Capsular Support Devices
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
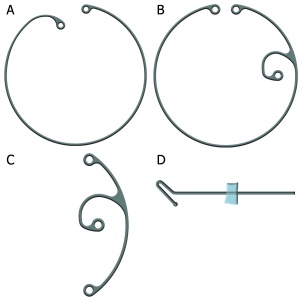
The presence of zonular weakness increases the risk of intra- and postoperative complications from cataract surgery, including posterior capsular rupture, vitreous loss, and lens dislocation and decentration. Capsular support devices are important management tools for eyes with zonulopathy[1]. They facilitate safe and successful cataract surgery by improving capsular bag stability and centration. These devices consist of capsular tension rings, modified capsular tension rings, capsular tension segments, and capsular retention hooks (Figure 1).
Evaluation
Capsular support devices should be considered for patients who have suspected zonular weakness or who are considered at risk for developing zonulopathy. Common risk factors for weak zonules are pseudoexfoliation syndrome, mature cataracts, high myopia, and prior eye surgery (e.g. radial keratotomy, vitrectomy, or glaucoma filtering surgery)[1]. Other risk factors include history of eye or head trauma, uveitis, retinopathy of prematurity, retinitis pigmentosa, Marfan syndrome, homocystinuria, Weill-Marchesani syndrome, Rieger syndrome, myotonic dystrophy, hyperlysinemia, sulfite oxidase deficiency, and intraocular neoplasms.
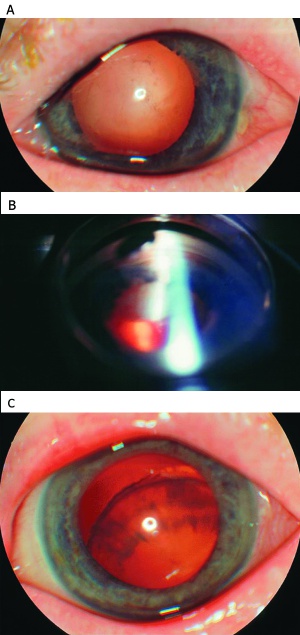
Signs of weak zonules include iridodonesis, phacodonesis, abnormal anterior chamber depth or asymmetry, angle asymmetry on gonioscopy, and vitreous in the anterior chamber[2]. Zonular dehiscence and lens subluxation or dislocation can be seen in advanced zonulopathy (Figure 2).
Despite a surgeon’s best efforts, weak zonules may not be noticed until after the surgery has begun. Intraoperative signs of weak zonules include anterior chamber depth fluctuation, difficulty puncturing the anterior lens capsule, star-shaped striae on the capsule surface during the capsulotomy, lens movement when performing the capsulorrhexis, and difficulty rotating the nucleus within the capsular bag despite adequate hydrodissection[2].
Types of Capsular Support Devices
Capsular tension devices improve the safety and success of cataract surgery when the integrity of the zonular apparatus is in question[1][4]. By increasing the likelihood of capsular bag placement of an intraocular lens, the risks associated with alternative fixation in the anterior chamber or to the iris and sclera can be lessened.
Standard Capsular Tension Rings
The standard capsular tension ring or CTR is a flexible C-shaped device made of polymethylmethacrylate (PMMA)(Figure 1A)[5][6]. Each end has a blunt tipped eyelet to aid in insertion of the device. When positioned in the capsular bag, the ring exerts an outward force that redistributes tension from areas of intact zonules to strengthen areas of weak or missing zonules[5][7].
Indications and Contraindications
The best candidate for a standalone standard capsular tension ring is a patient with mild diffuse zonular weakness or focal zonular weakness extending fewer than three to four clock hours.
A standard capsular tension ring alone may not be adequate for eyes with advanced zonular weakness, more than 4 clock hours of zonular loss, or progressive zonulopathy. Such eyes require endocapsular devices that can be scleral fixated, such as modified capsular tension rings or capsular tension segments.
Absolute contraindications for a capsular tension ring are the presence of anterior or posterior capsular tears or any concern for bag compromise. A capsular tear may propagate due to the centrifugal forces exerted by the ring on the capsular bag.
Device Specifications
Two capsular tension rings have been approved by the U.S. Food and Drug Administration. The Morcher ring (Stuttgardt, Germany), distributed by FCI Ophthalmics (Pembroke, Massachusetts, USA) and Alcon Laboratories, Inc (Fort Worth, Texas, USA), is available in three sizes: type 14 (12.3 mm diameter, compresses to 10.0 mm), type 14C (13.0 mm diameter, compresses to 11.0 mm), and type 14A (14.5 mm diameter, compresses to 12.0 mm). The Ophtec ring (Groningen, The Netherlands), distributed by Johnson & Johnson Vision (Santa Ana, California, USA), is available in two sizes: model 275 (12.0 mm diameter, compresses to 10 mm) and model 276 (13.0 mm diameter, compresses to 11.0 mm). The Morcher ring is slightly stiffer than the Ophtec ring.
