Content Template Example
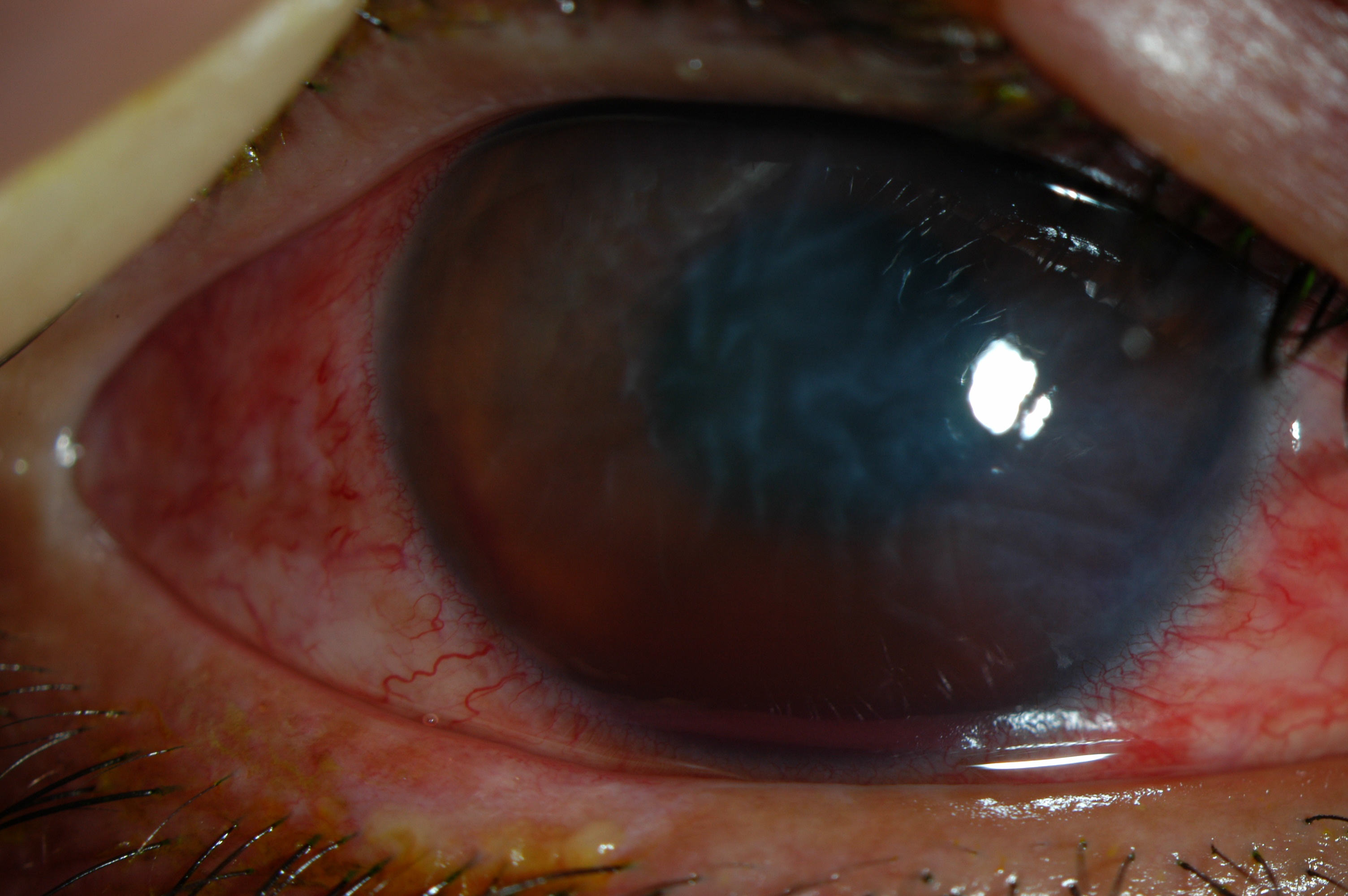
A cataract is a clouding of the lens in the eye that affects vision. The lens is a clear part of the eye that helps to focus light, or an image, on the retina. The retina is the light-sensitive tissue at the back of the eye. In a normal eye, light passes through the transparent lens to the retina. Once it reaches the retina, light is changed into nerve signals that are sent to the brain. The lens must be clear for the retina to receive a sharp image. If the lens is cloudy from a cataract, the image that is seen will be blurred.
