Conjunctival Lymphangiectasia
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Conjunctival lymphangiectasia (CL) is a rare condition characterized by dilated lymphatic vessels in the conjunctiva, the thin, transparent membrane that covers the front surface of the eye and lines the inside of the eyelids.
Disease
The lymphatic vessels in the conjunctiva are responsible for draining excess fluid and waste products from the eye, and their dilation can lead to a range of symptoms, including redness, swelling, irritation, and tearing.
Conjunctival Lymphangiectasia can manifest in two distinct forms: diffuse or localized. In the diffuse form, there is swelling of the conjunctiva (chemosis), and the lymphatic vessels are spread out over a wide area. In the localized form, the lymphatic vessels appear as a series of small, pearl-like bumps (referred to as a "string of pearls" appearance). This localized form may be present in only one or both eyes, which is more commonly associated with a systemic disease.[1]
Lymphangiectasia hemorrhagica conjunctivae is the term used to describe a lesion that occurs when there is a link between a blood vessel and the enlarged lymphatics, causing the area to intermittently fill with blood.[2]
Etiology
The exact cause of conjunctival lymphangiectasia is not fully understood, although it has been linked to a number of factors, including trauma, infection, inflammation, and congenital abnormalities.[3]
Infantile conjunctival lymphangiectasia and lymphedema are typically classified as primary and caused by underdevelopment of the lymphatic system. They are often associated with systemic disorders like Turner syndrome [4], Kippel-Trenaunay-Weber syndrome [5], conjunctival and peripheral lymphedema with distichiasis, or Nonne-Milroy-Meige disease [6], all of which have significant systemic morbidity. Thus, when diagnosing infantile conjunctival lymphangiectasia, a thorough general examination should be performed to rule out other potential disorders.[7]
Current literature suggests that there is a link between conjunctival lymphangiectasia and Fabry disease, as both conditions involve an altered lymphatic system. While cornea verticillata is the most common ocular finding in individuals with this lysosomal storage disorder, the presence of CL and dry eye syndrome should not be overlooked.[8] Although the prevalence of conjunctival lymphangiectasia is only 1% in the general population, it has been found to be significantly higher in patients with hereditary transthyretin amyloidosis and could potentially serve as a biomarker for severe systemic disease.[9]
Diagnosis
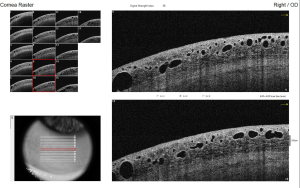
Diagnosis typically involves a detailed eye examination, as well as imaging tests such as ultrasound or anterior segment optical coherence tomography (ASOCT), to evaluate the extent of lymphatic dilation. The hyporeflective lesions vary in size and are cyst-like lesions on ASOCT. [10] Histopathological examination is invasive and confirms the diagnosis.
Differential diagnosis
- Conjunctivochalasis
- Inclusion cyst
- Conjunctival phlyctenulosis
- Pingueculum
- Conjunctival intraepithelial neoplasia
- Cyst conjunctival nevi
- Lymphangioma
- Allergic conjunctivitis
- Dead Loa Loa[11]
- Carotid Cavernous Fistula
Management
In most cases, conjunctival lymphangiectasia resolves on its own without any intervention.
Treatment options for conjunctival lymphangiectasia depend on the severity of the symptoms. They may include topical as antihistamine and steroids or oral medications to reduce inflammation and swelling and surgical intervention in more severe cases.
Patients with conjunctival lymphangiectasia have several treatment options available, including surgical excision, cryotherapy, anti-vascular endothelial growth factor (anti-VEGF) subconjunctival injections, and radio wave electro-ablation.
