Crossed Quadrant Homonymous Hemianopsia
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
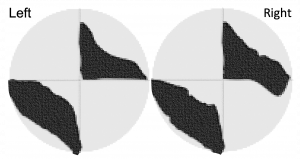
Crossed-quadrant homonymous hemianopsia is also known as the "checkerboard visual field deficit". According to Cross et al., [1], from 1891-1982 there were only 9 reported cases of this deficit documented in the medical literature. As of 2020, there are newer reports associated to Multiple Sclerosis[2][3], Viper bite[4], with different presentations[5]. In this classic deficit, one lesion occurs above the calcarine fissure and one below on the opposite side [6][7]. The defects usually extend across the horizontal median but always respect the vertical median. [8]
Disease
Crossed-quadrant homonymous hemianopsia is the homonymous loss of two opposite quadrants of the visual field which is a rare occurrence. Cases of crossed-quadrant homonymous hemianopsia are rare. Visual loss may be sudden or gradual. Visual fields may be affected either simultaneously or in succession, with the former being the most common. It is likely that cerebral infarctions derive principally by embolization of the calcarine arteries from basilar or vertebral branches.
Risk Factors
- Hypertension
- Atherosclerosis
- Prior stroke
- Tertiary syphilis
- Coronary artery disease
- Multiple Sclerosis
- Trauma
Pathophysiology
Cases of CQHH can occur after two simultaneous events or two separate events.
This disease process can be due to trauma, bilateral multiple sclerosis lesions, cerebral infarcts or viper bite. Most of the cerebral infarcts are derived principally by embolization of the calcarine arteries from basilar or vertebral branches. There has been one documented case of CQHH from the University of Rome, Institute of Ophthalmology from 1995 in a patient with multiple sclerosis[2].
Primary Prevention
Primary prevention includes decreasing risk factors for stroke.
Diagnosis
The most frequent cause is embolization of the calcarine arteries (from basilar or vertebral branches) or from thromboembolism from cardiac disease [9].
Most of the cases are related to ischemic or hemorrhagic stroke, associated to spontaneous thromboembolism, cervical-vertebral trauma, vessel dissection and one case of viper bite.
The entity may occur in monocular patients with a corresponding superior and contralateral inferior quadrantanopia secondary to occipital stroke, that can be otherwise asymptomatic. Therefore high suspicion with a automated perimetry check (30-2) is recommended [10]
History
The first documented case was by Groenouw in 1891 in the Archiv fur Psychiatrie. Groenouw's patient first had a left hemiplegia and a left homonymous hemianopsia. Ten months later, he suffered a second stroke and then it was noted he had developed a crossed quadrant hemianopsia[8].
The first case of a patient solely complaining of eye symptoms was reported in the British Journal of Ophthalmology in 1926. The authors noted that this sign can only be explained by "a sudden affection of both hemispheres of the brain." He also reported that the visual path must be "of course behind the chiasma; therefore in the optic tract, the primary optic ganglia, the optic radiation or cortical centre of vision"[8].
