Conjunctival Reactive Lymphoid Hyperplasia
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Original contributors: Vendantam S, Patadia S, Gugala Jr. Z, Brock DC, Huang A, Yen MT
Disease Entity
Conjunctival Reactive Lymphoid Hyperplasia (CRLH) is the manifestation of uncontrolled proliferation of lymphoid cells in the conjunctiva of the eyes. This hyperplasia is typically benign though in rare instances, it can progress to malignant lymphoma. CRLH comes from a group of Lymphoid Hyperplasia diseases which are characterized by lymphoproliferation and enlargement of the affected tissues which can include the liver and thyroid.
General manifestations of CRLH include tissue swelling, pain, redness, and pink colored lesions in the conjunctival stroma.[1] [2]
Etiology and History
CRLH may arise as a result of antigen stimulation of the conjunctiva mucosa-associated lymphoid tissue (MALT).[3] CRLH is also associated with aberrant autoimmune disease.[4] Chronic or acute MALT inflammation may also arise from allergies or infection with Chlamydia psittaci.[5] [6] However, the exact cause of development remains undetermined. CRLH occurs primarily in adolescents and adults with a higher predisposition in males. Adolescent patients usually present with an otherwise unremarkable history without systemic lymphoma.[5]
Diagnosis
Clinical diagnosis
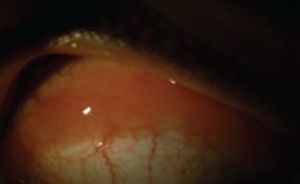
The primary presenting sign of benign CRLH is often a slow growth tumor in the conjunctiva in the form of a salmon-colored lesion, with little conjunctival infection and no significant neovascularization upon slit-lamp examination (Fig. 1).[7]
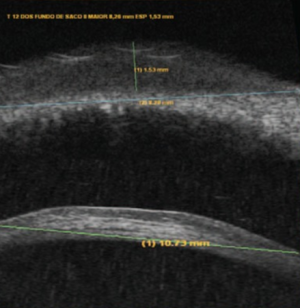
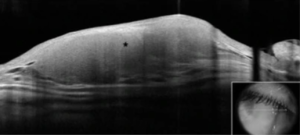
Ultrasound biomicroscopy may be performed to confirm lesion depth and diameter (Fig. 2).[7] On optical coherence tomography (OCT), the tumor presents as a homogeneous, hyporeflective lesion with thin overlying epithelium (Fig. 3).[2]
Physical examination
As a result of MALT inflammation, patients with CRLH usually present with a “salmon-patch” conjunctival lesion while experiencing symptoms including a palpable mass with swelling, proptosis, conjunctival irritation, diplopia, upper lid ptosis, and pain.[8] Irritation and palpable masses/lesions on the conjunctiva often form the patient’s chief complaint. Lesions are commonly located on the medial bulbar conjunctiva.[5] Many symptoms of CRLH overlap with conjunctival lymphoma and conjunctival amyloidosis. While conjunctival amyloidosis may be differentiated using HR-OCT, conjunctival lymphoma and CRLH are differentiated using histopathological evaluation, immunohistochemistry, flow cytometry and/or gene rearrangement.[9] [10]
Symptoms
Although many may not experience any symptoms, CRLH may present with one or more of the following:[1] [2]
- Enlarged lymph nodes, specifically in the neck
- Pain and redness
- Swelling of the eyelids
- Difficulty moving the eye
- Masses and/or lumps
- Blurred vision
- Bulging eyes
- Drooping eyes
Histopathological and Immunohistochemical Diagnosis
Dependent upon symptom presentation and findings from clinical examination, incisional biopsy may be recommended to confirm diagnosis and exclude neoplastic lesions. Histopathology of formalin-fixed tissue typically shows chronic inflammatory process presenting in lymphoid follicles (Fig. 4).[7]
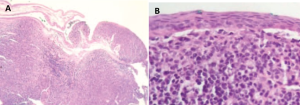
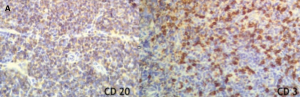
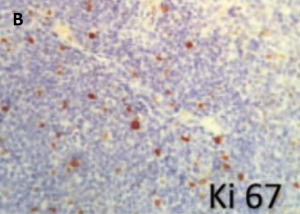
Analysis of fresh, unfixed tissue with flow cytometry for specific immunohistochemical antibodies stains positive for polyclonal markers (e.g., both CD3 T lymphocytes and CD20 B lymphocytes) (Fig. 5A).[7] Immunohistochemistry also reveals low levels of KI-67, a marker of active cell proliferation (Fig. 5B).[7]
