 17.8 mm in females. In Asians, the mean protrusion measurement was 14.4, ranging from 8 to 20 mm, reporting significantly lower than in Caucasians.[9]
Likewise, the upper limits of normal were higher in African Americans (24.7 mm AA male and 23.0 mm AA female vs. 21.7 mm Caucasian male and 20.1 mm female).[10] Furthermore, the normal range of males was higher than that of females by about 1-1.5 mm, depending on race. An asymmetry of more than 2 mm between the two eyes is considered abnormal and should warrant further evaluation.[11]
In the pediatric population, the mean protrusion measurements increased with age: less than 4 years old (13.2 mm), 5-8 years old (14.4 mm), 9-12 years old (15.2 mm), and 13-17 years old (16.2 mm). There was no difference in the measurements between males and females.[12]
Indications
Exophthalmometry is indicated for various pathologic conditions affecting eye protrusion. A valuable utility of exophthalmometry is that it allows the clinician to objectively record a patient’s degree of enophthalmos/exophthalmos and track any change over time.
Causes of Enophthalmos
- Orbital trauma
- Orbital surgery
- Orbital varix
- Silent Sinus Syndrome
- Loss of or remodeling of the sphenoid wing secondary to neurofibromatosis
- Age-related bony changes and/or fat atrophy
- Radiotherapy
- Lipodystrophy
- Linear scleroderm
- Parry-Romberg syndrome
- Drugs
- HIV
Causes of Exophthalmos
- Orbital trauma
- Orbital varix
- Orbital cellulitis
- Orbital tumors
- Thyroid-related eye disease
- Sarcoidosis
- Granulomatosis with polyangiitis
- IgG4-related disease
- Carotid-cavernous fistula
- Cavernous sinus thrombosis
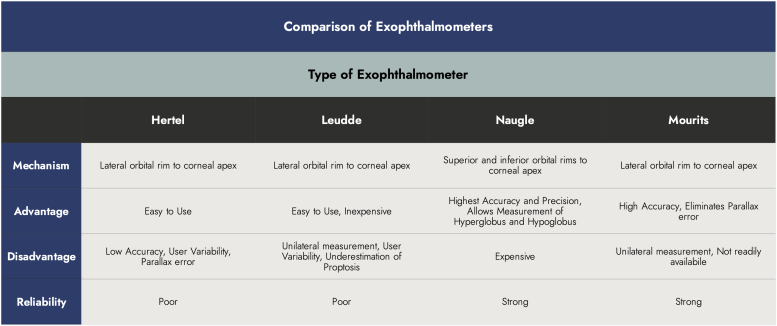
Comparison of Different Clinical Exophthalmometers
The Hertel, Luedde and Mourits exophthalmometers measure proptosis using the lateral orbital rim as the reference point. Any surgery, disease, or trauma that causes any changes in the position of the lateral rim can alter the accuracy of the measurement. In this instance, the Naugle exophthalmometer should be used because it uses the forehead (superior orbital rim) and cheek (inferior orbital rim) as the reference point.[15] In comparison to Hertel exophthalmometers, the Naugle was shown to have higher precision and reproducibility with comparable accuracy. Additionally, the Naugle provided the best patient comfort, thus increasing patient cooperation with the exam. [16]
A comparative study of Mourits, Luedde, and Hertel exophthalmometers demonstrated that the most accurate measurement of proptosis was taken with Mourtis, intermediate accuracy with Hertel, and low accuracy with Luedde exophthalmometer when compared to proptosis measurement by computed tomography (CT) biometry. Furthermore, inter-user reproducibility was the greatest in Mourtis. This study also reported that Luedde produces an underestimation of actual proptosis. The Hertel exophthalmometer produces overestimation, especially for small values, and underestimation for larger values. Of all three, Mourtis exophthalmometer produces the most reliable proptosis measurement with only a slight underestimation.[17]
Regardless of which device a clinician uses, the proptosis measurement should be considered with caution due to potential underestimation or overestimation when using different exophthalmometers and done by different examiners.[17]
Radiologic Exophthalmometry
Radiologic exophthalmometry utilizes computed tomography (CT) to provide an objective measurement of proptosis. Multiple techniques exist for measuring proptosis with CT. In one method, a horizontal line is drawn between the lateral orbital rims that bisects the lens in the axial plane. A perpendicular line is then drawn to the apex of the cornea and measured.
In another method, a line is drawn between the lateral and medial orbital rims on each side that bisects the lens in the axial plane. A perpendicular line is then drawn to the apex of the cornea and measured.
In the last method, a line is drawn between the superior and inferior orbital rims that bisects the lens in the sagittal plane. A perpendicular line is then drawn to the apex of the cornea and measured.
Each technique has been shown to have a statistically significant relationship with Hertel exophthalmometry. CT scans are easily accessible and are associated with higher repeatability and accuracy, allowing early detection of conditions such as thyroid eye disease.[18] However CT imaging is not routinely used for the sole purpose of measuring proptosis due to the risk of subjecting patients to unneccessary radiation and the high associated costs, as well as easily available exophthalmometry devices for clinic use. [19]
Digital Photography Exophthalmometry
Digital photography exophthalmometry is a simple method of noninvasive measurement involving a camera that allows measurements to be easily documented and stored online. [19] In this technique, a surgical pen mark is made at the height of the lateral canthus on the anterior border of the lateral orbital rim. A sticker of a selected size is also placed on the patient’s lateral forehead to allow for digital calibration. Once the side-view photographs are taken, the distance between the lateral orbital rim and the corneal apex is measured.
