Dry Eye Syndrome Questionnaires
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
A number of questionnaires have been developed to assess a patient’s subjective experience of dry eye symptoms in order to produce more objective and reproducible data that can be used to better manage and treat patients with dry eye disease. According to the Definition and Classification Subcommittee of the International Dry Eye Workshop, “Dry eye is a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles.”[1] Clinicians have many questionnaires that they can utilize in assessing their patients. Currently the most versatile and used questionnaires include the National Eye Institute Visual Function Questionnaire-25 and the Ocular Surface Disease Index due to their mutlidemsionality and their assessment of the quality of life changes in the patient.
National Eye Institute Visual Function Questionnaire-25 (NEI-VFQ25)
The NEI-VFQ25 was created by the National Eye Institute to assess the effect of visual impairment on the patient’s current health-related quality of life, including questions dealing with irritation in and around the eye.[2] The 25-item questionnaire gives a score on a scale of 0 to 100 points. A score of 0 is the worst score, and a score of 100 is the best score and means the patient has no vision problems.
This questionnaire was developed from a 51-item version of the NEI-VFQ. The 25-item questionnaire was developed to be a shorter version of the original that preserved its multidimensionality, reliability, and validity.[3] The questionnaire has several subscale categories that assesses different aspects of health-related quality of life including overall health, overall vision, difficulty with near vision, difficulty with distance vision, limitations in social functioning due to vision, role limitations due to vision, dependency on others due to vision, mental health symptoms due to vision, future expectations for vision, driving difficulties, and pain and discomfort around the eyes.[3] Due to its decreased number of items the shorter questionnaire takes 5 to 10 minutes while the longer questionnaire takes 15 minutes on average, making it easier to use in clinical settings and research.[3]
When used in the setting of patients with Sjögren’s syndrome-related dry eye, the NEI-VFQ subscale categories show weak to moderate associations with the ocular surface parameters (Oxford score, van Bijsterveld score, tear film break up time, Schirmer score with and without anesthesia).[4] Patients therefore might not have an accurate assessment of their dry eye symptoms if they suffer from Sjögren’s syndrome based on the moderate to weak association with ocular surface parameters.
While NEI-VFQ25 is a more succinct version of its 51-item predecessor, it is also a questionnaire that was developed from a study that had specific enrollment criteria that selected patients with moderate-to-severe disease. Using this patient population makes the questionnaire possibly less sensitive to the symptoms in patients with milder forms of ocular disease.[3] When validation studies were performed, it was found that correlations between responses given for the Early Treatment Diabetic Retinopathy study (ETDRS) and the NEI-VFQ25 visual acuity ranged from 0.65 to 0.70, with other subscales showing correlations ranging from 0.39 to 0.69.[3] The only subscale outside of these ranges was ocular pain which had a correlation of 0.06 to 0.11.[3] This questionnaire’s strength therefore lies in its good use of subscales in order to encompass symptoms of diverse etiologies in order to provide a more versatile assessment. Clinicians are encouraged to use this questionnaire to assess the effects that various diseases and treatments have on a patient’s quality of life.
Survey Available with open access at: [1]
Ocular Surface Disease Index (OSDI)
The OSDI, which was created by the Outcomes Research Group at Allergan Inc in order to quickly assess the symptoms of ocular irritation in dry eye disease and how they affect functioning related to vision.[5] This 12-item questionnaire assesses dry eye symptoms and the effects it has on vision-related function in the past week of the patient’s life.[6] The questionnaire has 3 subscales: ocular symptoms, vision-related function, and environmental triggers. Patients rate their responses on a 0 to 4 scale with 0 corresponding to “none of the time” and 4 corresponding to “all of the time.” A final score is calculated which ranges from 0 to 100 with scores 0 to 12 representing normal, 13 to 22 representing mild dry eye disease, 23 to 32 representing moderate dry eye disease, and greater than 33 representing severe dry eye disease.[7]
The OSDI assesses quality of life measures, which aligns the questionnaire with Federal Food and Drug Administration’s emphasis on utilizing patient-reported outcomes in order to support medicinal product submissions and clinical drug trial efficacy.[6] Tear break up time is another way that clinicians assess dry eye disease. When OSDI and tear break up time were analyzed, a statistically significant inverse correlation between the test scores was found; the higher or worse the OSDI score, the lower or worse the tear break up time was.[8]
The OSDI limits itself by assessing a small number of dry eye symptoms including sensitivity to light, grittiness, and pain. The questionnaire does not assess other symptoms such as tearing and foreign body sensation.[7] The lack of these fields makes the questionnaire less accurate in assessing specific symptoms that the patient may describe. In addition, while frequency can be a good measure of a patient’s experience of symptoms it is not a complete substitute for the severity of the symptoms that the patient experiences.
