Conductive Keratoplasty
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Conductive Keratoplasty (CK) is a noninvasive procedure which utilizes radiofrequency energy to correct presbyopia and low hyperopia with or without astigmatism. It can also be used to correct residual refractive error after laser in-situ keratomileusis (LASIK) or cataract surgery. The portable nature of CK and its low comparative cost are benefits. However, this technology has largely fallen out of favor with most refractive surgeons given the high rate of regression after several years.
Other procedures used to correct hyperopia include LASIK, photorefractive keratectomy (PRK), noncontact and contact laser thermal keratoplasty (LTK), diode laser keratoplasty, thermokeratoplasty, intracorneal implants, and intraocular lenses. While LASIK, PRK and, laser-assisted subepithelial keratectomy (LASEK) are most popular for low to moderate hyperopia correction, some patients are not good candidates for laser procedures due to anatomical, pathological, or psychological reasons. For these patients, CK involves no laser, change to the central cornea, tissue cutting, or tissue removal. Several studies have shown that CK is an effective, predictable, stable, and safe procedure.
Biomechanics of Conductive Keratoplasty
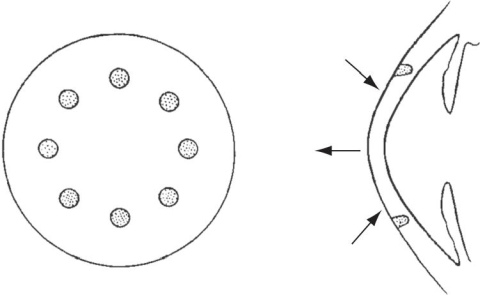
Treatment with CK is based on the effect of temperature on the biomechanical properties of the cornea.[1] At 55-65°C, collagen dehydrates and retracts, but retains its original configuration on cooling. At temperatures above 70-100°C, however, collagen completely denatures resulting in necrosis and permanent damage.[2] CK delivers controlled-released radiofrequency current (350-400 kHz) within peripheral corneal stroma to a depth of 500 µm through a thin, hand held probe (keratoplast tip; Refractec Inc., Irvine, California). The electrical impedance to energy flow through collagen fibrils increases the tissue temperature to the 65°C target resulting in controlled shrinkage of the peripheral collagen lamellae.[2][3][4][5] Circles of eight spots are created by repeated insertion of the probe at 6, 7, or 8 mm circumference optical zones as determined by nomogram for a total of 8, 16, 24, or 32 spots. Shrinking the peripheral collagen has a tightening effect on the mid-peripheral cornea which causes increased curvature of the central cornea, increasing refractive power. (See Figure 1)
Astigmatism, corneal trauma, previously decentrated ablation, and keratoconus may also be treated by adding spots to the flat meridian.[7][8][9]
Preoperative Evaluation
A complete medical and ocular history should be obtained prior to CK. Complete ophthalmologic examination should also be performed, including manifest and cycloplegic refraction, uncorrected visual acuity, best spectacle-corrected visual acuity, slit-lamp and dilated fundus examination, tonometry, corneal pachymetry, and computed corneal topography. Soft contact lenses should not be worn for 2 weeks prior to this examination, and rigid gas permeable (RGP) contact lenses should be stopped for 4 weeks prior at minimum plus 1 additional week for every 10 years of RGP wear. Refractive stability should also be demonstrated with minimal discrepancy between manifest and cycloplegic refraction.
Contraindications
Contraindications to CK may include pregnancy, breastfeeding, corneal dystrophies or corneal scarring within the central 6-7 mm optical zone, history of herpetic keratitis, autoimmune or collagen vascular disease, significant atopic disease, insulin-dependent diabetes, or immunocompromised states.[10]
Procedure
While surgical techniques vary, most involve a similar procedure. Topical anesthesia and antibiotics are administered to the eyes and the operated eye is prepped and draped in a sterile fashion. A lid speculum is placed in the eye and the visual axis is marked with ink using a Sinsky hook. The inked CK marker is then centered over the visual axis and applied to the cornea. A fiber-free sponge is then used to dry the cornea to prevent dissipation of the applied energy by a wet surface. The CK console is then set to the appropriate power and duration for the procedure and a sterile keratoplast tip is applied to a sterile handpiece. The keratoplast tip is then inserted into to the cornea in the marked areas as guided by the nomogram to create appropriate spots. The amount of visual correction at a given spot is determined by the degree of pressure applied. For example, using LightTouch CK, enough pressure is applied to produce a 2 mm dimple in the cornea to achieve the desired correction. After the correct number of spots has been created in the peripheral cornea, antibiotic drops are again placed in the eye and a soft contact lens is placed over the cornea.[10][11]
Outcomes
The efficacy, as measured by UCVA, is 20/40 or better in >89% of eyes overall for correction of hyperopia and astigmatism. [12][13][14][15][16] The predictability, as measured by manifest refractive spherical equivalent (MRSE), is satisfactory overall.[12][13][14][15][16] The stability of CK, as measured by a mean diopter change in the MRSE during the follow up period, is excellent overall.[12][13][14][15][16] Finally, the safety of CK, as measured by a loss of >2 lines of best spectacle corrected visual acuity (BSCVA), is excellent.[12][13][14][15][16]
Complications
Intraoperative complications during CK are rare and include corneal aseptic necrosis.[10][11] The most common post-operative complaints are of foreign body sensation and light sensitivity during the first few days after surgery. Surgically induced astigmatism is a rare complication caused by several factors including inaccurate cornea markings, asymmetric application of spots, insertion of probe at an angle other than perpendicular to the cornea, and insertion of the probe into the same spot more than once.[8] Correction of surgically induced astigmatism is possible with enhancement. Clinical experience has suggested a loss of effect after several years, but there is a lack of published literature regarding the incidence of this phenomenon.
