Chemical Peels of the Eyelids and Face
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Chemical peeling, also known as chemexfoliation, is a minimally invasive skin resurfacing procedure that rejuvenates and improves overall skin quality and appearance. A chemical peel consists of applying various combinations of ablative agents to promote collagen growth in the epidermal and dermal layers of the skin. On the face, its usage can lead to improvements in rhytids, hyperpigmentation, and scarring. Chemical peels can also be used in conjunction with surgical or laser blepharoplasty to maximize results. Completing chemical peels requires comprehensive patient evaluation and treatment management to minimize adverse effects and optimize outcomes.
Anatomy and Physiology
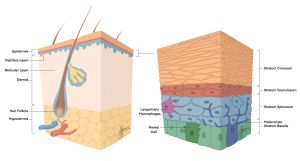
Figure 1: Anatomy of the skin. [1] The skin is composed of three layers: the epidermis, dermis, and hypodermis. The epidermis, the outermost layer, is a stratified squamous epithelium that is divided into four avascular layers: stratum corneum, stratum granulosum, stratum spinosum, and stratum basale. The dermis is composed of two layers of connective tissue: papillary layer, and reticular layer. The hypodermis, also known as the subcutaneous fascia, is the innermost layer and consists mainly of loose connective tissue and adipose tissue. Anatomic representation courtesy of Jerry Jose.
The skin remodeling effects of chemical peels depends on the depth of action of the chemicals used. For this reason, understanding and distinguishing the layers of the skin is crucial. The epidermis is a stratified squamous epithelium that consists of four avascular layers, which form a protective barrier against the external environment. The most superficial layer, the stratum corneum, is comprised of 10 to 30 layers of lipids, keratin, and dead keratinocytes, also known as anucleated squamous cells. This layer also contains terminally differentiated keratinocytes, known as corneocytes. The stratum corneum sheds frequently and is subsequently replaced by the keratinized layers below. Next is the stratum granulosum, followed by the stratum spinosum, both of which are composed of keratinocytes, which are the cells that produce keratin. The stratum spinosum also contains Langerhans macrophages, which are important for adaptive immune responses, and desmosomes that interlock to maintain the integrity of the cells. The fourth, and deepest, layer is the stratum basale and is composed of a single layer of cuboidal precursor stem cells. This layer contains melanocytes, which maintain skin pigmentation, and Merkel cells responsible for tactile sensation.
The dermis, which lies below the epidermis, is composed of two layers of connective tissue: the papillary and reticular layers. The upper, thinner papillary layer connects the epidermal and dermal layers through finger-like projections that intertwine with the stratum basale. The deeper, thicker reticular layer consists of bundles of collagen fibers and elastin, which maintain the tensile properties of the skin, including firmness and elasticity.
The hypodermis, commonly referred to as subcutaneous fascia, is the deepest layer of the skin. It mainly consists of loose connective tissue and adipose tissue, along with skin appendages, such as hair follicles, sensory neurons, and blood vessels.[2][3]
Treatment Plan
Chemical peels allow for controlled keratolysis (separation of epidermal keratinocytes) and keratocoagulation (clumping of keratinocytes into a thin layer on the surface of the skin) at the desired cutaneous depth. This allows for penetration of the chemical to promote regulated exfoliation and remodeling of the underlying layers of skin. The chemicals then denature proteins within the epidermal and dermal layers, resulting in the release of proinflammatory cytokines, which then initiate the inflammatory signaling cascade. The cascade ultimately culminates in the deposition of new dermal collagen and elastin, reorganization of structural scaffold proteins, and regeneration of keratinocytes.[4][3] The deposition of collagen and elastin, both major components of the extracellular matrix in connective tissue, improves skin plasticity, strengthens the dermis, and boosts skin firmness. The structural proteins maintain the appropriate spatial arrangement of elastin and collagen within the skin that provide its stretch and recoil function. Finally, the keratinocytes produce keratin, a type of fibrous protein, which supports the epidermal barrier.
