Canthoplasty
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Medial and Lateral Canthoplasty
Background
The medial and lateral canthi and their underlying structures play invaluable functional and structural roles. They contribute to the shape of the eye, aid with proper blink and corneal protection, and contribute to the aesthetic properties of the face. Due to their differences, canthoplasty for both the medial canthus and lateral canthus have individual indications, approaches, and special considerations.
The medial canthus and medial canthal ligaments are landmark components that provide structural shape and integrity to the lower eyelid. The medial canthus serves to give a medial angular contour to the eye, aids in the lacrimal pump mechanism, and prevents ectropion. Due to its proximity to the nasolacrimal duct and attachments, surgeries to the area must focus on restoring or maintaining functional capacity. Disruption to the medial canthus can lead to functional disease like epiphora and can cause structural abnormalities such as lower lid laxity, abnormal canthal position, increased intercanthal distance, and a reduced or absent naso-orbital valley [1].
The lateral canthus is an equally delicate structure and similarly contributes to the overall shape and health of the eye. Just like the medial canthus, there are important underlying anatomical structures which must also be considered during cosmetic surgery and repair. Disruption to the lateral canthus can lead to lower lid laxity, ectropion, chronic irritation, epiphora, and exposure keratopathy. Furthermore, the lateral canthus in particular is an attention point where observers look for bilateral symmetry. The lateral canthal angle and position is also a subconscious indicator of youthfulness.
Lower lid laxity and associated clinical manifestations may lead to inadequate blinking and protection of the ocular surface. These conditions are typically caused by previous surgery, aging, hormonal conditions, congenital defects, trauma, or paralysis[2]. In addition to negative functional sequelae, eyelid laxity causes an unpleasant aesthetic look that deviates from a desired youthful anatomic structure. Canthoplasty is a surgical reconstructive procedure to modify and reshape the corner of the eye.
Reconstruction of the canthal margins is used to reestablish eyelid function, amend eyelid malposition, or satisfy aesthetic preferences[3]. Canthoplasty can also be used to alter the dimensions of the eye to achieve a more desirable and attractive appearance. Therefore, its applicability is twofold - there are both functional and cosmetic benefits for a wide range of patients.
This article aims to comprehensively address medial and lateral canthoplasty with the intention of differentiating the unique considerations of each. This article also intends to provide sequential guidance from patient evaluation to postoperative care, as well as the different surgical approaches to canthoplasty.
Anatomy
Due to the intricacy and unique anatomy of both the medial and lateral canthus, detailed knowledge of the periorbital anatomy is necessary for ophthalmologists to successfully reconstruct the canthus, optimize outcomes, and avoid complications.
Muscles
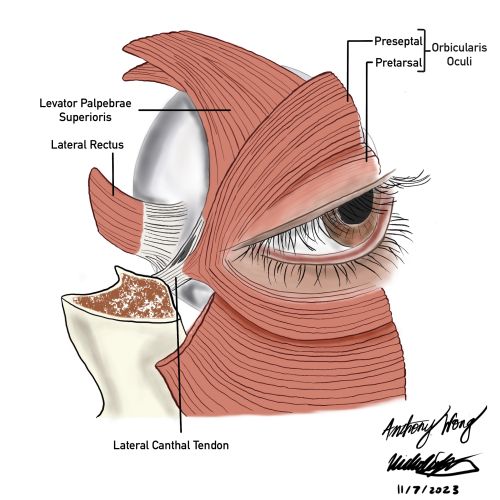
The orbicularis oculi muscle is innervated by the seventh cranial nerve and is separated into pretarsal, preseptal, and orbital sections. It is shaped like a sphincter around the eye and functions to close the eyelid. The orbital section of the muscle originates from the maxillary process of the frontal bone, the frontal process of the maxillary bone, the superomedial orbital margin, medial canthal tendon, and the inferomedial orbital margin. The preseptal segment starts at the medial canthal tendon and posterior lacrimal diaphragm, where it splits to surround the eye and converges at the lateral palpebral raphe. Laterally, the pretarsal orbicularis oculi muscles join the lateral canthal tendon about 7 mm from the lateral orbital tubercle. The inferior part of the orbicularis oculi may extend to the corner of the mouth and is a major structure in the malar, cheek, and nasojugal areas of the face.
Eyelids
The upper eyelid consists of multiple layers, and is often separated into 3 lamellae (anterior, middle, posterior). Depending on the height from the eyelid margin, there are varying numbers of layers. In general from anterior to posterior the layers are as follows: skin, orbicularis oculi, pre-septal fat, orbital septum, post-septal fat, levator muscle, mullers muscle, tarsus, conjunctiva.
