Choroidal Vascular Anomalies: Posterior Vortex Veins, Choroidal Macrovessels, Choroidal Macroaneurysms, and Choroidal Vessel Varix
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
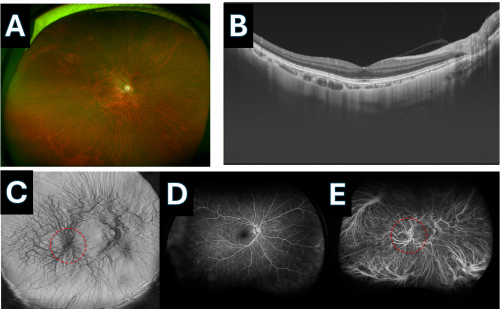
Choroidal vascular anomalies, such as posterior vortex veins, choroidal macrovessels, choroidal macroaneurysms, choroidal vessel varices, and pachyvessels are increasingly recognized in ophthalmic practice due to advancements in imaging technologies. These anomalies, once overlooked or misdiagnosed, have gained attention as potential contributors to various ocular pathologies, including central serous chorioretinopathy (CSCR), polypoidal choroidal vasculopathy (PCV), choroidal neovascularization (CNV), macroaneurysms, and hemorrhage, all of which can significantly impact vision. These vascular anomalies may mimic other serious conditions such as choroidal tumors, melanoma, metastatic lesions, and choroidal granulomas, leading to unnecessary and extensive diagnostic workups if not correctly identified. It is crucial for ophthalmologists to be familiar with these anomalies to avoid misdiagnosis and ensure proper management. Although these conditions are often benign, regular follow-up is recommended due to the risk of secondary complications, such as CNV, hemorrhage, and exudation, which can affect vision. En face Optical Coherence Tomography (OCT) is a valuable tool for visualizing choroidal vessels and is readily available in commercial OCT devices, providing detailed imaging that can aid in the diagnosis and monitoring of these conditions. If uncertainty remains, Indocyanine Green Angiography (ICG) can be employed to further investigate the vascular anomalies.
Posterior Vortex Veins or Macular Vortex Veins
Disease Entity
Disease
Posterior vortex veins or macular vortex veins are anatomical variants of the choroidal venous system. These veins are responsible for draining the choroid, which supplies blood to the outer retina. Posterior vortex veins are typically located around the equator of the eye, while macular vortex veins are an unusual variant that drains near or within the macular region, a critical area for central vision. The presence of macular vortex veins is particularly significant in conditions like high myopia and pachychoroid spectrum diseases, where they may contribute to pathological changes in the retina.[2][3]
Etiology
The etiology of posterior and macular vortex veins involves developmental variations in the venous drainage system of the choroid. Macular vortex veins may develop due to altered choroidal outflow, often associated with high myopia or other structural abnormalities of the eye. These veins can also be linked to changes in scleral thickness and structure, particularly in highly myopic eyes.[4][5]
Risk Factors
Risk factors for the development of macular vortex veins include:
- High Myopia: The elongation of the eyeball in high myopia can lead to changes in choroidal blood flow, increasing the likelihood of vortex vein anomalies.[6]
- Pachychoroid Spectrum Diseases: These conditions are characterized by a thickened choroid and may be associated with abnormal vortex veins.[7]
- Age: Although less clearly defined, age-related changes in the choroid may contribute to the development of vortex vein anomalies like posterior vortex vein varix.[8]
General Pathology
Posterior and macular vortex veins exhibit abnormal dilation or positioning relative to typical choroidal drainage patterns. In macular vortex veins, the drainage of choroidal blood near or within the macula can lead to significant clinical consequences, including an increased risk of choroidal neovascularization (CNV).[9]8
Pathophysiology
The pathophysiology of macular vortex veins involves altered venous drainage leading to increased venous pressure and congestion within the choroid. This can result in various pathological changes, including pachyvessel formation, choroidal thickening, and, in some cases, CNV. The abnormal location of these veins near the macula may directly impact central vision.[10][2]
Primary Prevention
Primary prevention of posterior or macular vortex veins is not well established due to their congenital and developmental nature. However, managing underlying conditions like high myopia and regular monitoring in patients with known risk factors may help prevent complications associated with these anomalies.[1]
Diagnosis
History
A detailed patient history focusing on visual symptoms, particularly those related to central vision, and any history of high myopia or other relevant ocular conditions is crucial. Understanding the patient's history of retinal conditions or previous surgeries can also provide valuable diagnostic clues.[11]12
Physical Examination