Sizing
A correctly sized ring has ends that slightly overlap each other and a diameter that is slightly larger than the diameter of the capsular bag [4][8]. Horizontal white-to-white and globe axial length measurements are correlated with bag diameter and are used to estimate appropriate ring size. However, it is not unreasonable to implant the largest ring available, since a larger ring has no apparent disadvantage[1].
Capsulorrhexis construction
A capsulorrhexis approximately 5.0 to 5.5 mm in diameter is preferred. A capsulorrhexis that is too small makes phacoemulsification more challenging and increases the risk of postoperative capsular phimosis. A capsulorrhexis that is too large may preclude the use of endocapsular support devices.
Ring insertion
The standard capsular tension ring can be inserted any time after the capsulorrhexis is constructed. Nonetheless, it is better to insert the ring as early as required but as late as possible. Early ring insertion enables early stabilization of the capsular bag, but complicates removal of lens material if cortex is trapped between the ring and the capsular wall[11].
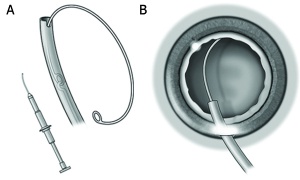
The ring can be implanted using an injector or dialed manually into the bag (Figure 3). Most surgeons use a single-use preloaded injector that is available for the Morcher and Optec rings. Reusable injectors are available from Geuder (Heidelberg, Germany) and Optec, but the Optec ring is not compatible with the Geuder injector. Manual ring insertion is performed using forceps and a Sinskey hook. With either technique, the leading arm of the ring should be carefully directed toward the area of weak zonules.
A newly described “fish tail” technique does not require dialing or injection and may limit zonular stress[12].
Modified Capsular Tension Rings
The standard capsular tension ring is frequently unable to center or stabilize the capsular bag in cases of more profound zonular weakness. Modified capsular tension rings, or Cionni rings, were developed to address this issue (Figure 1B)[13]. Because they can be permanently sutured to the sclera, they are indicated for advanced zonular weakness, more than four clock hours of weak zonules, and progressive zonulopathy.
Like a standard ring, the modified ring is a C-shaped PMMA device that needs to be dialed into the bag. Unlike the standard ring, it has one or two additional eyelets located 0.25 mm anterior to the plane of the ring and it cannot be injected. It must be dialed in manually. Via the extra eyelet(s), the surgeon can scleral fixate the modified ring with 9-0 polypropylene or CV-8 GoreTex suture.
Capsular Tension Segments
A capsular tension segment or CTS is a partial PMMA segment that provides 90 degrees of capsular support. It has a central eyelet that extends anterior to the plane of the ring for suture fixation to the sclera (Figure 1C)[14].
It is indicated when there is advanced zonular weakness and has several distinct advantages over a Cionni modified ring. The segment does not require dialing, can be used in the presence of an anterior or posterior capsular tear, and can be used for both intraoperative stabilization and postoperative fixation. It is less likely than a capsular tension ring to trap cortical material against the capsular wall.
One or more capsular tension segments can be used in the same eye. A capsular tension segment can be paired with a standard capsular tension ring to provide circumferential support.
Capsular Retention Hooks
Capsular retention hooks provide intraoperative capsular bag stabilization for patients with advanced zonular weakness (Figure 1D)[1]. The Mackool Capsular Support System (FCI Ophthalmics) consists of modified nylon iris hooks that support the anterior capsule edge and are temporarily secured by a retainer tab during surgery. By improving bag stabilization, capsule retractors may allow for cortex to be removed before a capsular tension ring needs to be inserted. Capsular retractors from MicroSurgical Technologies (Redmond, Washington) have a loop of double banded nylon that is friendlier to the capsular equator than the Mackool hook. The Chang modification makes it impossible for a capsule tension ring to become trapped in the loop portion of the device, which occasionally happened with the first-generation capsule retractor.
Outcomes
Studies show that capsular tension rings decrease the intraoperative risks of zonular dehiscence[15], posterior capsular rupture, and vitreous loss[16] and the postoperative risks of lens decentration, lens tilt[17], and posterior capsular opacification[18]. Capsular tension rings have no effect on refractive outcome, and modifying IOL power calculations is not necessary[19][20].
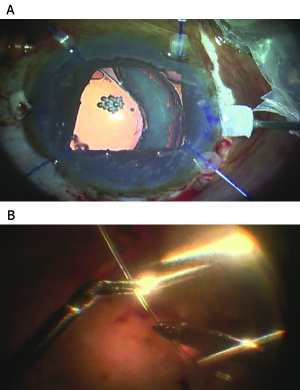
While capsular tension rings are generally inserted without issue, studies have described inadvertent insertion of a ring into the anterior chamber angle[21] and into the vitreous through a capsular tear[22]. Rings can also be dialed into the ciliary sulcus if the surgeon is not attentive to assuring that the leading point on the ring is injected beneath the capsulorrhexis. Late subluxation and posterior dislocation of the entire lens-ring-capsular bag complex have been reported[23], and this is of most concern in patients with progressive zonulopathy, like pseudoexfoliation syndrome or Marfan syndrome (Figure 4). To prevent late subluxation, a sutured modified capsular tension ring or capsular tension segment can be used. However, the risks of increased intraocular manipulation and suture breakage, erosion, and infection need to be considered[16].
