All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Corneal inlays
Corneal inlays, also called keratophakia, are implants placed in the corneal stroma for correction of presbyopia, a condition in which the ability to accommodate or focus at near objects is decreased.
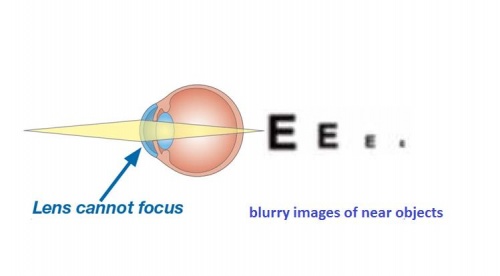
Accommodation and presbyopia
Generally, people under the age of 40 can focus easily both at distance and near. Near objects can be seen clearly due to contraction of the ciliary muscle and the resulting increase in the curvature of the anterior surface of the lens, a process called accommodation. Accommodation starts decreasing after the age of 40, making it difficult to see intermediate and near objects. Wearing reading glasses is the common solution to presbyopia.
Corneal inlays are one of the options for correction of decreased near vision in presbyopic people who desire spectacle-independence at all distances. They do not restore the ability to accommodate, as they have no effect on the ciliary muscle or the lens. They work by increasing the depth of focus or the refractive power of the central or paracentral cornea. Corneal inlays have also been used for correction of hyperopia, myopia, and astigmatism.
History of corneal inlays
Corneal inlays have been studied over the past 40 years. In 1949, Barraquer introduced the idea of corneal implants to change the corneal refraction.[1] He used corneal implants made of donor corneal tissue shaped by a cryolathe. He later tried using synthetic implants like Plexiglas. Various materials like PMMA, polysulfone, polypropylene and silicone oil were also tried in 1950s and 1960s. However, these materials were associated with stromal necrosis and extrusion of the implant.[2]
In 1961, Knowles found that water impermeable implants prevent flow of water and nutrients through the cornea, resulting in stromal thinning, and epithelial and stromal breakdown.[3] Therefore, it was necessary to make inlays using a permeable material in order to maintain normal corneal physiology.
Later, hydrogel inlays were found to be permeable to water and solutes, due to the hydrophilic polymers and large pore size. In 1967, Dohlman found that discs made of glycerin methacrylate hydrogel with 88 % water were compatible with corneas in rabbits and cats. However, over time, these discs opacified due to impregnation with proteins, and some corneas underwent necrosis due to the thickness of discs.[4] Over the years, hydrogels underwent more development. Weblin et al demonstrated the viability of improvised hydrogel inlays in non-human primates based on the presence of corneal clarity, normal appearing endothelium, intact epithelium, and the lack of inflammation, necrosis, and vascularization.[5] McDonald et al found that high water content hydrogel inlays were well tolerated in primates for up to 5 years.[6]
There continues to be further modification and improvement in the design of inlays to achieve better tolerance in the human cornea. The major changes include decrease in thickness, use of more biocompatible material, incorporation of multiple holes to allow passage of nutrients, and optimization of depth of placement in the cornea.
Types and Designs
Currently there are three types of corneal inlays which differ in their design, size, material and mechanism of action.
1.Refractive corneal inlays
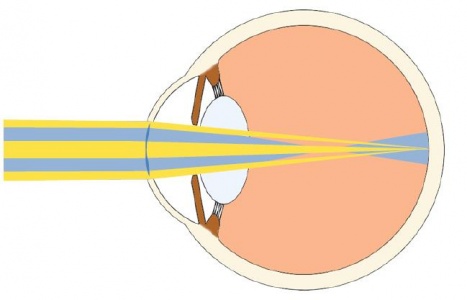
These disc shaped corneal implants work by changing the refractive index of the cornea. The central zone of the implant is neutral or plano, and has no refractive power. It allows light rays from distant source to focus on the retina, preserving distance vision. The central neutral zone is surrounded by one circular zone of additional positive power, which focus light rays from near objects on the retina, and improve near vision. Their design is similar to multifocal contact lens or intraocular lens.