A comprehensive ophthalmic examination, including dilated fundus examination, is essential. The examination may reveal abnormal venous structures, particularly in the macular area in cases of macular vortex veins.[12]
Signs
Signs of macular vortex veins may include:
- Presence of large, dilated choroidal vessels near the macula
- Associated retinal pigment epithelial changes
- Potential subretinal fluid or hemorrhage if CNV is present[5]
Symptoms
Patients may present with symptoms such as:
- Blurred or distorted central vision
- Scotomas (blind spots) in the central field
- Photopsia (flashes of light) in cases with active CNV[2]
Clinical Diagnosis
Clinical diagnosis involves identifying the characteristic features of vortex veins using multimodal imaging techniques. The abnormal location and dilation of the veins near the macula can be visualized through advanced imaging.[6]
Diagnostic Procedures
Key diagnostic procedures include:
- Optical Coherence Tomography (OCT): Provides detailed images of the retina and choroid, revealing structural changes associated with macular vortex veins.[12]
- Indocyanine Green Angiography (ICGA): Useful for visualizing the choroidal vasculature and confirming the presence of abnormal veins. [7]
- Fluorescein Angiography (FA): May be used to assess the presence of CNV and other related retinal pathologies.[10]
Laboratory Tests
Laboratory tests are generally not necessary for diagnosing posterior or macular vortex veins unless systemic vascular conditions are suspected.[2]
Differential Diagnosis
Differential diagnoses include:
- Choroidal neovascularization from other causes
- Central serous chorioretinopathy (CSC)
- Polypoidal choroidal vasculopathy (PCV)
- Choroidal melanoma[6]
- Sclerochoroidal calcification
Management
General Treatment
Treatment is primarily directed towards managing complications, such as CNV, rather than the vortex veins themselves. Regular monitoring and imaging are essential to detect any changes early.[11]
Medical Therapy
Anti-VEGF therapy is the mainstay treatment for CNV associated with macular vortex veins. This therapy helps reduce neovascularization and preserve vision.
Medical Follow-Up
Patients with macular vortex veins require close follow-up, particularly if CNV is present or if there are significant retinal changes. Regular OCT and ICGA are recommended to monitor cases with suspected for complications or other diseases .[9]
Surgery
Surgical intervention is not typically required for posterior or macular vortex veins themselves but may be necessary to address complications such as retinal detachment[1]
Surgical Follow-Up
Post-surgical follow-up is essential to ensure proper healing and monitor for recurrence or new complications.[5][7]
Complications
Complications can include:
Development of CNV leading to vision loss Retinal detachment in severe cases of associated pathology Subretinal hemorrhage[8]
Prognosis
The prognosis depends on the presence and management of complications like CNV. With appropriate treatment, many patients can maintain stable vision, though some may experience progressive vision loss.[12]
Choroidal Macrovesseles
Disease Entity
Disease
Choroidal macrovessels are large, anomalous blood vessels located within the choroid layer of the eye. These vessels are typically dilated branches of the posterior ciliary arteries and can be seen as prominent vascular structures during imaging. Choroidal macrovessels are generally benign but can sometimes be associated with visual disturbances due to their effect on the overlying retinal architecture.[13],[14]
Etiology
The exact cause of choroidal macrovessels is not well understood. These vessels are thought to arise from congenital vascular anomalies or may develop due to chronic changes in choroidal blood flow, possibly as a compensatory response to ischemia or other vascular insufficiencies.[15][16]
Risk Factors
- High Myopia: The structural changes associated with high myopia, such as elongation of the eyeball, may increase the likelihood of developing choroidal macrovessels.[17]
- Age: Age-related changes in the choroid might contribute to the formation of macrovessels.[18]
General Pathology
Choroidal macrovessels are characterized by abnormally large and dilated vessels within the choroid. These vessels may cause displacement and distortion of the overlying retinal layers, particularly affecting the retinal pigment epithelium (RPE) and ellipsoid zone. The presence of these vessels can sometimes mimic other choroidal and retinal vascular pathologies.
Pathophysiology
The pathophysiology of choroidal macrovessels involves abnormal choroidal blood flow that leads to the dilation of existing vessels or formation of new, larger vessels. The pressure exerted by these vessels on the surrounding retinal structures can cause mechanical distortion, potentially leading to visual symptoms such as metamorphopsia.