Disease Entity
Section: Cataract/Anterior Segment
A cataract in the adult eye (ICD-9 #366.1).
Disease
A cataract is a degradation of the optical quality of the crystalline lens.
Etiology
Cataracts are usually a result of denaturation of lens protein.
Risk Factors
Cataracts develop for a variety of reasons, including long-term exposure to ultraviolet light, exposure to radiation, secondary effects of diseases such as diabetes, hypertension and advanced age, or trauma (possibly much earlier).[1] Genetic factors are often a cause of congenital cataracts and positive family history may also play a role in predisposing someone to cataracts at an earlier age.Cataracts may also be produced by eye injury or physical trauma.
General Pathology
Add text here
Pathophysiology
Add text here
Primary Prevention
Add text here
Diagnosis
The purpose of the comprehensive evaluation of a patient whose chief complaint might be related to a cataract is to determine the presence of a cataract, confirm that a cataract is a significant factor related to the visual impairment and symptoms described by the patient, and exclude or identify other ocular or systemic conditions that might contribute to visual impairment or affect the cataract surgical plan or ultimate outcome. The comprehensive evaluation (history and physical examination) includes those components of the comprehensive adult medical eye evaluation specifically relevant to the diagnosis and treatment of a cataract as listed below.
History
Patient history,including the patient’s assessment of functional status, pertinent medical conditions, medications currently used, and other risk factors that can affect the surgical plan or outcome of surgery (e.g., immunosuppressive conditions, sympathetic alpha-1a antagonists).
Physical Examination
- Visual acuity with current correction (the power of the present correction recorded) at distance and when appropriate at near.
- Measurement of best-corrected visual acuity (with refraction when indicated).
- External examination (lids, lashes, lacrimal apparatus, orbit).
- Examination of ocular alignment and motility.
- Assessment of pupillary function.
- Measurement of intraocular pressure (IOP).
- Slit-lamp biomicroscopy of the anterior segment.
- Dilated examination of the lens, macula, peripheral retina, optic nerve, and vitreous.
- Assessment of relevant aspects of the patient’s mental and physical status.
Signs
As a cataract becomes more opaque, clear vision is compromised. A loss of visual acuity is noted. Contrast sensitivity is also lost, so that contours, shadows and color vision are less vivid. Veiling glare can be a problem as light is scattered by the cataract into the eye. A contrast sensitivity test should be performed and if a loss in contrast sensitivity is demonstrated an eye specialist consultation is recommended.
Symptoms
A cataract is defined as any opacification of the eye's crystalline lens, and any of these changes that then lead to a degradation in the optical quality of the lens can cause visual symptoms. As there are a wide variety of cataract types, there is a large spectrum of visual symptoms associated with cataractous changes. [2]
Clinical Diagnosis
Add text here
Diagnostic Procedures
Add text here
Laboratory Test
Add text here
Differential Diagnosis
Deep learning models are in development to aid diagnosis and classification of age-related cataract based on anterior segment slit-lamp photographs.[3]
Management
Add text here
General Treatment
Add text here
Medical Therapy
Management of a visually significant cataract is primarily surgical. Nonsurgical management includes counseling patients about cataract-related visual symptoms, providing reassurance about the cause of the visual disability, and prescribing new eyeglasses where appropriate. For some patients with a clinically significant cataract, a change in spectacle correction or use of specialized tints may restore acceptable vision for daily activities. In rare cases, the optical advantage of dilating a pupil of a patient with a small central cataract may outweigh the risk of glare problems that are induced by the dilating agent.