The Presbia Flexivue MicrolensTM (Presbia, Irvine, California, USA)is a transparent hydrogel implant (made of hydroxyethyl methacrylate and methyl methacrylate) with a diameter of 3 mm.It has a central plano zone, surrounded by multiple rings of progressively increasing powers from +1.50 to +3.50 D, creating a multifocal effect. The lens is 15-20 micronsthick from the center to its periphery. It is placed in a stromal pocket at a depth of three fifth of the corneal thickness. This is believed to be the optimal depth for nutrient flow.[7] At present, it is in FDA trials in the US.
The Icolens (Neoptics AG, Hunenberg, Switzerland) is commercially available outside the United States.
2. Corneal reshaping inlays
These corneal implants are designed to change the curvature of the anterior corneal surface. They are placed anteriorly in the cornea, either under a 130-150 microns flap, or in a stromal pocket, to create a hyperprolate anterior corneal surface. They correct presbyopia by increasing the curvature of the central part of the anterior corneal surface. Paracentral light rays ,travel through the thinner portion of the inlay and enable viewing distant objects while near objects can be viewed clearly through the central curved part of the cornea.
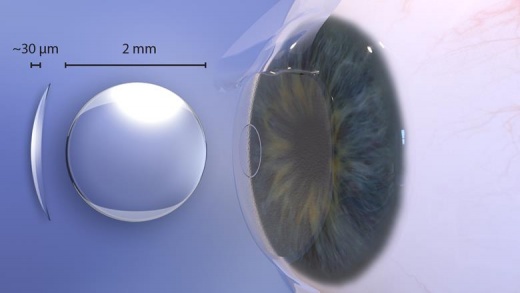
The Raindrop Near Vision Inlay,formerly known as the PresbyLens or Vue+ lens(ReVision Optics, Lake Forest, California, USA) is a thin transparent permeable hydrogel implant. It is 1.5-2mm in diameter and varies in thickness from 10 microns in the periphery to 32 microns in the center. Its refractive index and water content are similar to those of the cornea. It has no additional refractive power. Being permeable, it allows transmission of nutrients through it. The device was FDA approved in 2016; however, it was recalled in October of 2018 secondary to post-operative corneal haze.
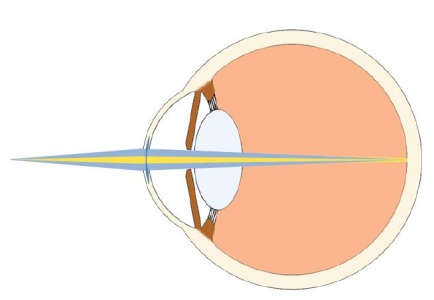
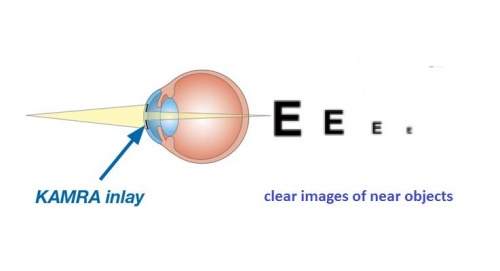
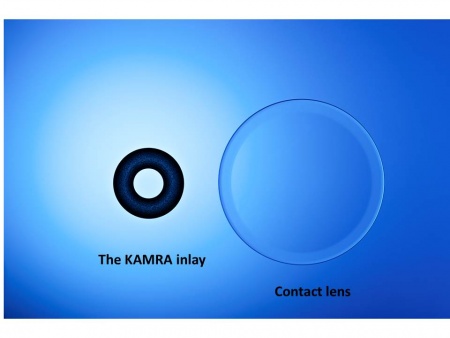
3. Small aperture inlays
These inlays are opaque, ring shaped with a central aperture. Based on the principle of pinhole optics, they improve near vision by increasing the depth of focus. The ring blocks the peripheral light rays and allows only the central rays to pass unhindered.