Primary Prevention
Primary prevention of choroidal macrovessels is challenging due to their congenital or developmental origin. However, early detection and regular monitoring in high-risk patients, such as those with high myopia or pachychoroid spectrum diseases, may help prevent complications.
Diagnosis
History
Patients with choroidal macrovessels may report visual disturbances, including metamorphopsia, scotomas, or blurred vision. A detailed history of ocular conditions, especially in patients with high myopia or chronic ocular diseases, is essential for diagnosis.
Physical Examination
A thorough ophthalmic examination, including dilated fundus examination, is critical. Choroidal macrovessels may appear as large, dilated, and tortuous vessels within the choroid, which can sometimes extend into the retina.
Signs
Presence of large, dilated choroidal vessels, often visible on imaging. Retinal elevation or distortion, particularly affecting the ellipsoid zone and RPE. Associated retinal changes, such as subretinal fluid or hemorrhage, if complications like choroidal neovascularization are present.
Clinical Diagnosis
The diagnosis of choroidal macrovessels is typically made based on imaging studies. Key imaging techniques include optical coherence tomography (OCT), fluorescein angiography (FA), and indocyanine green angiography (ICGA), which help differentiate choroidal macrovessels from other choroidal or retinal vascular anomalies.
Diagnostic Procedures
- Optical Coherence Tomography (OCT): Provides high-resolution cross-sectional images of the retina and choroid, highlighting structural changes caused by the macrovessel.
- Fluorescein Angiography (FA): Used to visualize the retinal and choroidal circulation, helping to map the course and distribution of the macrovessel.
- Indocyanine Green Angiography (ICGA): Particularly useful for imaging choroidal vasculature and confirming the presence of macrovessels.
Laboratory
Tests
Laboratory tests are not typically required for diagnosing choroidal macrovessels unless there is a suspicion of systemic conditions affecting ocular health.
Differential Diagnosis
- Choroidal neovascularization (CNV)
- Central serous chorioretinopathy (CSC)
- Polypoidal choroidal vasculopathy (PCV)
- Retinal hemangioblastoma
- Choroidal melanoma
Management
General Treatment
Management of choroidal macrovessels involves monitoring for complications such as CNV. Regular imaging and follow-up are essential for early detection and intervention.
Medical Therapy
Anti-VEGF therapy is recommended if CNV is associated with the choroidal macrovessel, as this treatment helps reduce neovascular growth and preserve vision.
Medical Follow-Up
Patients should undergo regular follow-up with OCT and angiographic imaging to monitor for disease progression and detect complications early.
Surgery
Surgical intervention is generally not required for choroidal macrovessels themselves but may be necessary for addressing associated complications, such as retinal detachment or epiretinal membrane peeling.
Surgical Follow-Up
Post-surgical follow-up is critical to ensure proper healing and to monitor for recurrence of symptoms or new complications.
Complications
- Development of CNV, potentially leading to vision loss.
- Development choroidal macroaneurysms, see below.
- Persistent visual disturbances such as metamorphopsia.
- Retinal detachment in severe cases.
- Subretinal hemorrhage.
Prognosis
The prognosis for patients with choroidal macrovessels largely depends on the presence and management of associated complications. With appropriate treatment and monitoring, many patients can maintain stable vision, though some may experience progressive visual disturbances.
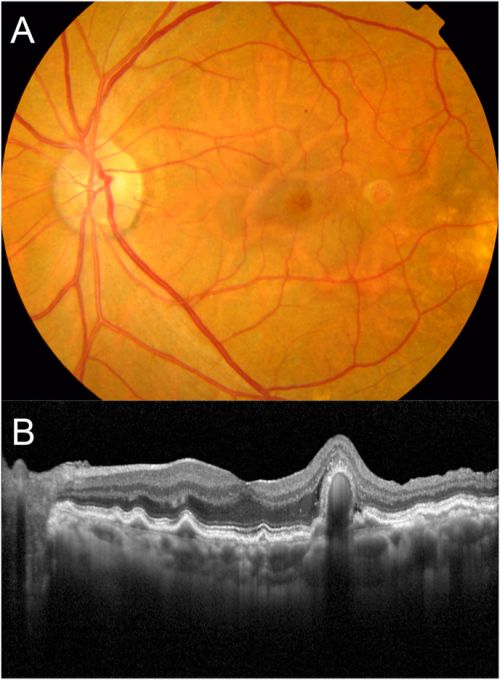
Choroidal Macroaneurysms
Disease Entity
Disease
Choroidal macroaneurysms are localized dilations of choroidal vessels, typically involving arteries rather than veins. These aneurysms can lead to visual impairment due to exudation, hemorrhage, or a combination of both, affecting the overlying retinal tissue.
