Cataract Surgery Following Radial Keratotomy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Background Cataract surgery in the context of prior radial keratotomy (RK) presents challenges in peri-operative planning, surgical execution and post-operative refractive expectations. An understanding of corneal biomechanics, wound healing, refractive power and complex biometric assessment is required to elevate the chances of safe surgical success and satisfactory outcomes.
Cataracts describe a multi-factorial change to the eye's lens system inducing optical changes, visual degradation and effect on quality of life among other secondary effects. This pathology remains a continued significant burden to the world population even in modern times.[1]
Radial Keratotomy Though the concept of radial keratotomy for altering corneal biomechanics and refractive state has approached near a century since Sato's [2] publication of the described procedure (on the posterior cornea), it wasn't until the latter 20th century when the popularity of the procedure took off being performed on the order of millions worldwide extending into the 1990s as well. As scientific analysis and clinical studies continued to accrue ,[3] the popularity of RK as a primary refractive treatment has since waned with procedures using LASER in different forms (excimer and femtosecond) and lens based treatments taking the forefront in the refractive surgery arena. As the patient population that had received RK aged, treatment of senescent processes, particularly cataract, became a meaningfully challenging venture reinvigorating the need to understand cornea physiology, pathology, wound healing and optics became evident as traditional assessments and methods of treatment had unsatisfactory results.
Prospective Evaluation of Radial Keratotomy (PERK) study: This study was performed in 1982 and inclusion criteria was for myopic patients with a refractive error ranging from -2.00D to -8.75 D. At 10 years the PERK study demonstrated that 43% of post-op patients between 6 months to 10 years developed a hyperopic shift of at least 1.00D. Between 6 months-2 years post-op, patient's averaged a +0.21 D/year hyperopic shift, but this rate decreased to 0.06 D/year by the 2-10 year post-op time frame. The significance of this study demonstrated that a hyperopic shift occurred throughout the duration of the entire 10 years after surgery, which should be accounted for during future surgical planning. A greater hyperopic shift was found in patients with smaller optical zones. Furthermore the PERK study demonstrated a diurnal fluctuation mean myopic shift 0.31 +/- 0.58 D from the morning to evening.
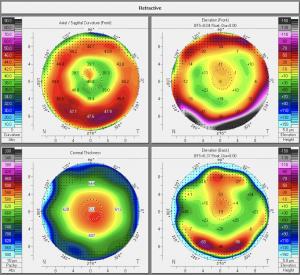
Challenges for IOL Calculation: RK changes the curvature of the central cornea and it’s overall topography where the cornea is flat centrally and steeper in the periphery. Standard topography can overestimate central corneal power which results in a post-operative hyperopic surprise. Central corneal power is not the real corneal power required for IOL calculations. Instead we need to find the effective corneal power.
Method
Symptoms and Signs
Pre-operative assessment requires additional attention to details at all levels compared to standard cataracts surgery starting all the way in the beginning with the first assessment as described by a standard chief complaint and history of present illness. For eyes with numerous incisions (e.g. 16 cut RK) fluctuation in vision can be a concerning symptom given the known effects of bio-mechanical weakening and secondary refractive effects that can be influenced by factors such as time of day, altitude and sleep cycles.
For cases where vision fluctuates over the course of a 24 hour cycle, timing of when to perform exams and ancillary testing can be challenging. Diurnal fluctuation occurs as a result of hypoxia from lid closure during sleep which creates edema within the incisions and subsequent hyperopic shift upon awakening. This hypoxic edema resolves throughout the day, and by the evening causes on average a myopic shift of 0.31D.[3] Some surgical cases go as far as warranting exams and measurements intentionally at different times of the day and detailed counseling on the refractive shifts and outcomes that will still be present after cataract treatment. Though some case series report limited success of stabilizing biomechanics of corneas with RK [4], such tailored control of wound healing and which areas preferentially tighten may be challenging as certain wounds could gape in comparison to non-incised corneal areas based on the amount of epithelial plugging.