Welch et al. described a successful treatment approach involving excision followed by conjunctival autograft or amniotic membrane transplant, resulting in reduced recurrence rates.[3] A case report published in 2018 presented the option of lesion resection followed by suturing the remaining tissue with an 8.0 Vicryl.[12]
Liquid nitrogen cryotherapy, which was described in a 2009 article, can be an efficient surgical alternative for the management of conjunctival lymphangiectasia. In certain cases, cryotherapy may need repeated to achieve optimal results.[13]
A single dose of subconjunctival injection with Avastin has also been effective in targeting VEGF, which plays a significant role in lymphangiogenesis.[14]
The latest approach for treating conjunctival lymphangiectasia involves using high-frequency radiowaves to ablate the affected area. This technique is highly promising, as it helps retain more conjunctival tissue than surgical excision. It is also a preferred first-line treatment option for conjunctival lymphangiectasia.[15] [16]
While surgical excision is a more invasive option, it is associated with a much lower recurrence rate than other treatment modalities.
Complications
Conjunctival lymphangiectasia is a rare condition; early diagnosis and management can help to prevent complications and improve the quality of life for affected individuals.
References
- ↑ Cristea, A.P., L.T. Petrescu, and C. Stan, Conjunctival Lymphangiectasia - case report. Rom J Ophthalmol, 2022. 66(4): p. 365-368.
- ↑ Awdry, P., Lymphangiectasia hemorrhagica conjunctivae. Br J Ophthalmol, 1969. 53(4): p. 274-8.
- ↑ 3.0 3.1 Welch, J., et al., Conjunctival lymphangiectasia: a report of 11 cases and review of literature. Surv Ophthalmol, 2012. 57(2): p. 136-48.
- ↑ Perry, H.D. and A.J. Cossari, Chronic lymphangiectasis in Turner's syndrome. Br J Ophthalmol, 1986. 70(5): p. 396-9.
- ↑ Ramasubramanian, A., et al., Conjunctival edema and distichiasis in association with congenital lymphedema of the lower legs. Ophthalmic Plast Reconstr Surg, 2009. 25(2): p. 148-50.
- ↑ Tabbara, K.F. and S.A. Baghdassarian, Chronic hereditary lymphedema of the legs with congenital conjunctival lymphedema. Am J Ophthalmol, 1972. 73(4): p. 531-2.
- ↑ Pastora, N., et al., Conjunctival lymphangiectasia presenting as pediatric pseudopterygium. Eye Contact Lens, 2013. 39(3): p. e12-4.
- ↑ Sivley, M.D., et al., Conjunctival lymphangiectasia associated with classic Fabry disease. Br J Ophthalmol, 2018. 102(1): p. 54-58.
- ↑ Bunod, R., et al., Conjunctival lymphangiectasia as a biomarker of severe systemic disease in Ser77Tyr hereditary transthyretin amyloidosis. Br J Ophthalmol, 2020. 104(10): p. 1363-1367.
- ↑ Daya, S.M. and R. Papdopoulos, Ocular coherence tomography in lymphangiectasia. Cornea, 2011. 30(10): p. 1170-2.
- ↑ Singh, S., et al., Conjunctival Lymphangiectasia Simulating Loa Loa. Ophthalmic Plast Reconstr Surg, 2022.
- ↑ Seven, E., et al., Conjunctival lymphangiectasia: A case report. Eastern Journal Of Medicine, 2018. 23(4): p. 316.
- ↑ Fraunfelder, F.W., Liquid nitrogen cryotherapy for conjunctival lymphangiectasia: a case series. Trans Am Ophthalmol Soc, 2009. 107: p. 229-32.
- ↑ Tan, J.C., S. Mann, and M.T. Coroneo, Successful Treatment of Conjunctival Lymphangiectasia With Subconjunctival Injection of Bevacizumab. Cornea, 2016. 35(10): p. 1375-7.
- ↑ Choi, S.M., K.H. Jin, and T.G. Kim, Successful treatment of conjunctival lymphangiectasia accompanied by corneal dellen using a high-frequency radiowave electrosurgical device. Indian J Ophthalmol, 2019. 67(3): p. 409-411.
- ↑ Han, K.E., C.Y. Choi, and K.Y. Seo, Removal of lymphangiectasis using high-frequency radio wave electrosurgery. Cornea, 2013. 32(4): p. 547-9.