Differential diagnosis
Differential diagnosis of CRLH includes conjunctival papilloma, foreign body granuloma, amyloid deposition, chronic follicular conjunctivitis, and other benign ocular surface tumors such as conjunctival pyogenic granulomas.[11] Malignant tumors such as squamous cell carcinoma and conjunctival lymphoma should also be considered and are of paramount importance to exclude early.[11]
Management
Medical therapy
Treatment is dependent on a variety of factors including the extent of symptoms present, comorbidities of other illnesses (e.g., Hodgkin's Lymphoma), and complexity/severity of the disease state. In many instances, careful observation can be the initial management for those who are asymptomatic or are not interested in pursuing further treatment. Historically, the first line of treatment for treating reactive lymphoid hyperplasia has been through administration of oral corticosteroids, such as prednisolone, alongside surgical resection of masses for symptomatic relief.[1] [7] Other forms of treatment include surgical resection with adjuvant perilesional steroid injection, cryotherapy, or external beam radiation therapy. Recent results have shown radiation therapy to be an effective treatment option especially if the condition is confined to only one orbit or for individuals who are contraindicated for corticosteroid use.[1] Studies have also shown that radiation therapy may also limit the extent of recurrence and malignancy development when compared to prednisone treatment alone.[1][12] Other reported forms of treatment have included use of doxycycline, cyclosporine 0.05%, and interferon ɑ-2b.[2][13] Novel treatments have been focusing on targeted-therapy approaches towards managing orbital lymphoid hyperplasia. Rituximab, a monoclonal antibody directed against the CD20 cell surface marker in B-lymphocytes, has been an increasingly popular treatment option for treatment.[1][14] One of the advantages towards using Rituximab over long-term corticosteroids are the decrease in steroid-associated side effects, lack of myelosuppression, and limited malignancy transformation.[1]
Complications
Since CRLH is generally benign, the most severe complication is a progression to malignancy as lymphoma. After therapy, there is a 20-30% chance for recurrence of the lesion, typically associated with lesions affecting the lacrimal gland. The incidence of lymphoma appears low across many studies and varies based on the monoclonality of the lesion. Without monoclonality, risk of lymphoma is around 8%. If the cells are derived from a single progenitor, risk for lymphoma increases to about ⅓ of cases. It is recommended that the progression of CRLH even after treatment should be tracked every six months to identify signs of recurrence or lymphoma.[1]
Prognosis
The outcomes for most patients with CRLH are positive. Given the main risk factor of recurring lesions, which affect approximately 20-30% of patients, there have been suggestions to follow up with patients for a minimum of 5 years.[1] The extent of the disease is the most important factor in determining risk of recurrence. There is a small risk for association with non-Hodgkin lymphoma. Additionally, some cases suggest that conjunctival lymphoma may arise from CRLH, emphasizing the need to prevent further malignancy.[15] Some isolated cases report thinning of the sclera along with the “salmon patch” lesion.[16] However, the prognosis for most patients is favorable when appropriate follow-up visits are taken.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Andrew NH, Coupland SE, Pirbhai A, Selva D. Lymphoid hyperplasia of the orbit and ocular ADNEXA: A clinical pathologic review. Survey of Ophthalmology. 2016;61(6):778-790. doi:10.1016/j.survophthal.2016.04.004