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 Reidel PJ, Samuelson TW. Capsular tension rings. Colvard DM, editor. Los Angeles, CA 2009. 115-21 p.
- ↑ Jump up to: 2.0 2.1 Sangal N, Chen TC. Cataract surgery in pseudoexfoliation syndrome. Semin Ophthalmol. 2014;29(5-6):403-8.
- ↑ American Academy of Ophthalmology. Exfoliation syndrome. https://www.aao.org/education/image/exfoliation-syndrome-3 Accessed December 12, 2024.
- ↑ Jump up to: 4.0 4.1 Goldman JM, Karp CL. Adjunct devices for managing challenging cases in cataract surgery: pupil expansion and stabilization of the capsular bag. Curr Opin Ophthalmol. 2007;18(1):44-51.
- ↑ Jump up to: 5.0 5.1 Gimbel HV, Sun R, Heston JP. Management of zonular dialysis in phacoemulsification and IOL implantation using the capsular tension ring. Ophthalmic Surg Lasers. 1997;28(4):273-81.
- ↑ Hara T, Hara T, Yamada Y. "Equator ring" for maintenance of the completely circular contour of the capsular bag equator after cataract removal. Ophthalmic Surg. 1991;22(6):358-9.
- ↑ Bayraktar S, Altan T, Kucuksumer Y, Yilmaz OF. Capsular tension ring implantation after capsulorhexis in phacoemulsification of cataracts associated with pseudoexfoliation syndrome. Intraoperative complications and early postoperative findings. J Cataract Refract Surg. 2001;27(10):1620-8.
- ↑ Vass C, Menapace R, Schmetterer K, Findl O, Rainer G, Steineck I. Prediction of pseudophakic capsular bag diameter based on biometric variables. J Cataract Refract Surg. 1999;25(10):1376-81.
- ↑ American Academy of Ophthalmology. Capsular tension ring. https://www.aao.org/education/image/capsular-tension-ring-5 Accessed December 12, 2024.
- ↑ American Academy of Ophthalmology. Capsular tension ring. https://www.aao.org/education/image/capsular-tension-ring-6 Accessed December 12, 2024.
- ↑ Ahmed, II, Cionni RJ, Kranemann C, Crandall AS. Optimal timing of capsular tension ring implantation: Miyake-Apple video analysis. J Cataract Refract Surg. 2005;31(9):1809-13.
- ↑ Angunawela RI, Little B. Fish-tail technique for capsular tension ring insertion. J Cataract Refract Surg. 2007;33(5):767-9.
- ↑ Cionni RJ, Osher RH. Management of profound zonular dialysis or weakness with a new endocapsular ring designed for scleral fixation. J Cataract Refract Surg. 1998;24(10):1299-306.
- ↑ Hasanee K, Ahmed, II. Capsular tension rings: update on endocapsular support devices. Ophthalmol Clin North Am. 2006;19(4):507-19.
- ↑ Bayraktar S, Alton T, Kucuksumer Y, Yilmaz OF. Capsular tension ring implantation after capsulorhexis in phacoemusification of cataracts associated with pseudoexfoliation syndrome. Intraoperative complications and early postoperative findings. J Cataract Refract Surg 2001; 27:1620–1628.
- ↑ Jump up to: 16.0 16.1 Cionni RJ, Osher RH, Marques DM, et al. Modified capsular tension ring for patients with congenital loss of zonular support. J Cataract Refract Surg 2003; 29:1668–1673.
- ↑ Lee DH, Shin SC, Joo CK. Effect of a capsular tension ring on intraocular lens decentration and tilting after cataract surgery. J Cataract Refract Surg 2002; 28:843–846.
- ↑ De´liseo D, Longanesi L, Grisanti F, Negrini V. Prevention of posterior capsule opacification using capsular tension ring for zonular defects in cataract surgery. Eur J Ophthalmol 2003; 13(2):151–154.
- ↑ Boomer JA, Jackson DW. Anatomic evaluation of the Morcher capsular tension ring by ultrasound biomicroscopy. J Cataract Refract Surg 2006; 32:846–848.
- ↑ Schild AM, Rosentreter A, Hellmich M, et al. Effect of a capsular tension ring on refractive outcomes in eyes with high myopia. J Cataract Refract Surg 2010; 36:2087–2093.
- ↑ Little BC, Richardson T, Morris S. Removal of the capsular tension ring from the anterior chamber angle. J Cataract Refract Surg. 2004;30(9):1832.
- ↑ Levy J, Klemperer I, Lifshitz T. Posteriorly dislocated capsular tension ring. Ophthal Surg Lasers Imaging. 2005;36(5):416.
- ↑ Jehan FS, Mamalis N, Crandall AS. Spontaneous late dislocation of the intraocular lens within the capsular bag in pseudoexfoliation patients. Ophthalmology. 2001;108(10):1727.