The OSDI has demonstrated good specificity (0.83) and a moderate sensitivity (0.60) when distinguishing between patients with dry eye disease and normal subjects.[5] This instrument displays a unique capacity to assess the frequency of dry eye symptoms and their effect on a patient’s visual related functioning.
Survey Available with open access at: [2]
Standard Patient Evaluation of Eye Dryness Questionnaire (SPEED)
The SPEED questionnaire was designed by Korb and Blackie in order to quickly track the progression of dry eye symptoms over time.[9] This questionnaire gives a score from 0 to 28 that is the result of 8 items that assess frequency and severity of symptoms. The symptoms assessed include dryness, grittiness, scratchiness, irritation, burning, watering, soreness, and eye fatigue. The questionnaire further assesses whether these symptoms were not problematic, tolerable, uncomfortable, bothersome, or intolerable.[10] The questionnaire also monitored diurnal and symptoms changes over 3 months.[11] Validity of the questionnaire was determined by seeing how well it was able to segregate patients based on their symptoms, relative to the OSDI questionnaire (gold standard). The resulting sensitivity and specificity were 0.90 and 0.80 respectively.[11]

The survey is available through Tear Science Inc. with no fee.[11][3]
Canadian Dry Eye Epidemiology Study (CANDEES)
This survey was created by the Centre for Contact Lens Research of the University of Waterloo in order to obtain data on the severity and overall prevalence of dry eye symptoms in patients in Canada.[12] The survey was sent to optometric practices in all provinces of Canada, and contained 13 questions covering demographics, contact lens use, medications use, symptoms with and without contact lens usage, mouth dryness, swollen or red eyelids, severity of symptoms in the morning compared to the afternoon, and allergies.[13]
This survey is available on page 626 of “A Patient Questionnaire Approach to Estimating the Prevelance of Dry Eye Symptoms in Patients Presenting to Optometric Practices across Canada.” The fee to use this questionnaire is $374.73.[12] [4]
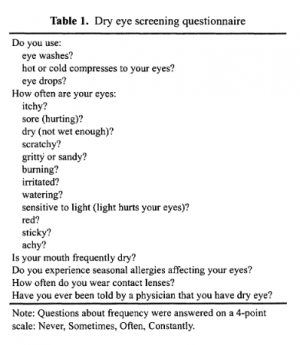
Dry Eye Screening for Dry Eye Epidemiology Projects (DEEP)
This questionnaire was created specifically for screening dry eye in patients in a proposed Dry Eye Epidemiologic Projects study.[14] The questionnaire consists of 19 questions, with only 14 being used in the analysis. The questions covered artificial tear or eye drop use, contact lens use, frequency of ocular symptoms, other types of dryness, and allergies. The sensitivity and specificity of this questionnaire are 0.6 and .94 respectively, based on irritation and dryness as predictor variables.[14] This suggests that this screening tool might be appropriate for dry eye patients in epidemiologic studies.