Etiology
The etiology of choroidal macroaneurysms is not entirely understood but is believed to involve degenerative changes in the arterial walls, possibly exacerbated by systemic vascular conditions such as hypertension or arteriosclerosis.
Risk Factors
Risk factors for choroidal macroaneurysms include:
Systemic Hypertension: Elevated blood pressure may contribute to the formation and progression of aneurysms in the choroidal vasculature. Age: Older patients are at a higher risk due to age-related vascular changes. Arteriosclerosis: The hardening and loss of elasticity in arterial walls can predispose individuals to aneurysm formation.
General Pathology
Choroidal macroaneurysms involve the dilation of choroidal arteries, leading to structural changes that can cause exudation or hemorrhage into the retinal layers. The affected vessel typically displays a saccular aneurysmal dilation.
Pathophysiology
The pathophysiology of choroidal macroaneurysms involves the weakening of an anomalous short posterior ciliary artery, leading to localized dilation. This can cause blood leakage into surrounding tissues, leading to retinal detachment, hemorrhage, or macular edema, contributing to vision loss.
Primary Prevention
Primary prevention strategies for choroidal macroaneurysms include managing systemic conditions such as hypertension and arteriosclerosis to reduce the risk of aneurysm formation and progression.
Diagnosis
History
A thorough patient history should focus on visual symptoms such as sudden vision loss, floaters, or flashes of light, which may indicate hemorrhage or exudative changes associated with a macroaneurysm.
Physical Examination
A comprehensive ophthalmic examination, including fundoscopic examination, is essential to identify signs of aneurysm, such as retinal hemorrhage or exudation.
Signs
Common signs of choroidal macroaneurysms include:
- Retinal Hemorrhage: Visible bleeding within the retina or subretinal space.
- Exudation: Leakage of fluid leading to macular edema and potential vision loss.
- Protruding Lesions: Visible elevation or protrusion of the retina or choroid.
Clinical Diagnosis
Clinical diagnosis is primarily based on imaging studies, which reveal the aneurysmal dilation of choroidal vessels and associated retinal changes.
Diagnostic Procedures
Key diagnostic procedures include:
- Optical Coherence Tomography (OCT): Provides cross-sectional images of the retina, revealing the extent of fluid accumulation and structural changes.
- Fluorescein Angiography (FA): Highlights the choroidal circulation and can identify areas of leakage or aneurysmal dilation.
- Indocyanine Green Angiography (ICGA): Used to visualize the choroidal vessels more effectively, identifying the aneurysmal dilation.
Laboratory Tests
Laboratory tests are generally not necessary for diagnosing choroidal macroaneurysms unless there is a suspicion of systemic conditions contributing to the vascular changes.
Differential Diagnosis
Differential diagnoses include:
- Polypoidal Choroidal Vasculopathy (PCV): Characterized by branching vascular networks with aneurysmal dilations.
- Retinal Artery Macroaneurysm: Involves the dilation of retinal arteries rather than choroidal vessels.
- Central Serous Chorioretinopathy (CSC): Typically presents with serous detachment without aneurysmal changes.
Management
General Treatment
Treatment is aimed at managing complications such as hemorrhage or exudation. Observation may be appropriate in asymptomatic cases or when the aneurysm is stable without significant exudation.
Medical Therapy
Anti-VEGF Therapy: May be used to reduce vascular permeability and exudation in cases where there is significant fluid accumulation. Laser Photocoagulation: Direct treatment of the aneurysm may be considered to prevent further leakage and stabilize the lesion.
Medical Follow-Up
Patients require regular follow-up to monitor for changes in the aneurysm, such as increased leakage, hemorrhage, or progression leading to vision loss.
Surgery
Surgical intervention may be necessary in cases where there is a significant retinal detachment or persistent exudation that does not respond to medical therapy.
Surgical Follow-Up
Post-surgical follow-up is critical to ensure proper healing, monitor for recurrence, and manage any complications that may arise.
Complications
Potential complications of choroidal macroaneurysms include:
- Retinal Detachment: Due to extensive hemorrhage or exudation.
