Cataract Surgery Training
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
For a long time, training in ophthalmic surgery was based on Halsted's methodology [1][2]. In this type of teaching, the resident should: have intense and repetitive opportunities to care for patients under the supervision of a qualified surgeon; gain an understanding of the scientific basis behind the disease that requires surgical treatment; and develop the ability to perform operations of increasing complexity [3]. In addition, only those who accomplished a predetermined number of procedures were considered able to perform it [1]. However, currently, this methodology is losing space to new training techniques based on Wet Labs and virtual reality simulators [4], since learning based only on the number of procedures performed and on direct practice with the patient has some limitations and risks. Among these limitations, we can mention the inconsistency in the level of skill acquired due to the variation in training opportunities, and among the risks, the patient's exposure to an inexperienced surgeon [1]. These modern methodologies for teaching microsurgery in ophthalmology allow residents to practice safely. Additionally, they enable the shortening of the learning curve and reduce the possibility of adverse events in practice [2][4][5].
Currently, a competent surgeon is defined as one who is able to “successfully apply professional knowledge, skills and attitudes” [6]. To assess competencies in cataract surgery, the International Council of Ophthalmology has developed the ICO-Ophthalmology Surgical Competency Assessment Rubric: Phacoemulsification methodology (ICO-OSCAR: Phaco) . The Council suggests applying the ICO-OSCAR to monitorate the resident’s learning process [7]. However, many countries still do not adopt it and prefer only the number of procedures performed as a parameter for acquisition of aptitude.
In the United States, the ACGME (Accreditation Council for Graduate Medical Education) requires 86 cataract surgeries per resident over the 3 years [8]. However, the country has been migrating from a model based on quantity to one based on developed competences [9]. Meanwhile, in Brazil, a developing country, the Brazilian Council of Ophthalmology requires at least 150 eye surgeries of any kind, whether cataract surgeries or not [8]. In Europe, education in ophthalmologic surgery in countries participating in the EBO (European Board of Ophthalmology) is decentralized [9], which means that each country follows a model that it finds best suited. Finally, some countries still find it difficult to train their ophthalmologists. In sub-Saharan Africa, for example, a survey published in 2019 found that the average number of procedures performed by second-year ophthalmology residents was zero [10]. In this sense, despite technological advances, the teaching of cataract surgery is quite heterogeneous around the world.
Modern training techniques
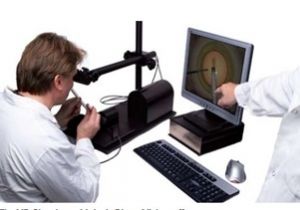
There are several areas in which training in simulated situations is part of both the learning and the improvement process. From airplane pilots, who spend hours in simulators before taking over an aircraft, to musicians, who rehearse incessantly before a performance, repetition is extremely important for acquiring the motor proficiency necessary to exercise certain skills. In view of this, there would be no reason to be different in learning surgical techniques, which stimulated the emergence of simulators capable of creating a controlled scenario both for training and for the assessment of acquired skills. Currently, the most popular cataract surgery simulators available are Eyesi (VRmagic) (Fig. 1), PhacoVision (Melerit Medical) (Fig. 2) and MicrovisTouch (ImmersiveTouch) (Fig. 3) [11][12]. PhacoVision (Melerit Medical) has a unique focus on phacoemulsification and capsulorhexis procedures [12], while MicrovisTouch (ImmersiveTouch) has only the module in capsulorhexis [11]. Both simulators still have few published studies that support their use for educational purposes [2][11]. On the other hand, Eyesi (VRmagic) is the most complete among the three and has several publications that indicate a positive association between its use in learning cataract surgery and the reduction of errors during surgical procedures involving patients [1][2][5][11][13].