At the present time, the highest quality evidence does not support a benefit from nutritional supplementation in preventing or delaying progression of cataracts; therefore, treatment with supplements is not recommended. Currently, there are no pharmacological treatments known to eliminate existing cataracts or retard their progression.
Patients may reduce their risk of cataract development or progression by modifying their exposure to risk factors. Patients who are currently smoking should be informed of the increased risk of cataract progression and the benefits of smoking cessation in retarding the progression of cataracts that have been demonstrated in several studies.Studies have found that smokers report that a physician’s advice to quit is an important motivator in attempting to stop smoking.Patients who are long-term users of oral or inhaled corticosteroids should be informed of the increased risk of cataract formation and may wish to discuss alternate medications with their primary care physician. Patients with diabetes mellitus should be informed of their increased risk of cataract formation.
Medical Follow-up
Add text here
Surgery
The preferred method to remove a cataract is extracapsular extraction, most commonly by phacoemulsification, which is now used in over 90% of cataract surgeries performed in the United States. The 2005 Leaming Survey highlighted the predominant trend of the small-incision, phacoemulsification technique.198 The findings were that many respondents use topical anesthesia with intracameral lidocaine, clear-corneal incisions, and a no-suture technique.
In a randomized trial of extracapsular cataract extraction (ECCE) and small-incision phacoemulsification, visual acuity following phacoemulsification was significantly better and more stable during the 1-year postoperative follow-up period compared with larger incision non-phaco techniques (ECCE). There were fewer surgical complications in the phacoemulsification group.At 1 year, the incidence of posterior capsular opacification (PCO) was significantly higher in the ECCE group than in the phacoemulsification group.253 Other nonultrasonic methods to remove the nucleus through a small incision, such as laser, mechanical, or high frequency water pulse technology, have been developed and are evolving.
|
Test Video |
The ideal technical elements of a successful cataract procedure currently include the following:
- Capsular bag fixation of an appropriate posterior chamber IOL.
- Minimal or no trauma to the corneal endothelium, iris, and other ocular tissues.
- A secure, watertight incision that minimizes surgically-induced astigmatism or reduces pre-existing corneal astigmatism.
Intraocular steps that are commonly used during phacoemulsification include the following:
- Construction of an appropriately sized incision that is tight enough to achieve a fluidically stable anterior chamber.
- Use of an ophthalmic viscosurgical device (OVD) to protect the corneal endothelium, manipulate tissues, and maintain adequate working space during surgery.
- Capsulorrhexis.256 This is a continuous curvilinear capsulotomy that facilitates hydrodissection, prevents posterior capsule tears that originate from radial anterior capsule tears, and facilitates the implantation and fixation of the IOL within the capsular bag. A capsulorrhexis that completely overlaps the IOL edge impedes the development of PCO.
- Hydrodissection,257 which reduces zonular stress during phacoemulsification by mobilizing the nucleus and epinucleus. By facilitating thorough cortical aspiration, hydrodissection also helps to retard PCO.258
- Nuclear disassembly and emulsification using techniques such as divide and conquer259 or chopping260 to minimize surgical trauma to intraocular tissues.
- Thorough removal of remaining epinucleus and cortex.
- Implantation and centration of a small-incision IOL within the capsular bag, or as dictated by surgical events, secure fixation of the IOL in the ciliary sulcus (with or without sutures) or anterior chamber.
- Removal of the OVD to minimize postoperative IOP elevation.
- Assurance of a watertight incision using sutures if the incision size and architecture alone do not produce a secure, self-sealing wound.