Clinical Diagnosis
Characteristics of visual field defects: [9][8] [11]
- The defects may arise in
- two simultaneous quandrantanopsias
- two successive homonymous hemianopsia, each resolving into a quadrantanopsia
- simultaneous bilateral homonymous hemianopsia resolving into crossed quadrant defects
- The defects usually extend across the horizontal midline but respect the vertical midline
- There may be sparing of the monocular temporal crescent
- Central vision is usually preserved
- The intact quadrants may demonstrate small areas of field loss
- Color vision may be abnormal
- Riddoch phenomenon may be present which accounts for apparent incongruity of field testing
- Simple or complex visual hallucinations may appear in the blind or seeing field
Diagnostic procedures
- Humphrey Visual Field (the automated visual field is rarely completely symmetric)
- Goldmann Visual Field
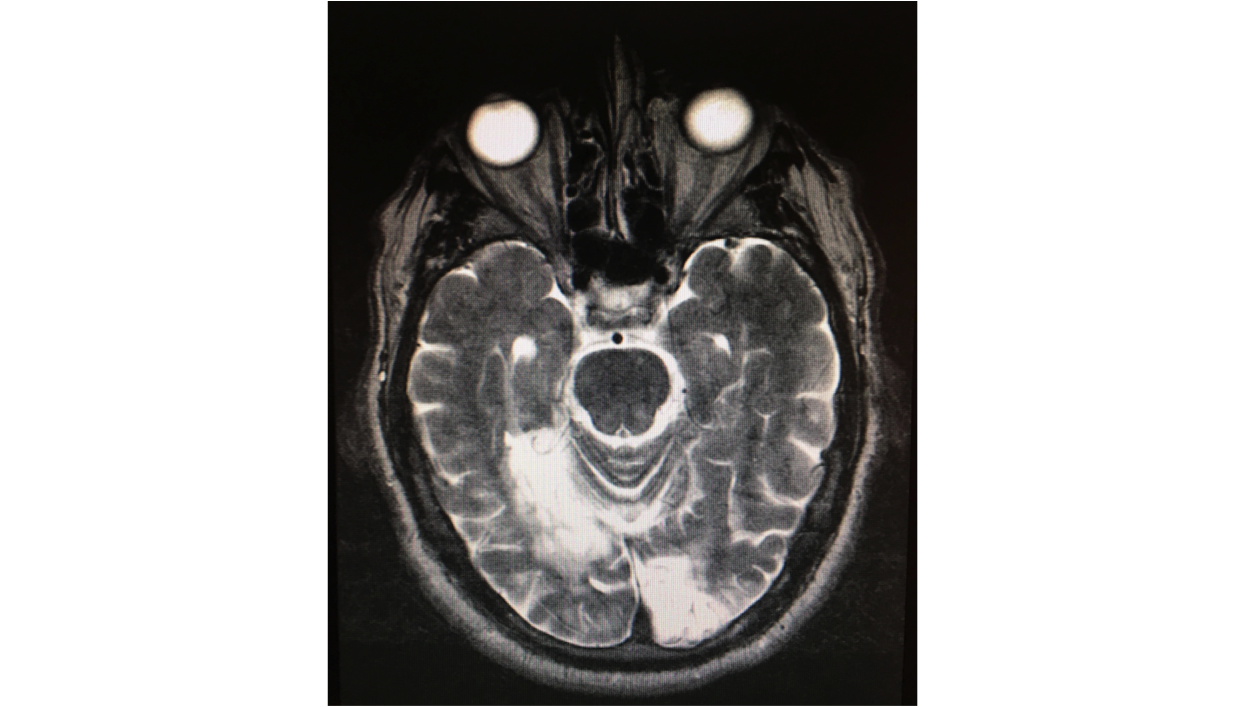
- CT scan
- Magnetic resonance imaging
Differential diagnosis
- Stroke
- Tumor
- Trauma
- Migraine
- Inflammatory Process
- Demyelinating Process
Management
It is recommended that the patient have a consult with Neurology in order to start treatment with appropriate anti-platelet therapy. The underlying etiology is mostly associated with vertebrobasilar disease or posterior cerebral ischemia from the original cervical spine injury. Most patients need to establish care with visual rehabilitation as well as low vision services.
Multidisciplinary approach by neurology, ophthalmology, neuro-radiology and neurosurgeon if there is a tumor related etiology.
General treatment
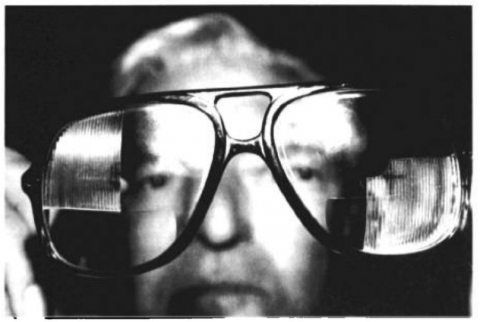
Some studies have recommended "checkerboard prisms." The goals of prisms are to expand the intact visual field. Images that normally fall on the hemianopic retina are shifted so they become visible by the seeing portion of the retina. The use of these prisms has been reported with varying degrees of success. "[1]
Complications
Cortical blindness can lead to Anton syndrome which is detail of blindness by the patient. This is usually seen with infarcts where the posterior cerebral artery is concerned and involve the primary visual cortex and association area.