A systematic review published in 2020 in the BMJ Open Ophthalmology by Ahmed et al [5] assessed the effectiveness of virtual reality simulators in improving the teaching of cataract surgery. 165 articles published between 2012 and 2019 were selected for an initial analysis, but only 10 met the inclusion criteria. The systematic review required studies that were able to provide qualitative results that assessed the effects of the Eyesi simulator (VRmagic) on surgical training. One of the articles reviewed was that by Ferris et al [14], who conducted a retrospective cohort study among first-year and second-year residents. Rates of posterior capsular rupture (PCR) in 29 NHS Ophthalmology Units between 2009 and 2015 were analyzed. The result obtained was a 38% lower PCR rate among residents who had access to training at Eyesi (VRmagic) in relation to those who did not have [14]. Another relevant article was the one by Staropoli et al [15] who compared the rates of surgical complications between 11 residents who trained on the Eyesi (VRmagic) and 11 residents who did not train on the simulator, all of whom were first-year ophthalmology students of the same institution. The result was a complication rate of 2.1% for the group that trained on the simulator compared to 5.1% for the group that did not train on the simulator [15]. The systematic review by Ahmed et al [5] concluded that training in the Eyesi simulator (VRmagic) is effective in reducing the rates of surgical complications.
The Eyesi simulator (VRmagic) has training modules in capsulorhexis, hydrodissection, phacoemulsification, irrigation/aspiration, IOL insertion and in managing complications [16]. During virtual surgery, instruments such as forceps, viscoelastic cannula, cystotome and phacoemulsification tip are available for virtual immersion to be performed [16]. Its software is capable of storing resident performance metrics, allowing a score to be generated, as well as feedback [1], which expands its use in skill acquisition assessment contexts. Several ophthalmology residency programs around the world use these modern simulators as a form of training for their residents [17]. Among them, we can mention the retina fellowship at the Université de Montréal (Canada) and the residency in ophthalmology at UNESP (Brazil), which only authorize physicians to practice surgeries after reaching predetermined benchmarks in the Eyesi simulators (VRmagic) as a way to increase patient safety. Despite all the advantages that simulators add to the teaching of cataract surgery, their high cost may end up being a limiting factor for their expansion of use. Depending on the model, an Eyesi simulator (VRmagic) can cost between $100,000 and $200,000 [18]. As a result, only locations that have more favorable economic conditions can acquire it, contributing to the heterogeneity of teaching cataract surgery around the world.
Wet lab
Wet lab is a type of laboratory in which its entire structure is focused on the handling and experimentation of biological materials, being an aid tool when it comes to teaching cataract surgery techniques, as it provides a safe way to acquire basic motor skills and to learn the name and the function of the instruments used [19]. In view of this, the ACGME Common Program Requirements considers surgical training in simulated environments essential for the training of ophthalmology residents [20].
According to Henderson et al [19], an ideal wet ophthalmic laboratory should contain “enough space for at least 2 people (student and teacher), a surgical microscope, a phacoemulsification machine, a table to place the eye, a sink with a supply of water, and a storage space", in addition the incorporated supplies would include" 2 sets of surgical instruments, blades, an ophthalmic viscosurgical device (OVD), irrigation solution and tubing for the phacoemulsification machine, irrigation/aspiration tips, lenses intraocular (IOLs), sutures, gloves, biohazard disposal containers and sharps disposal containers”. Several types of eyes can be used to practice surgical procedures, varying from synthetic eyes to the eyes of human and animal cadavers [19], each one having its advantages and disadvantages.