The skin on the eyelids lacks subcutaneous fat and is the thinnest skin in the human body. The orbital septum is a connective tissue layer that acts as a divider between the anterior eyelid and the more posterior orbital structures. Superiorly, it links the superior orbital rim periosteum to the levator aponeurosis and prevents inferior drift of the orbital fat[4].
The lower eyelid spans the distance between the lid margin and the inferior orbital bony rim. Like the upper eyelid, it can be divided into three layers or the anterior, middle, and posterior lamella. Once again, depending on the height from the eyelid margin, there will be varying structures anteriorly to posteriorly. In general the anterior lamella consists of skin and the orbicularis oculi muscle. The middle lamella contains the orbital septum, tarsus, and retroseptal fat. Finally, the posterior lamella involves the lower eyelid retractors, conjunctiva, and capsulopalpebral fascia, which is an extension of the inferior rectus muscle. The periorbita, periosteum, and orbital septum fuse to form the arcus marginalis that lines the infraorbital rim.
Lacrimal Gland
The lacrimal gland is an orbital structure located superotemporally within the lacrimal fossa, and it plays a crucial role in producing the aqueous component of the tear film critical for corneal protection. It is divided into two lobes, the orbital and palpebral, by the levator palpebrae superioris. Furthermore, these two lobes are connected by interlobular ducts. When a histological section is taken of the lacrimal gland, the tissue reveals mixed serous and mucinous acini, myoepithelial cells, and interconnecting ductules. Serous and mucinous acini secret the aqueous component of the tear film, and this aqueous is physically excreted via the myoepithelial cells. Another crucial role of the lacrimal gland is to secrete IgA and IgG antibodies from the myoepithelial cells, which ultimately establishes an adaptive immune purpose[5].
The lacrimal gland receives its blood supply from the lacrimal artery, which originates from the ophthalmic artery. The lacrimal vein then drains the blood into the superior ophthalmic vein, which travels across the cavernous sinus. The lacrimatory nucleus of the facial nerve within the pons controls the parasympathetics that regulate lacrimal gland's aqueous secretion. On the other hand, the superior cervical ganglion controls the sympathetic innervation of the lacrimal gland. Finally, the lacrimal nerve, originating from the ophthalmic nerve, controls sensory innervation to the lacrimal gland.
Iatrogenic injury is a potential complication of periocular surgery such as canthoplasty. Division of the temporal conjunctival fornix during a lateral canthoplasty has shown potential structural trauma to the lacrimal gland, leading to gland dysfunction[6]. Moreover, disruption of ophthalmic nerve fibers may cause harm to lacrimal gland function. If the ocular surface loses sensation secondary to ophthalmic nerve fiber damage, the lacrimal gland will lack the necessary sensory input and its activity can no longer be mediated for proper tear secretion.
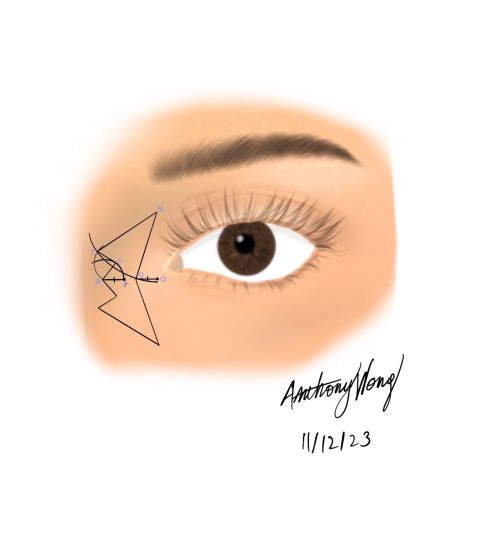
Medial Canthus
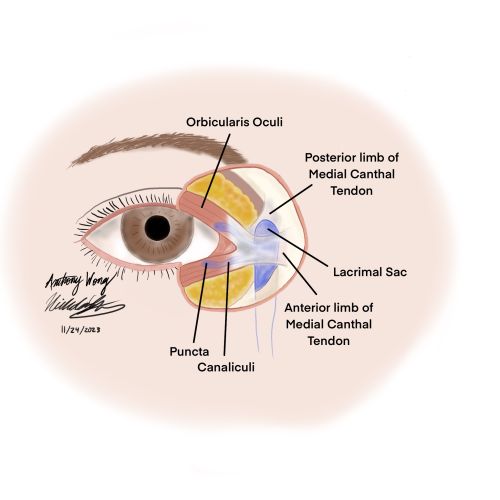
The medial canthus is the medial confluence of the upper and lower eyelid margins. The medial canthal tendon represents the union between the septum orbitale, Lockwood’s ligament, the levator aponeurosis, the check ligament of the medial rectus, and the pretarsal and preseptal portions of the orbicularis oculi muscle.