Riddoch syndrome (or Statokinetic dissociation[12]) has been seen in these patients as well. This phenomenon occurs when patients who have occipital lobe lesions in the striate cortex respond to visual stimuli that they do not consciously see in their visual field. These patients notice moving objects in a blind field.
Prognosis
The patient is unlikely to gain vision after this event. The goal is to help the patient adapt to this visual field loss and prevent further strokes by decreasing risk factors and taking appropriate anti-platelet therapy.
Resources
Explanation on Homonymous Hemianopia, video resource NANOS. https://youtu.be/XietRxh6UWE
References
- ↑ 1.0 1.1 Cross SA, Smith JL. Crossed-quadrant homonymous hemianopsia. The “checkerboard” field defect. J Clin Neurol Ophthalmol. 1982;2:149–158
- ↑ 2.0 2.1 Cesareo M, Pozzilli C, Ristori G, et al., Crossed quadrant homonymous hemianopsia in a case multiple sclerosis. Clin Neurol Neurosurg.1995;97:324–327
- ↑ Tamhankar MA, Markowitz CE, Galetta SL. Checkerboard fields in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2005;76:268
- ↑ Mahale R, Mehta A, Javali M, Srinivasa R. A case of bilateral occipital lobe infarcts following Indian tree viper bite. J Stroke. 2014;16(3):205-207.doi:10.5853/jos.2014.16.3.205
- ↑ Kamal S, Al Othman BA, Kini AT, Lee AG. Checkerboard Visual Field Defect in Occipital Stroke. J Neuroophthalmol. 2020;40(2):e13-e14.doi:10.1097/WNO.0000000000000892
- ↑ American Academy of Ophthalmology. Neuro-Ophthalmology Section 5. Basic and clinical science course, AAO 2016-2017
- ↑ Fong JW, Ly VV, Braswell RA. Crossed-quadrant homonymous hemianopsia in a monocular patient. Published:March 02, 2021DOI:https://doi.org/10.1016/j.jcjo.2021.02.004
- ↑ 8.0 8.1 8.2 8.3 Felix ch. Crossed quadrant hemianopsia. Br j ophthalmol. 1926;10(4):191-195. Doi:10.1136/bjo.10.4.191
- ↑ 9.0 9.1 Dyer JA, Hirst LW, Vandeleur K, Carey T, Mann PR. Crossed-quadrant homonymous hemianopsia. J Clin Neuroophthalmol. 1990;10(3):219-222.
- ↑ Fong JW, Ly VV, Braswell RA. Crossed-quadrant homonymous hemianopsia in a monocular patient. Can J Ophthalmol. 2021 Mar 3:S0008-4182(21)00041-7. doi: 10.1016/j.jcjo.2021.02.004. Epub ahead of print. PMID: 33667430
- ↑ Schiller J, Dietrich TJ, Lorch L et al., Homonymous visual field defects: Perimetric findings and corresponding neuro-imaging results. Proceedings of the XIIIth International Perimetric Society Meeting, Perimetry Update 1998/1999, Kugler Publications, p511–516.
- ↑ Hayashi R, Yamaguchi S, Narimatsu T, Miyata H, Katsumata Y, Mimura M. Statokinetic Dissociation (Riddoch Phenomenon) in a Patient with Homonymous Hemianopsia as the First Sign of Posterior Cortical Atrophy. Case Rep Neurol. 2017;9(3):256-260. Published 2017 Nov 10. doi:10.1159/000481304