This survey is available through Springer Science+Business Media with no fee.[14][5]
Dry Eye Questionnaire (DEQ)
The Dry Eye Questionnaire (DEQ) (Begley et al.) was created in order to diagnose dry eye disease and to quantify its severity level. This questionnaire measures several symptoms using four variables: degree of irritation, frequency, intensity in the morning, and intensity late in the day.[15] The patient’s recall period in items that ascertained the experience of the symptoms was within the past week. The DEQ does not demonstrate a correlation with clinical parameters, but allows for differentiating ophthalmic status: dry eye vs. non-dry eye patients, Sjögren syndrome [SS] and keratoconjunctivitis sicca [KCS] vs. non-SS-KCS patients, and control vs. SS-KCS and non-SS-KCS patients.[16] The validity of this survey compared to other symptom questionnaires (OSDI and McMonnies) was assessed, with Spearman correlation coefficients of r = 0.76 and 0.66, respectively.[17]
No permission available for use. [6]
Contact Lens Dry Eye Questionnaire (CLDEQ)
The CLDEQ was developed by Begley et al, to investigate the severity and frequency of dry eye symptoms in contact lens wearers.[18] This questionnaire has 36 items and was derived from the DEQ and is similar, except that patients are asked about dryness symptoms when they are wearing contact lenses.[19] The questionnaire divides symptoms into nine subscales including: dryness, discomfort, visual changes, irritation and soreness, grittiness and scratchiness, burning, foreign body sensation, itching, and photophobia. Within each subscale the questionnaire asks about the frequency of the symptoms, and intensity of the symptoms throughout the day, which is useful for understanding the distribution of symptoms in contact lens wearers throughout the day. When compared to the McMonnies’ Questionnaire, the sensitivity and specificity are 0.83 and 0.67 respectively.[19]
No permission available for use. [7]
Impact of Dry Eye in Everyday Life (IDEEL)
IDEEL is a 57-item questionnaire developed by Abetz et al., that that assess the impact of dry eye symptoms on everyday life.[20] This questionnaire consists of 3 modules: dry eye treatment satisfaction comprising of satisfaction with treatment effectiveness and treatment-related inconvenience/bother, dry eye impact on daily life comprising impact on daily activities, emotional impact, impact on work, and dry eye symptom-bother. This questionnaire assesses the impact of dry eye on quality of life, impact of treatment, and could aid in evaluating treatment effectiveness.[20] Concurrent validity between IDEEL dimensions and DEQ items expressed with Pearson coefficient correlations showed a range of -0.05-0.83.8 The correlations between the clinical findings and the treatment-related bother/inconvenience, symptom-related bother, impact on daily activities, emotional impact due to dry eye, and impact on work due to dry eye were low (p < 0.05).[20]
Survey available through Alcon Research LTD, France.[20] [8]
McCarty Symptom Questionnaire
This questionnaire was developed by McCarty et al. and assesses dry eye disease in an older (over 40 years old) adult population in the city of Melbourne, Australia. The questionnaire ascertained discomfort, foreign body sensation, dryness, itching, tearing, and photophobia on a scale from 0 to 3.[21] If the patient had any of these symptoms they were asked if they thought it was related to hay fever. A history of dry mouth was also obtained and graded on a scale of 0 to 3.[21] The results of this questionnaire were used in an epidemiology study in order to determine the incidence of dry eye in Australia.
Survey available on page 1115 of “The Epidemiology of Dry Eye in Melbourne, Australia.” The fee to use this questionnaire is $29.90.[21][9]
McMonnies Questionnaire
This questionnaire was developed by McMonnies et al. to screen for possible dry eye symptoms and to assess risk factors.[13] This instrument has 14 questions that focus on risk factors of dry eye. These risk factors include gender, age, contact lens history, dry eye symptoms, secondary symptoms, medical conditions associated with dry eye syndrome, dryness of mucous membranes, medication use, and previous dry eye treatments.[22] This questionnaire helps detect dry eye disease, as well as patients at risk for developing dry eye disease due to exposure to specific factors that the instrument indicates.[22] Concurrent validity was fair when compared to the NEI-VFQ25, with a statistically significant correlation with the pain module (r = -0.28 [p = 0.02]).[22]
Survey available on page 4 of “Accuracy of McMonnies Questionnaire as a Screening Tool for Chinese Ophthalmic Outpatients.” The fee to use this questionnaire is $374.73.[23][10]
Ocular Comfort Index (OCI)
The OCI questionnaire was developed by Johnson and Murphy as an instrument that allows for quick assessment of ocular comfort. It has 15 items that were identified from interviews of patients and a literature review. Eight areas were identified: positive (comfort), and negative (visual stability, tiredness, stinging, pain, itching, grittiness, and dryness).[24] Subparts were extrapolated from these areas and quantified with frequency and intensity. The OCI is able to detect symptom improvement before and after lubricant treatment (95% confidence interval of the treatment difference was -5.5 to -8.0 [P < 0.0001]).[24] The validity of the questionnaire showed a sensitivity 0.567 and a specificity of 0.550 in patients that have contact lens induced dry eye.[25]
Survey available on page 4452 of “Measurement of Ocular Surface Irritation on a Linear Interval Scale with the Ocular Comfort Index”, however, no permission is available for use.