- ↑ 2.0 2.1 2.2 2.3 2.4 Klavdianou O, Kondylis G, Georgopoulos V, Palioura S. Bilateral benign reactive lymphoid hyperplasia of the conjunctiva: A case treated with oral doxycycline and review of the literature. Eye and Vision. 2019;6(1). doi:10.1186/s40662-019-0151-4
- ↑ Coupland S, Heegaard S. Can Conjunctival lymphoma be a clinical diagnosis? British Journal of Ophthalmology. 2013;98(5):574-575. doi:10.1136/bjophthalmol-2013-304309
- ↑ Kubota T, Moritani S. High incidence of autoimmune disease in Japanese patients with ocular adnexal reactive lymphoid hyperplasia. American Journal of Ophthalmology. 2007;144(1):148-149. doi:10.1016/j.ajo.2007.03.018
- ↑ 5.0 5.1 5.2 AlAkeely AG, Alkatan HM, Alsuhaibani AH, et al. Benign reactive lymphoid hyperplasia of the conjunctiva in childhood. British Journal of Ophthalmology. 2016;101(7):933-939. doi:10.1136/bjophthalmol-2016-309030
- ↑ Ferreri AJ, Guidoboni M, Ponzoni M, et al. Evidence for an association between Chlamydia Psittaci and ocular adnexal lymphomas. JNCI Journal of the National Cancer Institute. 2004;96(8):586-594. doi:10.1093/jnci/djh102
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 Moraes BRM, Nascimento MVDD, Neto EDDS, Santo RM. Topical steroids eye drops in conjunctival reactive lymphoid hyperplasia: Case report. Medicine (Baltimore). 2017;96(47):e8656. doi:10.1097/MD.0000000000008656
- ↑ Coupland SE, Krause L, Delecluse HJ, et al. Lymphoproliferative lesions of the ocular adnexa. Analysis of 112 cases. Ophthalmology. 1998;105(8):1430-1441. doi:10.1016/S0161-6420(98)98024-1
- ↑ Beykin G, Pe'er J, Amir G, Frenkel S. Paediatric and adolescent elevated conjunctival lesions in the plical area: Lymphoma or reactive lymphoid hyperplasia? British Journal of Ophthalmology. 2013;98(5):645-650. doi:10.1136/bjophthalmol-2013-303527
- ↑ Venkateswaran N, Mercado C, Tran AQ, et al. The use of high resolution anterior segment optical coherence tomography for the characterization of conjunctival lymphoma, conjunctival amyloidosis and benign reactive lymphoid hyperplasia. Eye and Vision. 2019;6(1). doi:10.1186/s40662-019-0143-4
- ↑ 11.0 11.1 Andrew NH, Coupland SE, Pirbhai A, Selva D. Lymphoid hyperplasia of the orbit and ocular ADNEXA: A clinical pathologic review. Survey of Ophthalmology. 2016;61(6):778-790. doi:10.1016/j.survophthal.2016.04.004 Koppinger J, Silkiss RZ, Burkat CN. Conjunctival Lymphoma. EyeWiki. https://eyewiki.aao.org/Conjunctival_Lymphoma#:~:text=The%20differential%20diagnosis%20of%20conjunctival,deposition%2C%20and%20chronic%20follicular%20conjunctivitis.
- ↑ Kennerdell JS, Flores NE, Hartsock RJ. Low-dose radiotherapy for lymphoid lesions of the orbit and ocular Adnexa. Ophthalmic Plastic & Reconstructive Surgery. 1999;15(2):129-133. doi:10.1097/00002341-199903000-00012
- ↑ Criden MR, Bardenstein DS, Schnur GA. Successful Treatment With Doxycycline of Orbital and Multifocal Reactive Lymphoid Hyperplasia (RLH) Due to Presumed Chlamydia Psittaci. Investigative Ophthalmology & Visual Science. 2005;46(13):5414.
- ↑ Chen A, Hwang TN, Phan LT, McCulley TJ, Yoon MK. Long-term management of orbital and systemic reactive lymphoid hyperplasia with rituximab. Middle East Afr J Ophthalmol. 2012;19(4):432-435. doi:10.4103/0974-9233.102770
- ↑ Fukuhara J, Kase S, Noda M, Ishijima K, Yamamoto T, Ishida S. Conjunctival lymphoma arising from reactive lymphoid hyperplasia. World Journal of Surgical Oncology. 2012;10(1). doi:10.1186/1477-7819-10-194
- ↑ Rofail M, Lee LR, Whitehead K. Conjunctival benign reactive lymphoid hyperplasia associated with myopic scleral thinning. Clinical and Experimental Ophthalmology. 2005;33(1):73-75. doi:10.1111/j.1442-9071.2004.00947.x