While digital exophthalmometry has been shown by some authors to produce good results in patients with Graves Orbitopathy, this technique is associated with several drawbacks. One downside is the need for good standardization for parameters such as gaze, light, and camera settings. In addition, there has been documented higher intra-clinician variability for digital compared to clinical and radiologic techniques. Therefore, digital measurements have lower reproducibility and are not accurate enough to replace the other modalities.
References
- ↑ Chang AA, Bank A, Francis IC, Kappagoda MB. Clinical exophthalmometry: a comparative study of the Luedde and Hertel exophthalmometers. Aust N Z J Ophthalmol. 1995;23(4):315-318. doi:10.1111/j.1442-9071.1995.tb00182.
- ↑ Jump up to: 2.0 2.1 Stein, H. A., Stein, R. M., & Freeman, M. I. Chapter 10: Understanding ophthalmic equipment. In The ophthalmic assistant: A text for Allied and associated ophthalmic personnel. Elsevier; 2018:114-174
- ↑ Jump up to: 3.0 3.1 3.2 Genders SW, Mourits DL, Jasem M, Kloos RJ, Saeed P, Mourits MP. Parallax-free exophthalmometry: a comprehensive review of the literature on clinical exophthalmometry and the introduction of the first parallax-free exophthalmometer. Orbit. 2015;34:23-9.
- ↑ Dickinson AJ, Perros P. Controversies in the clinical evaluation of active thyroid-associated orbitopathy: use of a detailed protocol with comparative photographs for objective assessment. Clin Endocrinol (Oxf). 2001;55:283-303. 8.
- ↑ Musch DC, Frueh BR, Landis JR. The reliability of Hertel exophthalmometry. Observer variation between physician and lay readers. Ophthalmology. 1985;92:1177-80
- ↑ Bingham CM, Sivak-Callcott JA, Gurka MJ, et al. Axial globe position measurement: a prospective multicenter study by the International Thyroid Eye Disease Society. Ophthal Plast Reconstr Surg. 2016;32:106-12.
- ↑ Brodie, SE. Chapter 7: Oculofacial Plastics and Orbital Surgery. In Basic and Clinical Science Course. American Academy of Ophthalmology.
- ↑ Nightingale, C.L. and K. Shakib, Analysis of contemporary tools for the measurement of enophthalmos: a PRISMA-driven systematic review. Br J Oral Maxillofac Surg, 2019. 57(9): p. 904-912.
- ↑ Erb, M.H., Tran, N.H., McCulley, T.J., Bose, S., Exophthalmometry Measurements in Asians. Invest. Ophthalmol. Vis. Sci. 2003. 44(13):662.
- ↑ Migliori, M.E. and Gladstone, G.J., Determination of the normal range of exophthalmometric values for black and white adults. Am J Ophthalmol, 1984. 98(4): p. 438-42.
- ↑ Chen B, Perry JD, Foster JA. Chapter 88: Evaluation of an adult with orbital tumor. In Clinical Ophthalmic Oncology. W. B. Saunders; 2007:524-527.
- ↑ Dijkstal, J.M., et al., Normal exophthalmometry measurements in a United States pediatric population.Ophthalmic Plast Reconstr Surg, 2012. 28(1): p. 54-6.
- ↑ Saravanan A, Patel BC. Enophthalmos. In: StatPearls. Treasure Island (FL): StatPearls Publishing; April 3, 2023.
- ↑ Butt S, Patel BC. Exophthalmos. In: StatPearls. Treasure Island (FL): StatPearls Publishing; June 26, 2023.
- ↑ Nerad, J.A. Chapter 14: Diagnostic Approach to the Patient with Proptosis. In Techniques in Ophthalmic Plastic Surgery. Elsevier; 2021:545-610.
- ↑ Cole HP, Couvillion JT, Fink AJ, Haik BG, Kastl PR. Exophthalmometry: a comparative study of the Naugle and Hertel instruments. Ophthalmic Plast Reconstr Surg. 1997 Sep;13(3):189-94. PMID: 9306438.
- ↑ Jump up to: 17.0 17.1 Delmas, J., et al., Comparative study of 3 exophthalmometers and computed tomographic biometry. Eur J Ophthalmol, 2018. 28(2): p. 144-149.
- ↑ Park NR, Moon JH, Lee JK. Hertel exophthalmometer versus computed tomography scan in proptosis estimation in thyroid-associated orbitopathy. Clin Ophthalmol. 2019;13:1461-1467. Published 2019 Aug 2. doi:10.2147/OPTH.S216838
- ↑ Jump up to: 19.0 19.1 Pereira TS, Kuniyoshi CH, Leite CA, Gebrim EMMS, Monteiro MLR, Pieroni Gonçalves AC. A Comparative Study of Clinical vs. Digital Exophthalmometry Measurement Methods. J Ophthalmol. 2020;2020:1397410. Published 2020 Mar 23. doi:10.1155/2020/1397410