Symptom Assessment In Dry Eye (SANDE)
The SANDE questionnaire was developed by Schaumberg et al. and has two questions presented in visual analog scale. The two questions assess the frequency and severity of dry eye syndrome. The first and second versions of the questionnaire assess the patient’s symptoms two months apart. The questionnaire showed a good test reliability (ICC 0.53-0.76) when repeated assessments were done in a few days, suggesting that it could be useful in detecting changes in symptoms over time.[26]
Survey available on page 857 of “Correlations Among Symptoms, Signs, and Clinical Tests in Evaporative-Type Dry Eye Disease Caused by Meibomian Gland Dysfunction (MGD).” The fee to use this questionnaire is $315.[27] [11]
Schein Questionnaire
Developed by Schein et al. this questionnaire was used for an epidemiologic study to examine the distribution of dry eye in a population of Salisbury, Maryland older than 65 years old.[28] The questionnaire consisted of questions relating to six symptoms and their frequency. The questionnaire results were not well validated, with little correlation between the symptom score of the questionnaire and different clinical tests such as Schirmer test, Rose Bengal stain, as well as sociodemographic characteristics such as race, age, and sex.[29]
Survey available on page 1396 of “Relation between Signs and Symptoms of Dry Eye in the Elderly. A Population-Based Perspective”, however, no permission is available for use.[28][12]
Texas Eye Research and Technology Center Dry Eye Questionnaire (TERTC-DEQ)
This questionnaire was developed by the Texas Eye Research and Technology Center in order to identify moderate dry eye symptoms in patients that do not wear contact lenses.[30] The questionnaire has 28 items that were developed from the Dry Eye Questionnaire, that include symptoms, demographics, medications, and effect on daily living. Patients with a score above 32.3 had moderate dry eye while those below the threshold were considered healthy patients (sensitivity = 0.75 and specificity = 1.00).[13] Moderate concurrent validity with McMonnies (Spearman correlation coefficient = 0.507 [P = 0.003]) was shown.[13][30]
Survey available in the Appendix of “The Diagnosis and Characteristics of Moderate Dry Eye in Non-Contact Lens Wearers.” The fee to use this questionnaire is $374.73
Women’s Health Study Questionnaire
This questionnaire was developed by Schaumberg et al. to describe the magnitude of dry eye syndrome among women in the U.S.[31] This tool is easy to use in epidemiologic studies as well as for clinical research.[32] There are only 3 items in the questionnaire that are used to gauge the frequency of dryness, and symptoms of irritation as well as past history of dry eye syndrome that was diagnosed clinically.[31] The sensitivity and specificity of the questionnaire are 0.77 and 0.83 respectively when compared to clinical confirmation of dry eye syndrome.[32]
Survey available on page 2115 of “Hormone Replacement Therapy and Dry Eye Syndrome.” The fee to use this survey is $600.
References
- ↑ Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo C, Stapleton F. TFOS DEWS II Definition and Classification Report. The Ocular Surface. 2017;15(3):276-283.
- ↑ Nichols KK, Mitchell GL, Zadnik K. Performance and Repeatability of the NEI-VFQ-25 in Patients With Dry Eye. Cornea. 2002;21(6):578-583.