- Vision Loss: Secondary to macular involvement and persistent exudation or hemorrhage.
Prognosis
The prognosis for patients with choroidal macroaneurysms depends on the severity and location of the aneurysm, the presence of complications, and the effectiveness of treatment. With appropriate management, some patients may maintain stable vision, although others may experience progressive vision loss.[19]
Choroidal Varix
Disease Entity
Choroidal varix refers to the abnormal dilation of a vortex vein ampulla, which is often asymptomatic but can be mistaken for more serious choroidal or retinal conditions due to its appearance. This condition typically presents as a dark, elevated lesion on the choroid and may affect the overlying retinal pigment epithelium (RPE). The varices are usually benign but can cause significant clinical concern due to their resemblance to malignant lesions, such as choroidal melanomas.[11]
Disease
Choroidal varices are typically characterized by the dilation of vortex vein ampullae, which can present as isolated or multiple lesions. These varices can appear brownish-red to gray and are usually located in the mid-peripheral choroid. Although they are often detected incidentally, their appearance may lead to confusion with more serious conditions, requiring careful diagnosis.[20]
Etiology
The exact etiology of choroidal varices is not well understood. However, it is believed that increased ocular venous pressure or mechanical factors such as gaze-evoked kinking of the episcleral portion of a vortex vein may contribute to their development. Other potential contributing factors include narrowing of the scleral emissary canal and conditions that elevate venous pressure, such as Valsalva maneuvers or prone positioning.[20]
Risk Factors
Risk factors for the development of choroidal varices include:
- Increased ocular venous pressure
- Gaze-evoked mechanical stress on the vortex veins
- Advanced age, as these lesions are more commonly identified in older patients
- History of ocular trauma or surgery, which might contribute to altered venous drainage[11][20]
General Pathology
Choroidal varices exhibit abnormal dilation of the vortex vein ampullae. These dilations are typically benign and asymptomatic, but their presence can result in localized changes to the RPE, which may be mistaken for more concerning pathologies. In rare cases, varices can lead to a mass effect on surrounding structures, causing further complications.[11][20]
Pathophysiology
The pathophysiology of choroidal varices involves the dilation of vortex vein ampullae due to venous congestion. This congestion may arise from downstream obstructions or mechanical factors that impede normal venous outflow. In some cases, venovenous anastomoses or collateralization may develop to alleviate the congestion, potentially leading to the resolution of the varix.[11]
Primary Prevention
There are no established methods for the primary prevention of choroidal varices due to the unclear etiology and the typically benign nature of the condition. However, regular monitoring in patients with known risk factors may help in the early detection and differentiation from malignant lesions.[11]
Diagnosis
History
A thorough patient history is crucial, particularly focusing on any previous ocular surgeries, trauma, or symptoms that might suggest increased venous pressure. Patients are usually asymptomatic, and varices are often discovered incidentally during routine examinations.[20]
Physical Examination
Physical examination, including funduscopy, often reveals a dark, elevated choroidal lesion. The varix may change in appearance depending on the gaze or applied pressure, which can help differentiate it from other conditions.[11]
Signs
Signs of choroidal varices include:
- Elevated choroidal lesion, typically brownish-red to gray in color
- Absence of subretinal fluid or other associated retinal changes unless there is significant mass effect[20]
Symptoms
Most patients with choroidal varices are asymptomatic, and the condition is often discovered during routine eye examinations. Rarely, patients may notice visual disturbances if the varix exerts significant pressure on adjacent structures.[11]
Clinical Diagnosis
Clinical diagnosis is based on the characteristic appearance of the lesion during ophthalmoscopic examination, particularly noting any changes with gaze or applied pressure. Adjunctive imaging techniques are often necessary to confirm the diagnosis.[20]
Diagnostic Procedures
Key diagnostic procedures include:
- Optical Coherence Tomography (OCT): Reveals a hyporeflective cavity corresponding to the dilated choroidal vessels.
- Indocyanine Green Angiography (ICGA): Demonstrates early hyperfluorescence and dye pooling within the varix.