Surgical Follow-up
The ophthalmologist who performs the cataract surgery has a unique perspective and thorough understanding of the patient’s intraoperative course, postoperative condition, and response to surgery. The operating ophthalmologist is responsible for the care of the patient during the postoperative interval, the time in which most complications occur and within which stable visual function is achieved, and has an ethical obligation to the patient that continues until postoperative rehabilitation is complete. The operating ophthalmologist should also provide those aspects of postoperative eye care that are within the unique competence of the ophthalmologist (which do not include those aspects of postoperative care permitted by law to be performed by auxiliaries, and, for non-ophthalmological physicians, may also exclude additional functions). If such follow-up care is not possible, the operating ophthalmologist must make arrangements before surgery to refer the patient to a properly licensed, qualified health care professional for postoperative care with the prior approval of the patient and the health care professional. In rare special circumstances, such as emergencies or if no ophthalmologist is available, the operating ophthalmologist may make different arrangements for the provision of those aspects of postoperative eye care within the unique competence of the ophthalmologist, as long as the patient’s rights and welfare are the primary considerations.
The ophthalmologist who performs surgery has an obligation to inform patients about appropriate signs and symptoms of possible complications, eye protection, activities, medications, required visits, and details for access to emergency care. The ophthalmologist should also inform patients of their responsibility to follow advice and instructions provided during the postoperative phase and to notify the ophthalmologist promptly if problems occur.Patients should always have access to an ophthalmologist for appropriate care if serious problems arise.
Most ophthalmologists provide all postoperative care in their offices. Other members of a team of eye care professionals may also participate in the comanagement of postoperative care. The operating ophthalmologist is responsible to the patient for those aspects of postoperative care delegated to other eye care professionals.
Postoperative regimens of topically applied antibiotics, corticosteroids, and NSAIDs vary among practitioners. There are no controlled investigations that establish optimal regimens for the use of topical agents; therefore, it is the decision of the operating surgeon to use any or all of these products singly or in combination. Complications of postoperative medications include elevated IOP with corticosteroids and allergic reactions to antibiotics. Rarely, significant corneal reactions, including epithelial defects and stromal ulceration and melting, have been reported with topical ocular NSAIDs.
Complications
Complications specific to the IOL occur infrequently. The most common reasons for IOL explantation include incorrect power, opacification, decentration or dislocation, and glare or optical aberrations.Intraocular lenses may be damaged during implantation, and it may be necessary for the surgeon to consider intraoperative implant exchange.
The accuracy of IOL power selection is impaired when the preoperative ocular measurements are unreliable such as following prior keratorefractive surgery (see Cataract Surgery Following Refractive Surgery section). When an unacceptable refractive error results following IOL implantation, the surgeon and patient should discuss further surgical intervention, and the risks of intervention must be weighed against the alternatives of spectacle or contact lens correction. Surgical alternatives to IOL exchange include keratorefractive surgery and secondary ciliary sulcus implantation of a piggyback IOL.
Opacification of the IOL optic is rare and has been reported more often with hydrophilic acrylic materials. The complication of interpseudophakic opacification can occur when lens epithelial cells migrate in between two piggybacked IOLs that have both been implanted within the capsular bag. This fibrocellular material is difficult to remove and may require explantation of both IOLs.
A malpositioned posterior chamber IOL can cause visual complaints, such as edge glare or intraocular inflammation associated with iris chafing,pigment dispersion, and pupillary capture of the optic. This complication is least likely with capsular bag implantation of the IOL. Posterior chamber IOL decentration can result from a damaged haptic, asymmetric capsular contraction and fibrosis, a torn posterior capsule or zonular dialysis, an insufficiently long IOL implanted in the ciliary sulcus, and placement of one haptic in the ciliary sulcus and the other inside the capsular bag.
Prognosis
Add text here
Additional Resources
Add text here
References
- ↑ Basic Clinical Science Course (BCSC) of the American Academy of Ophthalmology. Section 11. 2006 - 2007.
- ↑ Cataract in the Adult Eye: Surgery and Diagnostic Procedures. Preferred Practice Patterns.American Academy of Ophthalmology. September 2006.
- ↑ Keenan TDL, Chen Q, Agrón E, et al. DeepLensNet: Deep Learning Automated Diagnosis and Quantitative Classification of Cataract Type and Severity. Ophthalmology. 2022;129(5):571-584. doi:10.1016/j.ophtha.2021.12.017