- ↑ Jump up to: 3.0 3.1 3.2 3.3 3.4 3.5 Mangione CM. Development of the 25-list-item National Eye Institute Visual Function Questionnaire. Archives of Ophthalmology. 2001;119(7):1050-1058.
- ↑ Vitale S, Goodman LA, Reed GF, Smith JA. Comparison of the NEI-VFQ and OSDI questionnaires in patients with Sjögren's syndrome-related dry eye. Health and Quality of Life Outcomes. 2004;2(1):44.
- ↑ Jump up to: 5.0 5.1 Schiffman RM. Reliability and Validity of the Ocular Surface Disease Index. Archives of Ophthalmology. 2000;118(5):615-621.
- ↑ Jump up to: 6.0 6.1 Bottomley A, Jones D, Claassens L. Patient-reported outcomes: Assessment and current perspectives of the guidelines of the Food and Drug Administration and the reflection paper of the European Medicines Agency. European Journal of Cancer. 2009;45(3):347-353.
- ↑ Jump up to: 7.0 7.1 Grubbs JR, Tolleson-Rinehart S, Huynh K, Davis RM. A Review of Quality of Life Measures in Dry Eye Questionnaires. Cornea. 2014;33(2):215-218.
- ↑ Özcura F, Aydin S, Helvaci MR. Ocular Surface Disease Index for the Diagnosis of Dry Eye Syndrome. Ocular Immunology and Inflammation. 2007;15(5):389-393.
- ↑ Blackie C, Albou-Ganem C, Korb D. Questionnaire assists in dry eye disease diagnosis. Four-question survey helps evaluate patients’ dry eye symptoms to improve screening. Ocular Surgery News Europe Edition. 2012.
- ↑ Asiedu K. Rasch Analysis of the Standard Patient Evaluation of Eye Dryness Questionnaire. Eye & Contact Lens: Science & Clinical Practice. 2017;43(6):394-398.
- ↑ Jump up to: 11.0 11.1 11.2 11.3 Ngo W, Situ P, Keir N, Korb D, Blackie C, Simpson T. Psychometric properties and validation of the Standard Patient Evaluation of Eye Dryness questionnaire. Cornea. 2013;32(9):1204-1210.
- ↑ Jump up to: 12.0 12.1 Doughty MJ, Fonn D, Richter D, Simpson T, Caffery B, Gordon K. A Patient Questionnaire Approach to Estimating the Prevalence of Dry Eye Symptoms in Patients Presenting to Optometric Practices across Canada. Optometry and Vision Science. 1997;74(8):624-31.
- ↑ Jump up to: 13.0 13.1 13.2 13.3 Guillemin I, Begley C, Chalmers R, Baudouin C, Arnould B. Appraisal of Patient-Reported Outcome Instruments Available for Randomized Clinical Trials in Dry Eye: Revisiting the Standards. The Ocular Surface. 2012;10(2):84-99.
- ↑ Jump up to: 14.0 14.1 14.2 14.3 Oden NL, Lilienfeld DE, Lemp MA, Nelson JD, Ederer F. Sensitivity and Specificity of a Screening Questionnaire for Dry Eye. Lacrimal Gland, Tear Film, and Dry Eye Syndromes 2 Advances in Experimental Medicine and Biology. 1998;438:807-820.
- ↑ Chalmers RL, Begley CG, Caffery B. Validation of the 5-Item Dry Eye Questionnaire (DEQ-5): Discrimination across self-assessed severity and aqueous tear deficient dry eye diagnoses. Contact Lens and Anterior Eye. 2010;33(2):55-60.
- ↑ Begley CG, Caffery B, Chalmers RL, Mitchell GL. Use of the Dry Eye Questionnaire to Measure Symptoms of Ocular Irritation in Patients With Aqueous Tear Deficient Dry Eye. Cornea. 2002;21(7):664-670.
- ↑ Simpson TL, Situ P, Jones LW, Fonn D. Dry Eye Symptoms Assessed by Four Questionnaires. Optometry and Vision Science. 2008;85(8):692-9.