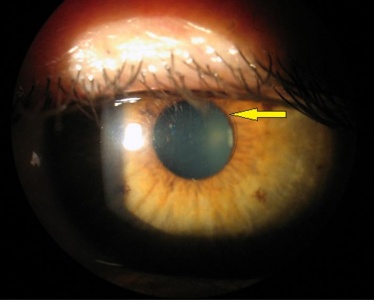
The Kamra Inlay (AcuFocus, Inc., Irvine, California, USA), previously known as ACI 7000, is an opaque ring shaped inlay made of polyvinylidene fluoride and carbon. It is 5 microns thick with an outer 3.8 mm diameter and a central 1.6 mm aperture. The ring has 8400 laser etched holes to facilitate diffusion of aqueous, oxygen and nutrients through the cornea. It is commercially available in the United States, Europe, Asia-Pacific, South America, and the Middle-East.
Currently under study
LinkoCare inlay is a presbyopic inlay made of biosynthetic collagen. The surgery aims at correcting presbyopia by increasing the refractive power of the non dominant eye for reading vision. The inlay is implanted to make the cornea steeper in the center. The increase in thickness is 15 µm and creates a keratometry increase of 3.3 D, reports Pavel Stodulka, MD, PhD.[8] The biosynthetic collagen should offer the advantage of an excellent biocompatibility.
Patient selection
Early and mid presbyopic people between the age of 40 and 60 years are ideal for the surgery. The inlays are implanted in presbyopic emmetropic eyes, but can also be used in eyes with myopia, hyperopia and astigmatism as a combined procedure with LASIK.[9] Patients who have had the LASIK procedure can also be implanted with the inlays. Patients should be free of ocular surface disease. Dry eyes and blepharitis should be managed optimally before considering the surgery. Patients with uncontrolled dry eyes, and blepharitis should not be implanted with the inlays. Topography should be performed to screen for corneal ectatic disorders like keratoconus, which is a contraindication for inlays. Patients having central cataracts should not be implanted with inlays. Pachymetry should be done to ensure adequate corneal thickness, to allow placement of the the Kamra and the Presbia Flexivue iMicrolens implants at a depth of 200-300 microns. The raindrop inlay, however, is placed relatively superficially at a depth of 120-150 microns.
Technique
Procedure
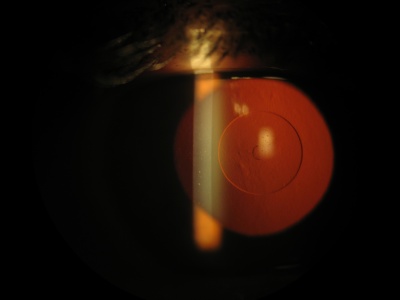
The procedure is done under topical anesthesia. Corneal inlays are usually implanted monocularly in the non-dominant eye. They can be inserted in stromal pockets or under flaps, similar to LASIK flaps. The flaps and pockets are more commonly created with a femtosecond laser, but flaps can still be created with a microkeratome. The flap is made similar to a LASIK flap. The stromal pocket is shaped like a keyhole. When using a femtosecond laser, the pocket is fashioned using either special software (available in some femtosecond lasers) for creation of pocket, or a mask with a keyhole opening on the applanation cone. After creating the flap or the pocket, the inlay is placed on the stromal bed. Special instruments are used for handling the inlay. Proper centration is important for best results. The center is identified by marking the first Purkinje reflection, or the co-axially sighted corneal reflex, or more accurately with devices like the OPD scan (Nidek) and the AcuTarget system (Acufocus). In patients with significant angle kappa the Kamra inlay should be placed halfway between the corneal vertex and the center of the entrance pupil. [10] The depth of placement depends on the design of the inlay. Inlays like the Raindrop which change the corneal curvature were placed relatively superficially, at a depth of 120-150 microns, while inlays with a central aperture, and those that change refractive index are placed deeper in the cornea, at 200-300 microns. The placement of inlays can be combined with LASIK for correction of ametropia either as a simultaneous or a two staged procedure.
Advantages of placing inlays in a stromal pocket are stable centration, minimal damage to corneal nerves, preservation of corneal sensation, maintenance of peripheral biomechanical stability, and minimal striae. [11]
Advantages of placing inlays under a flap include the ability to combine it with Excimer laser ablation of stromal bed for simultaneous correction of myopia, hyperopia, or astigmatism along with presbyopia. It also allows removal or repositioning if necessary, at a later date.[11]
Post-operative management
Antibiotic drops are administered for a week, while steroid drops are administered with a tapering course over a period of 1 month, to minimize interface wound healing, haze formation, and opacification, as well as to avoid refractive shifts.