Chemical peels can be used as on the eyelid skin for skin rejuvenation, alone or in combination with a surgical blepharoplasty.[5][6][7] Chemical peels can also be used to treat a variety of cutaneous conditions, including inflammatory disorders like acne vulgaris and rosacea, pigmentary disorders like melasma, and facial scarring.[8] They are also widely used for facial rejuvenation, epidermal reconstruction, and precancerous lesions, including treatment of rhytids and hyperpigmentation, reduced appearance of dilated pores, and actinic or solar keratoses, respectively.[2] Contraindications can include:
● history of allergic reactions to the peeling agents
● ongoing lacerations or infections of the peeling site, including herpes
● pregnancy or breastfeeding
● recent history of facial surgery or radiation therapy
A soft contraindication includes isotretinoin use in the past six months. Special consideration should also be given to individuals with psoriasis, atopic dermatitis, or connective tissue diseases, as well as those who are prone to keloid formation or poor wound healing, like in diabetes or immunosuppression.[9] Additionally, test spots can be recommended for patients at risk for hypo- or hyperpigmentation from chemical peels. In all patients receiving peels in the periocular area, special care should be taken to prevent products from entering the eye. In conjunction, preparations should be made for copious irrigation, should there be any ocular involvement or irritation.
Preparation/Ingredients
The spectrum of chemical agents used in peels is divided into light (superficial), medium, and deep subtypes depending on their depth of penetration. The pKa of the peeling agent, which is the pH at which 50% of the agent is in its free acidic state, correlates with the strength of the peel. pKa ranges from -5 to 50, where compounds with lower pKas ionize more easily and are usually stronger acids. The most commonly available agents are as follows (in order from weakest to strongest).[10][2]
- Alpha hydroxy acids (AHA, pKA 3.4-3.9) are organic carboxylic acid compounds that have a hydroxyl group substitution on the alpha carbon. Commonly used AHAs include glycolic acid, lactic acid, and citric acid.
- Beta hydroxy acids (BHA, pKa 2.3-3.0) are organic compounds that contain a carboxylic acid functional group and a hydroxyl group attached to the second carbon. These agents are more lipophilic than AHAs, which allow for better penetration through the skin. The most common BHA compound is salicylic acid (pKa 2.97), which is an ingredient in the Jessner solution. Jessner solution is widely used for its milder effects on the skin and is composed of 14% resorcinol (a phenol derivative), 14% salicylic acid, and 14% lactic acid mixed in ethanol. Other BHA compounds include lipohydroxy acid, a lipophilic derivative of salicylic acid, and pyruvic acid (pKa 2.39).
- Trichloroacetic acid (TCA, pKA 0.26) is an analog of acetic acid and has varying effects as a peeling agent, depending on the concentrations used.
- Phenol (pKa 10) is an aromatic organic compound used in deeper chemical peels due to its highly penetrative effects. Although its pKa is higher, it is a stronger acid than other compounds due to the resonance stabilization of its conjugate base (electron movement results in a more stabilized form of the molecule). It is usually mixed with croton oil, a compound used in varying concentrations with phenol to penetrate layers of skin, in order to produce uniform keratocoagulation. Commonly used solutions made with phenol include Baker-Gordon and Hetter’s formulas. Hetter’s formula differs from Baker-Gordon in that it includes croton; this takes advantage of the ability for croton oil to decrease the concentration of phenol required. Higher concentrations of TCA (>50%), used in deep peels, presents a frosting pattern on the skin, and should be used with caution due to increased risk for post-inflammatory hyper- or hypopigmentation and scarring.
Light peels use 20-30% TCA, Jessner solution, or 40-70% glycolic acid to injure the epidermis and the dermal-epidermal interface.[2] Light peels have the fastest healing time, with epidermal regeneration usually occurring within three to five days. Due to their mild effects, these peels can be used on most skin types to rejuvenate the skin and are used to treat fine wrinkles, acne, hyperpigmentation, and actinic keratosis.[9] Since light peels only mildly disrupts the skin, there is minimal risk of developing hyper- or hypopigmentation as an adverse effect.