- Fundus Autofluorescence: Shows hypofluorescent rings surrounding the lesion.[20]
Laboratory Tests
Laboratory tests are generally not required for diagnosing choroidal varices unless there is suspicion of underlying systemic conditions that could contribute to venous congestion.[11]
Differential Diagnosis
Differential diagnoses include:
- Choroidal melanoma
- Choroidal hemangioma
- Subretinal hemorrhage
- Metastatic choroidal lesions[20]
Management
General Treatment
Choroidal varices are generally benign and do not require treatment unless they cause significant symptoms or are mistaken for malignant lesions. Management typically involves monitoring with periodic imaging to ensure stability.[20]
Medical Therapy
Medical therapy is not typically required for choroidal varices. However, in cases where venous congestion is suspected to be contributing to the varix, treatment of the underlying cause may be considered.[11]
Medical Follow-Up
Regular follow-up is recommended to monitor the varix for any changes in size or appearance that could suggest a shift in the underlying pathology. Imaging techniques such as OCT and ICGA are useful for this purpose.[20]
Surgery
Surgical intervention is not commonly indicated for choroidal varices, as they are generally benign. However, if the varix is causing significant symptoms or is misdiagnosed as a malignancy, surgical excision may be considered.[20]
Surgical Follow-Up
Post-surgical follow-up should include regular imaging to monitor for recurrence and ensure that any residual varices do not cause further complications.[11]
Complications
Complications associated with choroidal varices are rare but may include:
- Misdiagnosis as a malignant lesion, leading to unnecessary interventions
- Localized changes in the RPE due to mass effect
- Venous congestion leading to the formation of additional varices[20]
Prognosis
The prognosis for patients with choroidal varices is generally excellent, as these lesions are benign and often remain stable over time. In some cases, the varix may resolve spontaneously, as noted in rare instances.[11]
Pachyvessels
Disease Entity
Pachyvessels are abnormally dilated choroidal vessels found within the Haller's layer of the choroid, commonly associated with pachychoroid spectrum diseases. These vessels are linked to various ocular conditions, including central serous chorioretinopathy (CSC), pachychoroid neovasculopathy (PNV), and polypoidal choroidal vasculopathy (PCV). The presence of pachyvessels is typically indicative of underlying choroidal thickening and altered choroidal hemodynamics.[21]
Disease
Pachyvessels play a central role in the pathophysiology of pachychoroid diseases. These enlarged vessels contribute to choroidal thickening, which can compress the overlying choriocapillaris and cause ischemia. This ischemia may lead to retinal pigment epithelium (RPE) changes, serous retinal detachment, and the development of choroidal neovascularization (CNV).[22]
Etiology
The etiology of pachyvessels is not entirely understood, but they are believed to arise from chronic venous congestion within the choroid. This congestion could be due to systemic factors like hypertension or localized factors such as thickened sclera, which restricts normal venous outflow.[23]
Risk Factors
Risk factors for the development of pachyvessels include:
- Central Serous Chorioretinopathy (CSC): A condition frequently associated with pachyvessels due to choroidal thickening.[24]
- Hypertension: Systemic hypertension is a significant risk factor due to its potential to increase choroidal venous pressure.[22]
- Age: Aging can lead to structural changes in the choroid, contributing to the development of pachyvessels.[23]
General Pathology
Pachyvessels are characterized by their significant dilation and thickening within the Haller's layer of the choroid. These vessels can cause compression of the overlying choriocapillaris, leading to reduced perfusion and ischemia in the outer retina. This can result in RPE dysfunction, serous retinal detachment, and choroidal neovascularization.[21][22]
Pathophysiology
The presence of pachyvessels leads to a cascade of pathological events. The dilated vessels compress the choriocapillaris, causing reduced blood flow and ischemia in the outer retina. This ischemia can lead to RPE dysfunction, serous retinal detachment, and the potential development of CNV. Additionally, choroidal hyperpermeability often accompanies pachyvessels, exacerbating retinal pathology.[21][24]
Primary Prevention
Primary prevention of pachyvessels focuses on managing systemic risk factors, particularly hypertension. Regular monitoring of individuals with a history of CSC or other pachychoroid spectrum diseases may help prevent complications associated with pachyvessels.
Diagnosis
History
Patients may report symptoms such as blurred vision or metamorphopsia, often linked to underlying conditions like CSC. A history of hypertension or other vascular diseases is also significant in the context of pachyvessels.
Physical Examination
Ophthalmic examination typically reveals signs of serous retinal detachment or RPE changes, particularly in the macula. Imaging is crucial for the identification of pachyvessels.
Signs
- Dilated and thickened choroidal vessels visible on imaging.
- Compression of the choriocapillaris leading to ischemic changes in the retina.[21]
Symptoms
- Blurred vision
- Metamorphopsia
- Scotomas in cases where CNV develops.