Advantages
- Good vision at near, intermediate and far distance. Studies have shown that most patients achieve uncorrected near visual acuity close to J1 or J2, with modest effect on distant visual acuity.[11][12][13][14][15][16] Near vision improves, with a possible 1-2 line trade off with distance vision in the treated eye. However, the dominant eye continues to have good distance vision in an emmetropic patient. Also, binocular vision at all distances is excellent. Vision at intermediate distance is better than that achieved with multifocal intraocular lenses.
- Safety: Since the surgery is limited to the cornea, the risk profile is different than intraocular surgeries for correction of presbyopia, like phakic IOLs (intraocular lens implanted in the eye over the natural lens), clear lens or cataract extraction with multifocal IOL insertion. It is also has a different risk profile than LASIK as it does not remove any corneal tissue, thus minimizing the risk of ectasia.
- Reversibility. The inlay can be explanted if the patient is dissatisfied.
- Combination with other refractive surgeries. Corneal inlay procedures can be done simultaneously with, or following LASIK and PRK to treat ametropia and presbyopia. It can also be performed in patients who have undergone cataract surgery with monofocal lens or phakic IOL implantation.
- Examination and imaging: The transparent Presbia Flexivue Microlens TM and Raindrop inlays as well as the ring shaped opaque Kamra inlay do not affect examination and imaging of ocular structures. [14][17]
Side effects
- Halos, glare and disturbances in night vision.
- Loss of contrast sensitivity: This is also due to reduction in light entering the eye.
- Difficulty in reading in dim light. The aperture design inlays reduce the amount of light entering the eye. This effect is more noticeable in dim lighting, making reading difficult.
- Effect of pupil size. Pupil size may affect vision in case of refractive inlays. In small pupils, most of the pupillary area is occupied by the inlay, making distance vision difficult. Conversely, in larger pupils, only a small part of the pupillary area is covered by the inlay making near vision blurry.
- Corneal haze. This may develop after implantation of the Raindrop inlay. It generally resolves spontaneously, or following a course of topical steroids.
- Prolonged visual recovery if combined with LASIK.
- Dry eye is more common and more severe than with femto LASIK. This is probably caused by the depth of the flap (200 microns with the pinhole inlay).
Complications
- Lens decentration. This can occur in the early post-operative period due to inadequate flap adhesion. Decentration degrades the quality of vision and specially affects distance vision. This can be corrected by accessing the inlay in the stromal pocket and repositioning.[19]
- Dry eyes: This can occur due to damage to the corneal nerves during flap creation, as in the LASIK procedure.
- Keratolysis, vascularization and opacification. These complications were more common with older inlay designs which were thicker, less biocompatible and had low water content. Anterior placement or non-porous implants affected the movement and diffusion of aqueous, oxygen, glucose and other nutrients to the anterior portion of the cornea, resulting in necrosis and tissue breakdown. However, today these complications are rare with the thinner profile, small diameter, higher permeability and better biocompatibility of inlays.
- Epithelial ingrowth. Epithelial cells may accidently get implanted in the interface and grow around the corneal implant. The ingrowth opacifies the interface and may cause blurry vision, photophobia and star bursts.[20]
- Central corneal flattening and hyperopic shift. It might be associated with haze formation on top of the pinhole inlay. It's usually reversed by one or two courses of topical steroids treatment.

Additional Resources
- Mukamal R, Lee WB, Boyd K. Corneal Inlays. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/treatments/corneal-inlays. Accessed March 07, 2019.
References
- ↑ Barraquer J I. Modification of refraction by means of intracorneal inclusions. Int Ophthalmol Clin. 1966; 6(1):53–78.
- ↑ Lane SL, Lindstrom RL, Cameron JD, Thomas RH, Mindrup EA, Waring GO 3rd, McCarey BE, Binder PS. Polysulfone corneal lenses. J Cataract Refract Surg. 1986 Jan;12(1):50-60.