Medium peels use combinations of 35% TCA with either Jessner’s solution or 70% glycolic acid.[2] Since these agents penetrate the skin more deeply, the healing process is more prolonged, usually requiring up to seven days. Medium peels have an increased risk for hyper- or hypopigmentation and must be used with caution on individuals with dark skin tones.[9] Like light peels, medium peels are also used to reduce wrinkles, hyperpigmentation, dryness, and erythema.[11]
Deep peels use 50% or greater TCA concentrations or croton-phenol combinations to rapidly denature keratinocytes and penetrate as deep as the reticular dermis.[2] Due to the extensive effects, deep peels are performed in surgical settings to improve patient comfort and require a significant healing time of two months or more. Additionally, because of the cardiotoxic properties of phenols, the patient’s cardiopulmonary function must be monitored continuously during the procedure. This includes intermittent or continuous monitoring of cardiac activity and oxygen saturation using electrocardiograms (ECG) and pulse oximeters, respectively. Other complications of phenols include hypo- or hyperpigmentation, scarring, and keloid formation. Recent advancements in technology have introduced laser resurfacing as an alternative or an addition to deep peels (See Eyewiki article on Laser Resurfacing of the Eyelids and Face[12]). [9]
Deep peels are typically avoided in the periorbital area due to the increased risk for cicatricial ectropion. Lower eyelid ectropion, or eversion of the eyelid, has been reported in patients who undergo phenol-based (deep) peels in conjunction with blepharoplasty.[6] Studies have found that light and medium depth peels, conducted with varying combinations of TCA, are better for eyelid procedures.[6]
Procedural Steps
Before beginning the peeling process, it is important to determine the appropriate depth of peel for a patient. To do so, the Fitzpatrick classification is commonly used to classify the skin phototype based on their reaction to sun exposure. The six categories are as follows. [13]
| Skin Type | Typical Features | Tanning Ability |
| Type I | Very pale white skin, blue/green eyes, freckles, blond/red/light hair | Skin burns easily with sun exposure, does not tan |
| Type II | Pale skin, blue/green/hazel eyes, blond/red/light hair | Skin burns frequently with sun exposure, tans with difficulty |
| Type III | White skin, blue/hazel/brown eyes, brown hair | Skin sometimes mildly burns with sun exposure, tans gradually |
| Type IV | Light brown (typically Mediterranean Caucasian) skin, brown hair, brown eyes | Skin burns minimally with sun exposure, tans easily |
| Type V | Brown (typically Middle Eastern) skin, brown eyes, dark brown/black hair | Skin rarely burns with sun exposure, tans very easily |
| Type VI | Dark brown/black skin, brown eyes, dark brown/black hair | Skin almost never burns with sun exposure, tans very easily |
The best candidates for medium or deep peeling are patients classified as Fitzpatrick I. Patients classified as Fitzpatrick III-VI are susceptible to aberrant pigmentation or dyschromia with more invasive forms of peeling.
Glogau classification is another way to categorize skin based on levels of photoaging. The four categories are as follows.[14]
| Group | Classification | Typical Age | Description |
| I | Mild | 28-35 | No wrinkles |
| II | Moderate | 35-50 | Wrinkles in motion (smile lines) |
| III | Advanced | 50-65 | Wrinkles at rest |
| IV | Severe | 60-75 | Widespread wrinkles |
After the skin is classified, some physicians choose to perform pre-peel spot testing to confirm the appropriate peel for the patient. The next step can be to prime the skin, which begins 2-4 weeks before the peel. To prime the skin, a topical agent, such as all-trans retinoic acid/tretinoin (0.025-0.05%) cream, salicylic acid (5-10% concentration), or glycolic acid (5-10% concentration), is applied daily to attenuate the stratum corneum layer and increase the depth of penetration.
The chemical peeling procedure begins by cleansing the patient’s skin of any residue and makeup with a degreasing agent, such as isopropyl alcohol or acetone. The patient should be in a supine position with the head of the bed elevated to 45 degrees and a hair cap worn to keep hair away from the procedural field. Petroleum jelly is sometimes applied to areas of potential pooling, like the nasolabial folds and lateral canthi. Additionally, the eyes should be covered with the appropriate shield. Although general anesthesia is not routinely required, oral analgesics may be administered.
The peeling agent is applied to the thicker regions of skin first, which includes the chin, nose, cheeks, and forehead, before moving onto thinner regions, like the areas around the eyes and mouth. Experience is required to master the nuances of applying the peeling agent, such as preventing overlaps in brushstrokes to avoid overconcentration of product and stretching wrinkled skin to ensure even coating.