Medially, the pretarsal orbicularis oculi can be subdivided into a superficial and deep head. The superficial head becomes the anterior aspect of the medial canthal tendon, merging with the fibrous end of the tarsal plate. The deep head, also called the pars lacrimalis or Horner’s muscle, originates on the lacrimal bone and converges at the medial palpebral commissure before inserting into the posterior lacrimal crest directly behind the lacrimal sac. Horner’s muscle is thought to participate in closing the medial canthus and lacrimal punctum. It also functions to pull the tarsus medial and tighten the palpebral margins. Finally, it compresses the lacrimal canaliculus with decreasing pressure medially to the lacrimal sac. Together these actions facilitate the flow of tears medially across the eyeball and through the lacrimal canaliculus towards the lacrimal sac. This is important for preserving the layer of lacrimal fluid over the cornea.
Similarly to the pretarsal portion of the orbicularis, the preseptal portion is separated into superficial and deep heads that both eventually join the medial canthal tendon. The deep head attaches to the fascia surrounding the lacrimal sac as well as the medial orbital wall above and below Horner’s muscle. The proximity of this insertion to the lacrimal sac has important implications during blinking. When the eyelids close, traction is placed on the deep head, which pulls the lacrimal sac fascia laterally and creates a negative internal pressure that draws tears to drain through the puncta and canaliculi.
The medial canthal tendon inserts onto the frontal process of the maxilla in three different fashions: anterior horizontal, posterior horizontal, and vertical. The anterior horizontal limb inserts onto the anterior lacrimal crest in alignment with the superior edge of the lacrimal sac. The posterior horizontal part diverges near the anterior lacrimal crest and attaches to the posterior lacrimal crest. The vertical component bears most of the disruptive forces to the medial canthus. These vertical fibers integrate into the periosteum at the medial orbital rim near the nasofrontal suture and define the superior border of the medial canthal tendon[7].
Overall, the medial canthus is a complex and crucial structure of the orbital anatomy. Its close relation to the lacrimal drainage system makes it particularly difficult to navigate and repair. Extra care and caution must be taken during surgeries involving the surrounding structures to avoid compromising the tear drainage apparatus and causing detrimental complications.
Lateral Canthus
The lateral canthus is the temporal point of fusion of the upper and lower eyelid. Structurally, the lateral canthal tendon fixates the position of the eyelids by its attachment to the periosteum of the inner lateral orbital tubercle. This area also receives support from the lateral horn of the levator aponeurosis, Lockwood’s ligament, the check ligament of the lateral rectus muscle, and the lateral canthal ligament.
The upper and lower tarsal plates converge at the lateral canthal tendon that attaches to Whitnall’s tubercle on the lateral orbital rim [8]. The pretarsal and preseptal orbicularis oculi muscles form the anterior aspect of the lateral canthal tendon. Posteriorly, the tendon is completed by the check ligaments of the lateral canthal muscle. The lateral horn of the levator aponeurosis is continuous with the superior component of the lateral canthal tendon. The inferior part of the tendon is created by fibrous elements of Lockwood’s suspensory ligament.
The fixation point of the lateral canthal tendon to the orbital tubercle periosteum is particularly important to note because improper surgical manipulation can cause lower lid laxity and ectropion. Movement of the lateral canthal tendon at its posterior fibrous attachments to the check ligament of the lateral rectus muscle provides an opportunity to alter the lateral canthal angle.
The Aesthetic Eye
The “almond” eye shape is a highly desired appearance that is primarily determined by the shape and position of the palpebral fissures. Ideally, there is an upward slope between medial and lateral canthi of up to 3 mm[9]. This tilt has been recognized as a necessary feature to achieve a youthful image. Horizontal dimensions of the eye aperture that reveal 1 to 2 mm of sclera below the iris may also be an appealing trait, although this space typically does not exist. Finally, a slight downward curving of the lateral third of the lower eyelid contributes to the illusion of a wider eye. The lateral canthus may drift inferiorly with aging or may be displaced by trauma, malignancies, or congenital defects such as dysostosis and microsomia. The clinical presentation of medial canthal displacement would likely include punctal eversion or a widened gap between the lower punctum and caruncle[10].