CK after LASIK and PRK
Although refractive surprises after LASIK are rare, overcorrection of myopia can occur, resulting in blurred vision at far and near distances, especially in pre-presbyopes and presbyopes. The initial treatment for hyperopia following myopic LASIK is repeated LASIK.[17][18] However, the cornea may be too thin to undergo an additional LASIK procedure. In such eyes, CK retreatment has been shown to effectively reduce hyperopia with predictable and safe results, although cylinder correction has produced some irregular and unpredictable outcomes.[19][20][21]
References
- ↑ Brinkmann R, Radt B, Flamm C, Kampmeier J, Koop N, Birngruber R: Influence of temperature and time on thermally induced forces in corneal collagen and the effect on laser thermokeratoplasty. Journal of cataract and refractive surgery 2000, 26(5):744-754.
- ↑ 2.0 2.1 Haw WW, Manche EE: Conductive keratoplasty and laser thermal keratoplasty. International ophthalmology clinics 2002, 42(4):99-106.
- ↑ Brinkmann R, Koop N, Geerling G, Kampmeier J, Borcherding S, Kamm K, Birngruber R: Diode laser thermokeratoplasty: application strategy and dosimetry. Journal of cataract and refractive surgery 1998, 24(9):1195-1207.
- ↑ Aquavella JV, Smith RS, Shaw EL: Alterations in corneal morphology following thermokeratoplasty. Archives of ophthalmology 1976, 94(12):2082-2085.
- ↑ Gasset AR, Kaufman HE: Thermokeratoplasty in the treatment of keratoconus. American journal of ophthalmology 1975, 79(2):226-232.
- ↑ American Academy of Ophthalmology. Thermokeratoplasty and conductive keratoplasty. https://www.aao.org/image/thermokeratoplasty-conductive-keratoplasty Accessed July 01, 2019.
- ↑ Hersh PS, Fry KL, Chandrashekhar R, Fikaris DS: Conductive keratoplasty to treat complications of LASIK and photorefractive keratectomy. Ophthalmology 2005, 112(11):1941-1947.
- ↑ 8.0 8.1 Pallikaris G, Naoumidi TL, Panagopoulou SI, Alegakis AK, Astyrakakis NI: Conductive keratoplasty for low to moderate hyperopia: 1-year results. Journal of refractive surgery 2003, 19(5):496-506.
- ↑ Kato N, Toda I, Kawakita T, Sakai C, Tsubota K: Topography-guided conductive keratoplasty: treatment for advanced keratoconus. American journal of ophthalmology 2010, 150(4):481-489 e481.
- ↑ 10.0 10.1 10.2 Fernandez-Suntay JP, Pineda R, 2nd, Azar DT: Conductive keratoplasty. International ophthalmology clinics 2004, 44(1):161-168.
- ↑ 11.0 11.1 Du TT, Fan VC, Asbell PA: Conductive keratoplasty. Current opinion in ophthalmology 2007, 18(4):334-337.
- ↑ 12.0 12.1 12.2 12.3 Naoumidi TL, Kounis GA, Astyrakakis NI, Tsatsaronis DN, Pallikaris IG: Two-year follow-up of conductive keratoplasty for the treatment of hyperopic astigmatism. Journal of cataract and refractive surgery 2006, 32(5):732-741.
- ↑ 13.0 13.1 13.2 13.3 Stahl JE: Conductive keratoplasty for presbyopia: 3-year results. Journal of refractive surgery 2007, 23(9):905-910.
- ↑ 14.0 14.1 14.2 14.3 Pallikaris IG, Naoumidi TL, Astyrakakis NI: Long-term results of conductive keratoplasty for low to moderate hyperopia. Journal of cataract and refractive surgery 2005, 31(8):1520-1529.
- ↑ 15.0 15.1 15.2 15.3 McDonald MB, Hersh PS, Manche EE, Maloney RK, Davidorf J, Sabry M: Conductive keratoplasty for the correction of low to moderate hyperopia: U.S. clinical trial 1-year results on 355 eyes. Ophthalmology 2002, 109(11):1978-1989; discussion 1989-1990.
- ↑ 16.0 16.1 16.2 16.3 McDonald MB, Durrie D, Asbell P, Maloney R, Nichamin L: Treatment of presbyopia with conductive keratoplasty: six-month results of the 1-year United States FDA clinical trial. Cornea 2004, 23(7):661-668.
- ↑ Lyle WA, Jin GJ: Laser in situ keratomileusis for consecutive hyperopia after myopic LASIK and radial keratotomy. Journal of cataract and refractive surgery 2003, 29(5):879-888.
- ↑ Rojas MC, Haw WW, Manche EE: Laser in situ keratomileusis enhancement for consecutive hyperopia after myopic overcorrection. Journal of cataract and refractive surgery 2002, 28(1):37-43.
- ↑ Chang JS, Lau SY: Conductive keratoplasty to treat hyperopic overcorrection after LASIK for myopia. Journal of refractive surgery 2011, 27(1):49-55.
- ↑ Habibollahi A, Hashemi H, Mehravaran S, Khabazkhoob M: Visual Outcomes of Conductive Keratoplasty to Treat Hyperopia and Astigmatism After Laser in situ Keratomileusis and Photorefractive Keratectomy. Middle East African journal of ophthalmology 2011, 18(3):238-242.
- ↑ Tomita M, Watabe M, Ito M, Tsuru T: Conductive keratoplasty for the treatment of presbyopia: comparative study between post- and non-LASIK eyes. Clinical ophthalmology 2011, 5:231-237.