After the peel is applied, cool saline compresses help to neutralize the solution and to increase patient comfort. To facilitate healing, “vinegar soaks” with 0.25% acetic acid can be used, followed by the application of a non-scented, bland emollient 3-5 times per day. [9]
Recovery and Maintenance
For each of these peels, the duration of treatment, including how long the products are applied for during each session and the number of peeling sessions needed to see desired effects, varies from person to person, depending on the unique characteristics of their skin. The recovery period, that is the time from when the chemical peel is performed to the complete re-epithelialization of the skin, varies for each type of peel. For light peels, this ranges from three to four days, while for medium and deep peels, it may take up to eight and fourteen days, respectively. Due to the varying penetrative depths of each peel, the post-treatment results also vary. The therapeutic benefits of light peels only last for up to two months, therefore, requiring regular maintenance treatments to see complete revitalization of the skin. The benefits of medium depth peels may last for up to four months post-treatment and depending on the goals of treatment, may require continuous therapy to see desired results. Deep peels, which are the most invasive of these procedures, may produce results that last up to ten years and do not require maintenance treatments. [7] For all procedures, patients should take extreme care to avoid damaging the skin until the desquamation and re-epithelialization process is complete. This includes avoiding abrasive products and practices, including application of makeup, during the healing process, as well limiting sun exposure for at least one month after the procedure. Applying sunscreen to protect the skin from sun damage post-procedure and avoid compromising therapeutic benefits must be reemphasized.
Conclusion
Due to the complexity of chemexfoliation, all treatment plans should be constructed in consultation with healthcare professionals. This is particularly important as the goals of treatment vary between patients, and the expertise of physicians will be fundamental in navigating the nuances of the procedure to ensure the best results for each person. Moreover, relying on the clinical experience of professionals will help to avoid complications that may arise from improper technique and methodology.
References
- ↑ Jose, J. (2022, August). Anatomy of the Skin.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Soleymani, T., Lanoue, J., & Rahman, Z. (2018, August). A Practical Approach to Chemical Peels: A Review of Fundamentals and Step-by-step Algorithmic Protocol for Treatment. The Journal of Clinical and Aesthetic Dermatology, 11(8), 21–28.
- ↑ 3.0 3.1 Yousef, H., Alhaji, M., & Sharma, S. (2021, November 19). Anatomy, Skin (Integument), Epidermis. StatPearls Publishing.
- ↑ O’Connor, A., Lowe, PM., Shumack, S., & Lim, A. (2017, October 24). Chemical Peels: A Review of Current Practices. Australasian Journal of Dermatology, 59(3), 171-181.
- ↑ Cho, I. (2013, September 13). Aging Blepharoplasty. Archives of Plastic Surgery, 40(5), 486-491.
- ↑ 6.0 6.1 6.2 Dailey, RA., Gray, JF., Rubin, MG., Hildebrand, PL., Swanson, NA., Wobig, JL., Wilson, DJ., & Speelman, P. (1998, January). Histopathologic Changes of the Eyelid Skin Following Trichloroacetic Acid Chemical Peel. Ophthalmic Plastic Reconstructive Surgery, 14(1), 9-12.
- ↑ 7.0 7.1 Obagi, S. (2022, March). Chemical Peels: Principles, Peeling Agents, and Pretreatment Assessment. UpToDate.
- ↑ Rendon, MI., Berson, DS., Cohen, JL., Roberts, WE., Starker, I., & Wang, B. (2010, July). Evidence and Considerations in the Application of Chemical Peels in Skin Disorders and Aesthetic Resurfacing. The Journal of Clinical and Aesthetic Dermatology, 3(7), 32-43.
- ↑ 9.0 9.1 9.2 9.3 9.4 Samargandy S. & Raggio BS. (2021, July 25). Skin Resurfacing Chemical Peels. StatPearls Publishing.
- ↑ O’Connor, A., Lowe, PM., Shumack, S., & Lim, A. (2017, October 24). Chemical Peels: A Review of Current Practices. Australasian Journal of Dermatology, 59(3), 171-181.
- ↑ Naik, MN., Honavar, SG., Das, S., Desai, S., & Dhepe, N. (2009). Blepharoplasty: An Overview. Journal of Cutaneous and Aesthetic Surgery, 2(1), 6-11.
- ↑ Barmettler, A., Yen, MT., Yi, JK. (2022, April 6). Laser Resurfacing of the Eyelids and Face. EyeWiki.
- ↑ Wright, Caradee. (2015, May). Real-time measurement of outdoor worker’s exposure to solar ultraviolet radiation in Pretoria, South Africa. South African Journal of Science, 111(5/6).
- ↑ Faghihi, G. Fatemi-Tabaei, S., Bbtahi-Naeini, B., Siadat, A. H., Sadeghian G., Nilforoushzadeh, M. A., Mohamadian-shoeili H. (2017, February 15) The Effectiveness of a 5% Retinoic Acid Peel Combined with Microdermabrasion for Facial Photoaging: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Dermatology Research and Practice, 2017;2017:8516527.