Indications
Functional Canthoplasty
Canthoplasty is a reconstructive procedure that is indicated for a variety of eyelid conditions. It is applicable to any disruption to the normal architecture of the canthus which can lead to negative functional sequelae. There are other oculoplastic procedures that can influence the shape of the canthus such as tarsorrhaphies, blepharoplasties, lateral tarsal strips, transpositions, and eyelid slings that may be used in tandem with canthoplasty or individually. Because of this, the surgeon is able to formulate the best plan of action for each indication.
Below is a list of common indications [11][12]:
- Entropion
- Congenital and involutional
- Ectropion
- Congenital, involutional and cicatricial
- Lid laxity
- Seen with anophthalmos or enophthalmos
- Seen with facial nerve palsy
- Canthal dystopia
- Exposure keratopathy
- Epiphora
- Vertical eyelid retraction
- Seen after blepharoplasty
- Seen with Thyroid Eye Disease (contraindicated if significant proptosis)
- In the setting of trauma
- Repair after Iatrogenic damage or Trauma
- In Conjunction with Blepharoplasty
- To prevent ectropion or eyelid retraction
- Festoons
- Delayed repair resulting in rounding of the canthus
- Telecanthus
- Congenital malposition or occlusion of the visual field
- Absent naso-orbital valley
- With lateral orbitotomy
- In orbital decompression
- Removal of orbital tumors
Cosmetic Canthoplasty
Although canthoplasty was historically born out of a need to repair the canthus, it has now gained popularity as an elective cosmetic procedure. Cosmetic canthoplasty typically aims to alter the lateral canthal angle. Due to the nature of cosmetic procedures, there are different goals depending on the patient and their baseline anatomy. Special considerations for different populations are addressed below.
Cultural Considerations in Appearance
It is important to make a distinction between ethnic populations and recognize that canthoplasty goals are different between individuals. Very specific goals should always be discussed and the surgeon should be cognizant of the cultural context and societal framework that influence outcome satisfaction. Additionally, the surgeon should aim to protect the patient’s cultural identity or individuality.
Canthoplasty has become widely popular among Asian populations as a surgical option to give the eye a larger appearance. Cosmetic canthoplasty lengthens the palpebral fissure and changes the angle of the lateral canthus to tilt downward. This increases the amount of lateral scleral show, often called the “scleral triangle”. Doing so not only gives the eye a larger appearance, but it also can be used to modify the overall shape of the palpebral fissures to the desired outcome[13].
Finally, a clear distinction should be made that the desired “larger eye” appearance for Asian patients is not synonymous with wanting to appear more Western or conforming to Western beauty standards. Instead, the goal is to create an eye shape that provides balance within the larger context of the face that aligns with the patient’s goals and cultural identity.
Cosmetic canthoplasty within the Western realm is largely performed to remedy the effects of senescence. The desired effect from age-related canthoplasty is contradictory to Asian Canthoplasty in that the favorable outcome is one with an upward canthal tilt. An upward tilt in an Asian patient would decrease scleral show and give the appearance of a smaller eye. However, in a patient with age-related canthal distortion, the upward canthal tilt gives lift to the orbital and local midface structures that have descended with time [13].
Differential Diagnosis
The differential diagnosis for canthal abnormalities is broad and includes many considerations, some of the major causes are listed below:
- Naso-ethmoidal trauma/ fractures
- Iatrogenic damage (previous surgery, cancer resection)
- Congenital malposition/deformity
- Blepharophimosis-ptosis-epicanthus inversus syndrome (BPES)
- Age-related laxity
- Canthal trauma
- Cicatricial Ectropion
- Architectural distortion (such as from prior radiation)
Preoperative Evaluation
History
A thorough history should be taken with attention to the mechanism of injury, the time since injury, and any negative sequelae. Additionally, it is imperative to assess whether a patient is suitable to undergo surgery. Information about comorbidities should be collected to guide decisions around anesthesia. Patients should be asked about medications and conditions that cause excessive bleeding to avoid potential retrobulbar hemorrhage and blindness. Usage of continuous positive airway pressure (CPAP) poses a risk for postoperative edema. Hypertension should be regulated and non-steroidal anti-inflammatory drugs (NSAIDS) should be discontinued for at least two weeks before the surgery. Because dry eye is frequently reported postoperatively, preoperative assessment should include questions about previous symptoms of dry eye and potential causes.
