Cataract Surgery Following Cornea Transplant
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Cataract surgery after corneal transplantation necessitates specific attention to stability and optimization of the corneal graft to enable precise IOL selection, and preservation of the corneal graft as cataract surgery causes corneal endothelial damage. The type of corneal graft will dictate planning; treatment of cataracts after full thickness penetrating keratoplasty (PKP) and treatment after Descemet's membrane endothelial keratoplasty (DMEK) differ on many levels.
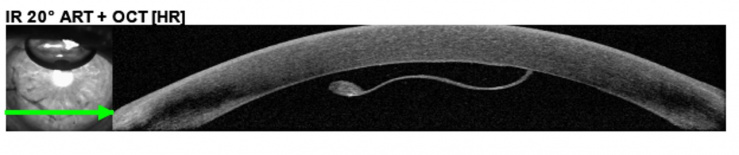
Fig 1. DMEK graft with detached peripheral edge
Patient counseling is of paramount importance. Patients should understand the known risks to their current graft as well as refractive goals, predictability and likely outcomes.
Offering cataract surgical treatment should take into account numerous factors including but not limited to: vision, fellow eye status, patient needs, graft status, type and duration of graft, lens density and medical necessity.
Methods
Optimizing the ocular surface
Optimizing the ocular surface is important before cataract surgery. This is even more pronounced in the context of prior corneal surgery. Categorical rejuvenation in the form of increased lubrication or other dry eye treatments are likely warranted to blunt the expected increase in ocular surface inflammation and secondary surface disease which happens even in the majority of cataract surgeries.
Preop-Biometry and Topography/ Tomography
The corneal graft must be clear to allow for optical biometry with good signal strength. If the corneal graft is not clear, A-scan biometry could bypass the non-clear cornea. Though cataract surgery in the setting of a "non-clear" cornea is often a combined procedure (cornea graft, lens extraction, intraocular lens implantation), which has its own challenges and is a topic of separate discussion.
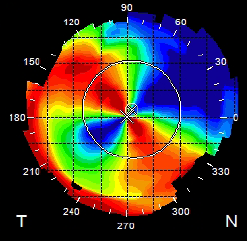
Compared to combined procedures, performing cataract surgery after corneal transplants has the advantage of better refractive outcomes (Hayashi and Hayashi, 2006). Care should be taken to confirm stability of the keratometry. In these patients, all corneal sutures should be removed, if possible, before final keratometry readings are obtained. Topography/ Tomography will be especially helpful in cases of PKP/Therapeutic Keratoplasty (TKP)/Lamellar Keratoplasty (LK)/Deep Anterior Lamellar Keratoplasty (DALK) as these grafts are known to have higher rates of significant astigmatism (regular and irregular), confounding IOL planning. IOL calculations are more reliable for EK compared to PKP/DALK.
IOL choices
Significant level of consistency and confidence in analyses (and counseling) are needed if considering IOL models other than standard monofocal styles (e.g. toric, see astigmatism management below). Caution must be taken when using any IOL model that induces aberrations significantly, or lowers contrast sensitivity, as corneal grafts present a range of compromised optics whether it is in the form of opacity (such as interface haze for lamellar based procedures or scarring at the graft host junction) or significant aberrations from astigmatism. It is often challenging to characterize higher order aberrations for PKP/DALK. Therefore, focus should be on maximizing treatment of lower order aberrations including 2nd order Zernike optics (myopia/hyperopia/astigmatism).
IOL choices for irregular and aberrated corneas may include pinhole IOL optics and adjustable optics, such as the Light-Adjustable Lens (LAL), to allow for correction or reduction in refractive errors after cataract surgery.
Anesthesia Considerations
Anesthesia considerations should follow what would be best suited for the patient ranging from topical anesthesia to general anesthesia based on patient ability to cooperate with the surgery. If anticipating maneuvers that include scleral tunnel, manual ECCE, SICS, then a retrobulbar or peribulbar block +/- without facial nerve block can be utilized. Positioning for these larger incision treatments should aim to minimize posterior pressure.
Incision Locations and types
Standard clear corneal incisions are a viable option as long as care is taken not to extend near the edges of the graft as to avoid causing detachments of endothelial grafts or dehiscence of full thickness grafts. Shorter uniplanar wounds that are sutured at the end may offer a compromise approach to achieve this.