Animal Eye Models
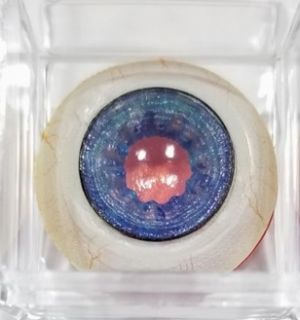
A wide variety of biologically derived eyes can be used during wet lab training sessions. Human cadaver eyes are the best model for training eye surgery [19], but their availability in eye banks and the high costs related to their acquisition end up causing many residency programs to seek more accessible ways to teach these types of surgeries. In this context, the eyes of animals such as pigs, goats, sheep and rabbits end up being viable options both for studies and for the simulation of surgical procedures in wet labs [19][21][22][23]. A systematic review published in 2020 [1] evaluated 16 studies that described models of materials that could be used in wet labs aimed at teaching cataract surgery. The authors highlighted the use of pig eyes to teach phacoemulsification [24] and rabbit eyes to teach the capsulorhexis process [21] as the ones with the most evidence of efficiency for training these procedures [1]. Pig eyes are more accessible than rabbit eyes in several Western countries, as they can be easily acquired in butchers or slaughterhouses, which makes their use more common in wet labs [19]. However, in countries like Sudan, a largely Islamic nation, pig eyes cannot be used for religious reasons [25]. In countries like India, where goat eyes are extremely cheap, there is a great stimulus for the development of studies on their use in wet labs [22].
As porcine eyes are the most used during cataract surgery training, here are some comparisons between them and human eyes. Although anatomically similar, the anterior capsule of a pig's eye available for wet labs is significantly more viscous and elastic [19]. This is because the minimum age for slaughtering pigs is 5 months. Thus, the anterior capsule of pig eyes available for wet lab tends to be younger and the capsulotomy becomes similar to a pediatric capsulotomy rather than a usual adult capsulotomy [19]. However, there are manipulations that can be made in the ocular structure so that it is possible to better simulate an elderly person's eye [19]. As the lens of pig eyes at birth is normally translucent, there is a need to induce a cataract by chemical or physical compounds, which can eventually end up opacifying the cornea and making it difficult to visualize the cataract [19]. It is worth noting that in some countries, such as Brazil, sanitary legislation requires that all pigs be submerged in a boiler with scalding water before any organ is removed; this ends up producing thermal injuries to the cornea, rupture of the lens capsule and even partially inducing cataracts in a non-homogeneous way, reducing the quality of eyes available for wet lab from this type of animal.
Several advances are taking place in terms of better adequacy of the use of animal eyes for teaching cataract surgery around the world. Among them, we can mention the preparation of the eye, the induction of cataracts, the development of eye positioning devices, among others. In addition, it is noteworthy that there are several companies that are investing in the development of synthetic eye models, as they have some advantages over biological materials.
Synthetic Eye Models
Unlike animal eye models, artificial eyes have some advantages such as the possibility of using the same eye several times to perform the same procedure, the predictability of simulating certain specific situations and the possibility of reusing surgical instruments in humans. On the other hand, this type of resource ends up being restricted to those places that have greater financial power, as its cost is relatively high compared to the eyes of animals. The SimulEYE company has as one of its products the SimuloRhexis (Fig. 4), a synthetic eye model that was developed specifically for the training of capsulorhexis. A kit allows 5 to 10 capsulotomies to be performed, ranging in price from $50 to $85 [26]. Bioniko Models, on the other hand, has products that allow specific situations to be simulated, one of them being the OKULO BROWN 8 (Fig. 5) which enables training in the management of cataract surgery complications [27]. In addition to it, the company also markets the OKULO BLUE 5 (Fig. 6) which was specifically developed for training in iris suture [28]. Both models cost $75 a unit and can be used only once. Last but not least, the Kitaro Eye company has a wide variety of products sold in the form of kits for both dry labs and wet labs. The great advantage of their synthetic eyes is that they make it possible to use the anterior capsule and cores more than once. A kit (Fig. 7) can range between $995 and $1600 [29].
As mentioned in the article by Henderson et al [19], instruments used in animal eyes should not be reused in human surgeries, as this creates the risk of biological contamination occurring. One of the risks is that the patient may acquire Creutzfeldt-Jakob Disease (CJD), a type of encephalopathy that can be transmitted when medical procedures are performed with contaminated materials or instruments that have been used inadvertently (called iatrogenic CJD) [30]. One of the advantages of synthetic eye models is that this risk of biological contamination does not exist, which allows the instruments to be reused in humans.