Given that cataracts only further aberrate post RK corneas, deciding the relative role of each on symptoms may be driven by the ability to perform diagnostic rigid contact lens fitting (particularly for new evaluations). For corneas with high number of incisions that result in very flat corneas, reverse geometry lenses (flatter in the center with some peripheral vaulting) may help in determine sources of decreased vision.
Formulae
Double K Formulas: Utilize various algorithms (SRK/T, Holladay or Hoffer Q) based on K value and axial length to determine effective lens position (ELP). Pre-RK Ks are used for correct ELP and post-RK Ks are used for corneal power.
1) True K RK algorithm
2) DK-Holladay-IOLM
3) Potvin-Hill
Among the Double K formulae True K method has been shown in some studies to have the lowest mean error especially when combined with partial history.[5] When no refractive history is available True K (No History) and unadjusted Haigis were most accurate.
Haigis formula: ELP calculated using axial length and AC depth.
Historical Method
This method is most useful when pre-RK refraction and keratometry readings are available. Of note this method may be confounded by progressive hyperopia after RK and myopic shift from nuclear sclerosis,.
Requirements:
1) Pre-RK Keratometry to calculate mean K
2) Pre-RK Refraction
3) Post-RK refraction
Formula
Effective Corneal Power (Post-RK) = (Pre-RK Mean K) - (Change in spherical equivalent at corneal plane)
Myopic Correction: This value should ideally be taken a few years after RK stabilizes, however before myopia is induced by cataract formation. This is calculated by taking the difference between the Pre-RK refraction and Post-RK refraction and converting to the power at the corneal plane. The effective corneal power can now be used for the K value in IOL calculations.
Example
Pre-RK Keratometry Mean K: Steep K (45D ) + Flat K (43D) = Mean K is (44D)
Change in spherical equivalent at corneal plane: Pre-RK refraction (-6.5D), Post-RK refraction (-0.5D). The surgical correction is 6 D at the spectacle plane. Correcting for a presumed vertex distance of 12mm using the vertex formula: Fc = F / (1-xF)
Fc (Power at corneal plane)
F(Power at spectacle plane)
x (change in vertex distance in meters)
Fc = 6/ (1 - 0.012 x 6) = 5.6 D or ~5.5 D at the corneal plane
Alternatively you can estimate the change by adding 0.25 D for 2D change in power after 4D:
| 4.00 D +0.25 D |
| 6.00 D +0.50 D |
| 8.00 D +0.75 D |
| 10.00 D +1.00 D |
| 12.00 D +1.25 D |
| 14.00 D +1.50 D |
Effective Corneal Power: 44D - 5.5 D = 38.5 D.
Double K Formulae
1) True K Method
2) DK-Holladay-IOLM (requires IOL Master)
-Modified Double-K (DK) formula using a presumed pre-RK K of 43.86 to calculate ELP and a post-RK K (from IOL master or Lenstar) to calculate corneal refractive power
3) Potvin-Hill (Requires use of Oculus Pentacam)
Final IOL Power = Holladay 1 IOL Calculation - 4.4554 + 0.0084 x CTmin
CTmin: Minimum Central Thickness. Calculated by taking thinnest local pachymetry in microns from Oculus Pentacam Topometric Display
American Society of Cataract and Refractive Surgery: IOL power calculator for eyes with prior RK
Link: https://iolcalc.ascrs.org/wbfrmCalculator3.aspx
1) Effective Refractive Power (EyeSys Topography)
-Effective Refractive Power (EffRP) used as the central corneal power by taking all points in the central 3mm and applying this for IOL power calculation.
2) Average Central Power
3) Atlas 1-4 (Zeiss Humphrey Atlas topographer)
-Averages annular powers on the Numerical View at 1mm, 2mm, 3mm, and 4mm to calculate average corneal power
4) Potvin-Hill (Pentacam)
-Holladay 1 IOL formula calculated using thinnest corneal pachymetry from the Pentacam and Power for the Sagittal Curve (PWR_SF_Pupil_4.0 mm Zone: 4mm zone centered on pupil measuring Sagittal Curve mean K)
5) DK-Holladay-IOLM (IOL Master or Lenstar)
-Modified double-K formula using post-RK K (from IOL master or Lenstar) to calculate corneal refractive power
6) OCT
7) Barrett True K
Management
Surgery
Recent developments in imaging and devices have allowed for use of intra-operative technologies such as aberrometry and refractometry to adjunct assessment of IOL selection.[6] Otherwise once a surgical plan including type of anesthesia is in place anticipate any other intra-operative such as a 10-0 nylon should be on standby if wounds dehisce (see below). Lower infusion pressure or lower bottle height may aid in avoiding potential complications.