Scleral tunnel utilization in preparation for standard Phaco/IOL, ECCE, SICS offers advantages of decreasing the above risks by moving the incision away from the cornea.
Soft-shell techniques and viscoelastic choices
Use of a dispersive viscoelastic that coats the endothelium is likely to be universally employed in intraocular surgery, particularly cataract extraction by phacoemulsification (and to some degree manual ECCE) to reduce endothelial loss.
Phacoemulsification, FLACS, Manual ECCE, Manual SICS
The choice of method for cataract extraction should factor in the graft's endothelial cell count as well as surgeon comfort and confidence with the technique. When using phacoemulsification, greater distance from the corneal endothelium should be maintained to avoid close energy and aggressive fluid flow near the graft. Methods of nuclear disassembly such as phaco-flip or pop and chop should be chosen with caution.
Astigmatism management
Particularly for PKP/DALK grafts, attention must be paid to the presence of astigmatism, both irregular and regular as this can significantly affect operative planning and refractive goals. For clinically significant levels of regular astigmatism management can include a variety of adjunct techniques in isolation or in combination, such as the use of corneal relaxing incisions (in the graft-host junction, internal to the wound interface) and toric IOLs. Limbal relaxing incisions in the context of PKP/DALK likely have limited role as the biomechanical effects likely have little translation to the central optical zones. Laser refractive treatments postoperatively may be used but with caution on the effects of ocular surface health. If utilized, the newer platforms using topography guided ablation algorithms may offer some tactical advantage of optical rehabilitation for cases with a component of irregularity.
Preoperative regional pachymetry, OCT or confocal microscopy may be adjunct imaging modalities to aid in decision making on wound depth and the amount of existing fibrosis (versus epithelial plug) at graft-host junctions. Incisions can be made with various instruments ranging from dedicated keratotomy knives to femtosecond laser.
Preoperative treatment with additional immune modulating therapies
There maybe extra considerations for adjunct increase in topical steroids or other ways to decrease immune mediated response against the graft peri-operatively for cataract surgery. Decision to add additional immune modulating agents can be made on a case by case basis.
References
- Stachs, Oliver et. al. Structural-functional correlations of corneal innervation after LASIK and penetrating keratoplasty. J Refract Surg. 2010 Mar;26(3):159-67. doi: 10.3928/1081597X-20100224-01. Epub 2010 Mar 11.
- Fogagnolo, Paolo et. al. New therapeutic strategy and innovative lubricating ophthalmic solution in minimizing dry eye disease associated with cataract surgery: a randomized, prospective study. Adv Ther. 2020 Apr;37:1664-1674. doi: 10.1007/s12325-020-01288-z. Epub 2020 Mar 17.
- Lynds R, Hansen B, Blomquist PH, Mootha VV. Supervised resident manual small-incision cataract surgery outcomes at large urban United States residency training program. J Cataract Refract Surg. 2018 Jan;44(1):34-38. doi: 10.1016/j.jcrs.2017.09.032. PMID: 29502616
- Lains, I et. al. Irregular Astigmatism After Corneal Transplantation--Efficacy and Safety of Topography-Guided Treatment. Cornea. 2016 Jan;35(1):30-6. doi: 10.1097
- Bohringer, Daniel et. al. Long-term follow-up of astigmatic keratotomy for corneal astigmatism after penetrating keratoplasty. Acta Ophthalmol.. 2016 Nov;94(7):e607-611. doi: 10.1111/aos.13061.
- Hong-Wei Zho, Li-Xin Xie. Effects of Cataract Surgery on Endothelium in Transplanted Corneal Grafts: Comparison of Extracapsular Cataract Extraction and Phacoemulsification for Complicated Cataract after Penetrating Keratoplasty. Chin. Med J. (Engl) 2016 Sep 5;129(17):2096-101. doi: 10.4103/0366-6999.189050
- Muraine, M, et. al Keratoplasty combined with cataract surgery. J Fr. Ophthalmol. 2012 Sep;35(7):546-54. doi: 10.1016/j.jfo.2012.06.002. Epub 2012 Aug 21
- Parmar P, Salman A, Kalavathy CM, Thomas PA, Jesudasan CA. Outcome analysis of cataract surgery following therapeutic keartoplasty. Cornea. 2005 Mar;24(2):123-9. doi: 10.1097/01.ico.0000138835.06953.db.