Clinical Diagnosis
The diagnosis of pachyvessels is confirmed through multimodal imaging, where their characteristic dilation and thickening are visible.
Diagnostic Procedures
- Optical Coherence Tomography (OCT): Visualizes the thickened choroid and pachyvessels.[23]
En Face OCT is a vital imaging modality in the detection and management of pachyvessels and related lesions in pachychoroid spectrum diseases. This advanced technique provides a broad, detailed view of the choroid, allowing for the precise mapping of pachyvessels, which appear as large hyporeflective spaces within the Haller’s layer. En face OCT is particularly effective in identifying areas of choroidal thickening, congestion, and interactions at choroidal watershed zones, which are critical for understanding disease pathophysiology. It also correlates structural abnormalities with functional changes, such as choroidal hyperpermeability, aiding in the comprehensive assessment of conditions like central serous chorioretinopathy (CSC) and pachychoroid neovasculopathy (PNV). Overall, en face OCT enhances the early detection, accurate diagnosis, and targeted management of these conditions, surpassing traditional imaging techniques in its detailed and expansive visualization capabilities.
- Indocyanine Green Angiography (ICGA): Highlights hyperpermeable areas and dilated vessels.[24]
- Optical Coherence Tomography Angiography (OCT-A): Assesses blood flow and identifies CNV.[22]
Laboratory Tests
Laboratory tests are not typically necessary for diagnosing pachyvessels unless there is a need to assess systemic conditions.
Differential Diagnosis
Differential diagnoses include:
Polypoidal choroidal vasculopathy (PCV) Central serous chorioretinopathy (CSC) Choroidal neovascularization (CNV) from other causes[23]
Management
General Treatment
Management primarily involves treating associated complications like CNV. Regular monitoring and imaging are crucial to identify and address any progression or complications related to pachyvessels.[22]
Medical Therapy
- Anti-VEGF Therapy: Used to manage CNV associated with pachyvessels, aiming to reduce neovascularization and preserve vision.[24]
Medical Follow-Up
Regular follow-up is essential for patients with pachyvessels, especially if CNV is present or there are significant retinal changes. OCT and ICGA are recommended to monitor disease progression.[21]
Surgery
Surgical intervention is not typically required for pachyvessels themselves but may be necessary to address complications such as retinal detachment.[23]
Surgical Follow-Up
Post-surgical follow-up is crucial to ensure proper healing and monitor for recurrence or new complications.[22][24]
Complications
Complications related to pachyvessels include:
- Development of CNV leading to vision loss.
- Retinal detachment in severe cases.
- Subretinal hemorrhage.[21]
Prognosis
The prognosis for patients with pachyvessels depends on the presence and management of complications like CNV. With appropriate treatment, many patients can maintain stable vision, though some may experience progressive vision loss.[22]
Additional Resources
Add text here
References
- ↑ 1.0 1.1 1.2 Nitta K, Akiyama H (July 02, 2024) Different Vortex Vein Anomalies Observed in a Single Case: Macular Vortex Vein in One Eye and Varix of Vortex Vein Ampulla in the Other Eye. Cureus 16(7): e63668. doi:10.7759/cureus.63668
- ↑ 2.0 2.1 2.2 2.3 Schouten IM, Palkar AH, Bhende M. Macular vortex vein with choroidal neovascularisation in pathologic myopia. Indian J Ophthalmol. 2019;67(10):1717-1718.
- ↑ Sharma A, Parachuri N, Kumar N, et al. Vortex vein anastomosis and pachychoroid—an evolving understanding. Eye. 2021;35(6):1545-1547.
- ↑ Ohno-Matsui K, Morishima N, Ito M, et al. Posterior routes of choroidal blood outflow in high myopia. Retina. 1996;16(5):419-425.
- ↑ 5.0 5.1 5.2 Patel G, He G, Zhang X, Wen F. Subfoveal focal choroidal excavation with macular vortex vein. Ophthalmology Retina. 2023;17(6):41-43.
- ↑ 6.0 6.1 6.2 Matsumoto H, Hoshino J, Arai Y, et al. Vortex vein anastomosis at the watershed in pachychoroid spectrum diseases. Ophthalmol Retina. 2020;4(9):938-945.