Complications
Intra-operative wound dehiscence can occur in very weak wounds under infusion pressure and lead to loss of stability and high fluid utilization. Suturing these may add some partial stability both for the cornea and chamber mechanics. Also control of infusion pressure and minimizing number of times in/out of the eye will be beneficial to minimize compression/decompression events.
Crossing of incisions - Scleral tunnel incisions are typically preferred for wound construction when there are many (>8) incisions or incisions will not allow adequate space for a clear corneal incision. Clear corneal incisions can be made between between RK incisions[7], however clear corneal incisions made too close to RK incisions or too central are at a higher risk for further inducing irregular astigmatism, possible worsening of aberrations and loss of structural integrity if they cross the RK incisions. Structural instability of incisions may require suturing or even corneal transplantation depending on resultant opacity and irregular astigmatism.
Depending on corneal edema and other factors, the post-operative eye may demonstrate an early hyperopic surprise that may improve over the course of 2-3 months. Given this, it is advisable to monitor refractive error in the early post-operative period and avoid potential IOL exchange in the first few months after surgery and much of the refractive surprise can resolve on its own.[8]
Post-operative
Standard risks of any intra-ocular surgery apply to this surgical scenario, however additional risks of refractive surprise and fluctuating vision due to altered corneal physiology and anatomy still apply. General risks related to this must be discussed in the pre-operative counseling (see above).
References
- ↑ Khairallah, M, Vision Loss Expert Group of the Global Burden of Disease Study. Invest. Ophthalmol. Vis. Sci. 2015. Oct;56(11):6762-9. doi. 10.1167/iovs.15-17201.
- ↑ Sato, T (1939). "Treatment of conical cornea (incision of Descemet's membrane)". Acta Soc Ophthalmol Jpn (in Japanese). 43: 544–55.
- ↑ Jump up to: 3.0 3.1 Waring GO, Lynn MJ, McDonnell PJ (October 1994). "Results of the prospective evaluation of radial keratotomy (PERK) study 10 years after surgery". Arch. Ophthalmol. 112 (10): 1298–308. doi:10.1001/archopht.1994.01090220048022. PMID 7945032.
- ↑ Elbaz, Uri et. al. "Collagen crosslinking after radial keratotomy" Cornea. 2014 Feb;33(2):131-6. doi. 10.1097/ICO.0000000000000044.
- ↑ Turnbull, Andrew M.J. et al. Methods for Intraocular Lens Power Calculation in Cataract Surgery after Radial Keratotomy. Ophthalmology, Volume 127, Issue 1, 45 - 51
- ↑ Curado, Sebastiao et. al. "Intraoperative Aberrometry Versus Preoperative Biometry for IOL Power Selection After Radial Keratotomy: A Prospective Study" J. Refractive Surgery. 2019. Oct 1;35(10):656-661.
- ↑ Meduri, A et. al. "Cataract surgery on post radial keratotomy patients" Int. J. Ophthalmol. 2017 Jul 18;10(7):1168-1170. doi: 10.18240/ijo.2017.07.12. eCollection 2107.
- ↑ Stephenson M. Refractive Surprises After Cataract Surgery. In: Review of Ophthalmology; 2014.
- Geggel HS. Intraocular Lens Power Selection after Radial Keratotomy: Topography, Manual and IOLMaster Keratometry Results Using Haigis Formulas. Ophthalmology. 2015 May; 122(5): 897-902.doi. 10.1016/j.ophtha.2014.12.002.Epub 2015 Jan 2017. PMID: 25601534