The advantages of artificial eyes over animal eyes in cataract surgery training are numerous, but what will dictate which option a residency program chooses will be the institution's financial power and the availability in the region of animal or human eyes that meet their needs. For these and other factors analyzed in the text, the teaching of cataract surgery around the globe is extremely heterogeneous and varies according to the resources, culture and demands of each location.
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Sikder S, Tuwairqi K, Al-Kahtani E, Myers WG, Banerjee P. Surgical simulators in cataract surgery training. Br J Ophthalmol. 2014;98(2):154-158. doi:10.1136/bjophthalmol-2013-303700
- ↑ Jump up to: 2.0 2.1 2.2 2.3 Lee R, Raison N, Lau WY, et al.. A systematic review of simulation-based training tools for technical and non-technical skills in ophthalmology. Eye. 2020;34(10):1737-1759. doi:10.1038/s41433-020-0832-1.
- ↑ 100 years of surgical education: The past, present, and future | The Bulletin. Accessed August 28, 2021. https://bulletin.facs.org/2013/07/100-years-of-surgical-education/
- ↑ Jump up to: 4.0 4.1 Alwadani S. Cataract surgery training using surgical simulators and wet-labs: Course description and literature review. Saudi J Ophthalmol. 2018;32(4):324. doi:10.1016/J.SJOPT.2018.01.003
- ↑ Jump up to: 5.0 5.1 5.2 5.3 Ahmed TM, Hussain B, Siddiqui MAR. Can simulators be applied to improve cataract surgery training: a systematic review. BMJ Open Ophthalmol. 2020;5(1):488. doi:10.1136/BMJOPHTH-2020-000488
- ↑ NI B, CW C. Competency in surgical residency training: defining and raising the bar. Acad Med. 2007;82(6):569-573. doi:10.1097/ACM.0B013E3180555BFB
- ↑ Golnik KC, Beaver H, Gauba V, et al. Cataract Surgical Skill Assessment. Ophthalmology. 2011;118(2):427-427.e5. doi:10.1016/J.OPHTHA.2010.09.023
- ↑ Jump up to: 8.0 8.1 Soriano ES. Cataract surgery teaching. Arq Bras Oftalmol. 2015;78(4):V-VI. doi:10.5935/0004-2749.20150053
- ↑ Jump up to: 9.0 9.1 Muttuvelu D V., Andersen CU. Cataract surgery education in member countries of the European Board of Ophthalmology. Can J Ophthalmol. 2016;51(3):207-211. doi:10.1016/J.JCJO.2016.04.006
- ↑ Dean W, Gichuhi S, Buchan J, et al. Survey of ophthalmologists-in-training in Eastern, Central and Southern Africa: A regional focus on ophthalmic surgical education. Wellcome Open Res. 2019;4. doi:10.12688/WELLCOMEOPENRES.15580.1
- ↑ Jump up to: 11.0 11.1 11.2 11.3 Oflaz AB, Köktekir BE, Okudan S. Does Cataract Surgery Simulation Correlate with Real-life Experience? Turkish J Ophthalmol. 2018;48(3):122. doi:10.4274/TJO.10586
- ↑ Jump up to: 12.0 12.1 Wallace BS, Sabates NR. Simulation in Ophthalmology. Mo Med. 2013;110(2):152. Accessed October 7, 2021. /pmc/articles/PMC6179658/
- ↑ McCannel CA, Reed DC, Goldman DR. Ophthalmic Surgery Simulator Training Improves Resident Performance of Capsulorhexis in the Operating Room. Ophthalmology. 2013;120(12):2456-2461. doi:10.1016/J.OPHTHA.2013.05.003
- ↑ Jump up to: 14.0 14.1 JD F, PH D, RL J, B B, M O, JM S. Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: report 6. The impact of EyeSi virtual reality training on complications rates of cataract surgery performed by first and second year trainees. Br J Ophthalmol. 2020;104(3):324-329. doi:10.1136/BJOPHTHALMOL-2018-313817