- ↑ 7.0 7.1 7.2 Hiroe T, Kishi S. Dilatation of asymmetric vortex vein in central serous chorioretinopathy. Ophthalmol Retina. 2018;2(2):152-161
- ↑ 8.0 8.1 Matsumoto H, Kishi S, Mukai R, Akiyama H. Remodeling of macular vortex veins in pachychoroid neovasculopathy. Sci Rep. 2019;9:14689.
- ↑ 9.0 9.1 Spaide RF. Choroidal blood flow: review and potential explanation for the choroidal venous anatomy including the vortex vein system. Retina. 2020;40(9):1851-1864.
- ↑ 10.0 10.1 Milani P, Mazzola M, Bergamini F. Suprachoroidal hemorrhage and vortex vein varix: a potential association. Eur J Ophthalmol. 2020;30(5):943-946.
- ↑ 11.00 11.01 11.02 11.03 11.04 11.05 11.06 11.07 11.08 11.09 11.10 11.11 11.12 Weidmayer SL, Demirci H. The spontaneous resolution of a vortex vein varix: case report. BMC Ophthalmol. 2021;21(1):101.
- ↑ 12.0 12.1 12.2 Spaide RF, Ledesma-Gil G, Cheung CMG. Intervortex venous anastomosis in pachychoroid-related disorders. Retina. 2020;40(9):1851-1864.
- ↑ Lima LH, Laud K, Chang LK, Yannuzzi LA. Choroidal macrovessel. Br J Ophthalmol. 2011;95(9):1333-1334. doi:10.1136/bjo.2011.206829.
- ↑ Ehlers JP, Rayess H, Spaide RF. Isolated choroidal macrovessel: a track-like choroidal lesion. Can J Ophthalmol. 2014;49(6) . doi:10.1016/j.jcjo.2014.09.006.
- ↑ Choudhry N, Rao RC. Enhanced depth imaging features of a choroidal macrovessel. Retin Cases Brief Rep. 2016;10(1):18-21.doi:10.1097/ICB.0000000000000157.
- ↑ Casalino G, De Simone L, Scialdone A, Pavesio C. Choroidal macrovessel: Optical coherence tomography angiography and imaging features. Indian J Ophthalmol. 2019;67(7):1168-1170. doi:10.4103/ijo.IJO_2085_18.
- ↑ Kovach JL. Unilateral choroidal macrovessel. JAMA Ophthalmol. 2016;134(3) . doi:10.1001/jamaophthalmol.2015.3678.
- ↑ Lima LH, Pimenta R, Zetta C. Multimodal imaging of choroidal macrovessel. J Fr Ophtalmol. 2020;43(5):371-372. doi:10.1016/j.jfo.2019.09.009.
- ↑ Kinoshita T, Mori J, Imaizumi H. Visual impairment associated with choroidal macroaneurysm in a patient with presumed anomalous short posterior ciliary artery. Am J Ophthalmol Case Rep. 2022 Nov 20;28:101755. doi: 10.1016/j.ajoc.2022.101755. PMID: 36439652; PMCID: PMC9694064.
- ↑ 20.00 20.01 20.02 20.03 20.04 20.05 20.06 20.07 20.08 20.09 20.10 20.11 20.12 Veronese C, Staurenghi G, Pellegrini M, et al. Multimodal Imaging in Vortex Vein Varices. Retin Cases Brief Rep. 2017;11(Suppl 1):163-165. doi:10.1097/ICB.0000000000000575
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 Gal-Or O, Dansingani KK, Sebrow D, et al. Inner Choroidal Flow Signal Attenuation in Pachychoroid Disease. Retina. 2018;38(10):1984-1992.
- ↑ 22.0 22.1 22.2 22.3 22.4 22.5 22.6 Wang T, Chan W, Tsai SH, Chen LJ. Clinical features of pachyvessels associated with polypoidal choroidal vasculopathy in chronic central serous chorioretinopathy. Sci Rep. 2021;11:13867.
- ↑ 23.0 23.1 23.2 23.3 23.4 Hilely A, Au A, Lee WK, et al. Pachyvitelliform Maculopathy: An Optical Coherence Tomography Analysis of a Novel Entity. Br J Ophthalmol. 2022;106(7):882-889.
- ↑ 24.0 24.1 24.2 24.3 24.4 Govetto A, Sarraf D, Scialdone A. "Hide and Seek" Neurosensory Retinal Detachments in Peripapillary Pachychoroid Syndrome Associated with Pulmonary Arterial Hypertension. Retin Cases Brief Rep. 2021;16(1):118-125.