- ↑ Begley CG, Caffery B, Nichols KK, Chalmers R. Responses of Contact Lens Wearers to a Dry Eye Survey. Optometry and Vision Science. 2000;77(1):40–6.
- ↑ Jump up to: 19.0 19.1 Nichols JJ, Mithcell GL, Nichols KK, Chalmers R, Begley C. The performance of the contact lens dry eye questionnaire as a screen survey for contact lens-related dry eye. Cornea. 2002;21:469-475.
- ↑ Jump up to: 20.0 20.1 20.2 20.3 Abetz L, Rajagopalan K, Mertzanis P, Begley C, Barnes R, Chalmers R. Development and validation of the impact of dry eye on everyday life (IDEEL) questionnaire, a patient-reported outcomes (PRO) measure for the assessment of the burden of dry eye on patients. Health and Quality of Life Outcomes. 2011;9(1):111.
- ↑ Jump up to: 21.0 21.1 21.2 McCarty CA, Bansal AK, Livingston PM, Stanislavsky YL, Taylor HR. The Epidemiology of Dry Eye in Melbourne, Australia. Ophthalmology. 1998;105(6): 1114-119.
- ↑ Jump up to: 22.0 22.1 22.2 Nichols KK, Nichols JJ, Mitchell GL. The Reliability and Validity of McMonnies Dry Eye Index. Cornea. 2004;23(4):365-71.
- ↑ Tang, F., Wang, J., Tang, Z., Kang, M., Deng, Q., & Yu, J. (2016). Accuracy of McMonnies Questionnaire as a Screening Tool for Chinese Ophthalmic Outpatients. Plos One, 11(4).
- ↑ Jump up to: 24.0 24.1 Johnson ME, Murphy PJ. Measurement of Ocular Surface Irritation on a Linear Interval Scale with the Ocular Comfort Index. Investigative Ophthalmology & Visual Science. 2007;48(10):4451.
- ↑ Michel M, Sickenberger W, Pult H. The effectiveness of questionnaires in the determination of Contact Lens Induced Dry Eye. Ophthalmic and Physiological Optics. 2009;29(5):479-486.
- ↑ Schaumberg DA, Gulati A, Mathers WD, Clinch T, Lemp MA, Nelson JD, Foulks GN, Dana R. Development and Validation of a Short Global Dry Eye Symptom Index. The Ocular Surface. 2007;5(1):50-57.
- ↑ Cuevas M, Gonzalez-Garcia M, Castellanos E, Quispaya R, Parra L, Fernandez I, Calonge M. Correlations Among Symptoms, Signs, and Clinical Tests in Evaporative-Type Dry Eye Disease Caused by Meibomian Gland Dysfunction (MGD). Current Eye Research. 2012; 37(10):855–863.
- ↑ Jump up to: 28.0 28.1 Schein OD, Tielsch JM, Muñoz B, Bandeen-Roche K, West S. Relation between Signs and Symptoms of Dry Eye in the Elderly. A population-based perspective. Ophthalmology. 1997;104(9):1395-1401.
- ↑ Bandeen-Roche K, Muñoz B, Tielsch JM, West SK, Schein OD. Self-reported assessment of dry eye in a population-based setting. Invest Ophthalmol Vis Sci. 1997;38:2469-2475.
- ↑ Jump up to: 30.0 30.1 Narayanan S, Miller WL, Prager TC, Jackson JA, Leach NE, Mcdermott AM, Christensen MT, Bergmanson JP. The Diagnosis and Characteristics of Moderate Dry Eye in Non-Contact Lens Wearers. Eye & Contact Lens: Science & Clinical Practice. 2005;31(3):96-104.
- ↑ Jump up to: 31.0 31.1 Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. American Journal of Ophthalmology. 2003;136(2):318-326.
- ↑ Jump up to: 32.0 32.1 Gulati A, Sullivan R, Buring JE, Sullivan DA, Dana R, Schaumberg DA. Validation and Repeatability of a Short Questionnaire for Dry Eye Syndrome. American Journal of Ophthalmology. 2006;142(1):125-131.