- ↑ Jump up to: 15.0 15.1 Staropoli PC, Gregori NZ, Junk AK, et al. SURGICAL SIMULATION TRAINING REDUCES INTRAOPERATIVE CATARACT SURGERY COMPLICATIONS AMONG RESIDENTS. Simul Healthc. 2018;13(1):11. doi:10.1097/SIH.0000000000000255
- ↑ Jump up to: 16.0 16.1 Eyesi Surgical – Haag-Streit Simulation. Accessed October 7, 2021. https://www.vrmagic.com/medical-simulators/eyesi-surgical
- ↑ McCannel CA. Simulation Surgical Teaching in Ophthalmology. Ophthalmology. 2015;122(12):2371-2372. doi:10.1016/J.OPHTHA.2015.08.036
- ↑ CRSToday | The Eyesi Ophthalmic Surgical Simulator. Accessed October 7, 2021. https://crstoday.com/articles/2008-may/crst0508_20-php/
- ↑ Jump up to: 19.00 19.01 19.02 19.03 19.04 19.05 19.06 19.07 19.08 19.09 19.10 Henderson BA, Grimes KJ, Fintelmann RE, Oetting TA. Stepwise approach to establishing an ophthalmology wet laboratory. J Cataract Refract Surg. 2009;35(6):1121-1128. doi:10.1016/J.JCRS.2009.01.027
- ↑ Common Program Requirements. Accessed October 7, 2021. https://www.acgme.org/What-We-Do/Accreditation/Common-Program-Requirements/
- ↑ Jump up to: 21.0 21.1 Ruggiero J, Keller C, Porco T, Naseri A, Sretavan DW. Rabbit models for continuous curvilinear capsulorhexis instruction. J Cataract Refract Surg. 2012;38(7):1266. doi:10.1016/J.JCRS.2012.01.034
- ↑ Jump up to: 22.0 22.1 Dada VK, Sindhu N. Cataract in enucleated goat eyes: Training model for phacoemulsification. J Cataract Refract Surg. 2000;26(8):1114-1116. doi:10.1016/S0886-3350(00)00448-X
- ↑ Kayikçioǧlu Ö, Eǧrilmez S, Emre S, Erakgün T. Human cataractous lens nucleus implanted in a sheep eye lens as a model for phacoemulsification training. J Cataract Refract Surg. 2004;30(3):555-557. doi:10.1016/J.JCRS.2003.08.018
- ↑ A M, J N, J N, H H, T K, K K. Cataract surgery training using pig eyes filled with chestnuts of various hardness. J Cataract Refract Surg. 1999;25(5):622-625. doi:10.1016/S0886-3350(99)00003-6
- ↑ Dean WH, Buchan JC, Gichuhi S, et al. Ophthalmology training in sub-Saharan Africa: a scoping review. Eye 2020 354. 2020;35(4):1066-1083. doi:10.1038/s41433-020-01335-7
- ↑ SimuloRhexis — SimulEYE®. Accessed October 7, 2021. https://www.simuleye.com/products/simulorhexis-kit
- ↑ OKULO BROWN 8 (BR8) - CATARACT & COMPLICATIONS – BIONIKO. Accessed October 7, 2021. https://bioniko.myshopify.com/collections/cataract/products/okulo-brown-8-br8
- ↑ OKULO BLUE 5 (BL5) IRIS SUTURING – BIONIKO. Accessed October 7, 2021. https://bioniko.myshopify.com/collections/cataract/products/okulo-blue-5-bl5
- ↑ Quotation made with a Kitaro representative in 2018 after contacting them through the website https://www.kitaroeye.com/
- ↑ Doença de Creutzfeldt-Jakob (DCJ) - Distúrbios cerebrais, da medula espinal e dos nervos - Manual MSD Versão Saúde para a Família. Accessed October 7, 2021. https://www.msdmanuals.com/pt-br/casa/distúrbios-cerebrais,-da-medula-espinal-e-dos-nervos/doenças-causadas-por-príons/doença-de-creutzfeldt-jakob-dcj
Observation: Ana Vega and Gustavo Correia worked together on this publication and contributed equally to it.