- ↑ Knowles W F. Effect of intralamellar plastic membranes on corneal physiology. Am J Ophthalmol.1961;51:1146-1156.
- ↑ Dohlman C H,RefojoMF,RoseJ.Synthetic polymers in corneal .surgery.I.Glycerylmethacrylate. ArchOphthalmol. 1967;77(2):252-257.
- ↑ WerblinT P, Peiffer R L,Binder P S, McCarey B E, Patel A S. Eight years experience with Permalens intracorneal lenses in nonhuman primates.Refract Corneal Surg.1992;8(1):12-22.
- ↑ McDonald M B,McCarey B E,Storie B,et al. Assessment of the long-term corneal response to hydrogel intrastromal lenses implanted in monkey eyes for up to five years. J. Cataract Refract Surg. 1993;19(3):213- 222
- ↑ Larrea X, De Courten C, Feingold V, Burger J, Büchler P. Optom Vis Sci. 2007 Dec; 84(12):1074-81. Oxygen and glucose distribution after intracorneal lens implantation.
- ↑ https://www.healio.com/news/ophthalmology/20200313/bioengineered-corneal-inlay-overcomes-biocompatibility-problems-of-past-technologies
- ↑ Tomita M, Kanamori T, Waring G O IV, et al. Simultaneous corneal inlay implantation and laser in situ keratomileusis for presbyopia in patients with hyperopia, myopia or emmetropia: Six-month results. J Cataract Refract Surg. 2012;38(3):495-506.
- ↑ Gatinel D, El Danasoury A, Rajchles S, Saad A. Recentration of a small aperture corneal inlay. J Cataract Refract Surg 2012; 38:2186–2191.
- ↑ 11.0 11.1 11.2 10.Waring G O IV, Klyce S D. Corneal inlays for the treatment of presbyopia. Int Ophthalmol Clin 2011;51(2):51-62.
- ↑ Yilmaz O F, Alagoz N, Pekel G, et al. Intracorneal inlay to correct presbyopia: Long-term results. J Cataract Refract Surg2011;37(7):1275-1281.
- ↑ Pallikaris I O, Slade S, Vukich J, Bouzoukis D. Corneal inlays for presbyopia. Presented at the 29th Congress of the ESCRS; September 19, 2011; Vienna, Austria
- ↑ 14.0 14.1 14.2 Seyeddain O, Hohensinn M, Riha W, et al. Small-aperture corneal inlay for thefckLRcorrection of presbyopia: 3-year follow-up. J Cataract Refract Surg 2012;38:35–45.
- ↑ Pallikaris I G. Intracorneal refractive inlays for the treatment of presbyopia: visual outcomes and safety. Paper presented at: American Academy of Ophthalmology annual meeting: Oct 23, 2009: San Francisco, CA.
- ↑ Pallikaris I G.Intracorneal lenses for the treatment of presbyopia using femtosecond laser: visual outcomes and safety. Paper presented at: American academy of Ophthalmology annual meeting: October 17,2010: Chicago, IL.
- ↑ Bouzoukis D I, Kymionis G D, Panagopoulou SI, et al. Visual outcomes and safety of a small diameter intrastromal refractive inlay for the corneal compensation of presbyopia. J Refract Surg 2012; 28:168–173.
- ↑ Brooker E T, Waring G O IV, Vilupuru A S, Sanchez Leon F. Effect of small aperture intra-corneal inlay on visual fields. Invest Ophthalmol Vis Sci 2012;53:abstract 1391.
- ↑ Hoopes Jr., P, Walker B., Birdsong, OC., Moshirfar M. Small-aperture corneal inlay repositioning. J Cataract Ref Surg. 2018. Vol 44. (1) pg 3-5
- ↑ 18.Jorge L. Alió, MD, PhD; M. Emilia Mulet, MD, PhD; Luis F. Zapata, MD; M. Teresa Vidal, MD, PhD; Victoria De Rojas, MD, PhD; Jaime Javaloy, MD, PhD. Intracorneal Inlay Complicated by Intrastromal Epithelial Opacification. Arch Ophthalmol. 2004;122(10):1441-1446. doi:10.1001/archopht.122.10.1441