Physical Examination
Ocular Examination
The preoperative evaluation should include a full eye exam to assess the overall health of the eye. After, the physical examination should be performed and special attention should be given to the following components[11]:
- A slit lamp exam to help analyze the corneal surface, assess for dryness, and check for punctal eversion or stenosis
- A Schirmer test may be performed to determine if there is a component of ocular surface disease[2].
- The margin to reflex distance (MDR) may also be performed to assess for ptosis. MDR-1 (normal 3-4 mm) is measured as the distance between the corneal light reflex and the upper eyelid margin. MDR-2 (normal 3-5 mm) is the distance between the corneal light reflex and the lower eyelid margin
- Note: this may be useful to plan for concurrent or staged blepharoplasty
- A Hertel exophthalmometer may be used to measure existing proptosis
- Attention should be given to any visible neoplasms, skin discoloration, or actinic damage to the area that could impact the quality of surgical results.
- Note: The patient should be asked about any previously noted healing difficulties, such as keloid formations.
- It is important to make note of any facial asymmetry or deformities that exist prior to surgery.
- Other important observations to assess are positions of the eyelids, canthal angle disparities, and intercanthal distances.
- The strength and function of ocular muscles, such as that of the orbicularis, should be noted prior to surgery
Lateral Canthus Measurements
For a lateral canthoplasty, the distance from the lateral canthus to the orbital rim is an important measurement to obtain for successful lengthening of the palpebral fissure. Additionally, for patients who are undergoing canthoplasty to achieve a specific canthal angle, it is important to measure the degree of eye slant[13].
A cosmetically aesthetic anatomy consists of a lateral canthal angle that is approximately 4.1 degrees or 1.2 mm higher than the medial canthal angle[13]. This structure also allows for proper tear film distribution and lacrimal drainage. Ultimately it is critical to attentively examine the periorbital appearance and take note of any keratopathy, scleral show, or lid retraction that may exist, as increasing exposure may exacerbate pre-existing pathology.
Preoperative imaging is not routinely performed for cosmetic canthoplasty. In cases of trauma, iatrogenic injury, or pathology that alters normal architecture, a CT or MRI may help characterize the anatomical features prior to surgery.
Lower Eyelid Laxity
Inspection of different aspects of the facial anatomy should be completed to fully characterize the patient’s lower lid laxity. Any confounding edema, excess skin, wrinkles, lesions, or damage to the periorbital skin should be noted. Excess skin is identified by pinch tests. If the lower eyelid is retracted, its position should be measured and the causes should be addressed.
Preoperative and postoperative photography is suggested. It can help with preoperative planning, staging, and to track progress. Five different positions should capture the prominence of the lateral, central, and medial fat compartments. These positions include close-ups of the eyes when open, closed, looking upward, and looking to the sides. Surgeons should palpate the inferior orbital rim because it determines the extent of fat resection that can be performed to optimize aesthetic results.
The ideal position of the lateral canthus is up to 3 mm higher than the horizontal plane of the medial canthus. This canthal tilt may be altered by elongation or instability of the canthal tendons. Several lid laxity examinations should be performed preoperatively to prevent postoperative lower lid malposition. These are described below.
Distraction Test
The distraction test assesses the laxity of the tarsoligamentous sling. This test involves gently pulling on the lower eyelid either medially or laterally horizontally to its fullest extent in order to evaluate the degree of retraction away from the globe. There is a medial distraction test, which evaluates for lateral canthal tendon laxity as well as a lateral distraction test, which evaluates for medial canthal tendon laxity. Although there is no singularly approved grading scale, there have been proposed guidelines below[2]:
Medial Canthal Tendon Assessment
Action: Gently pull the lower eyelid laterally while the patient is looking forward. Observe the movement of the punctum
- Grade 0: normal
- Grade I: 2 mm displacement
- Grade II: 3 mm displacement
- Grade III: >3 mm displacement
- Grade IV: never returns to normal after blinking
Lateral Canthal Tendon Assessment
Instructions: Gently pull the lower eyelid medially while the patient is looking forward. Observe the movement of the lateral canthal corner
- Grade 0: normal (0-2 mm displacement)
- Grade I: 2-4 mm displacement
- Grade II: 4-6 mm displacement
- Grade III: >6 mm displacement
- Grade IV: never returns to normal after blinking
Snapback Test
The snap test should be performed as part of the ocular examination in order to evaluate for orbicularis muscle tone. The lower lid is gently pulled followed by observation of its return to position without necessitating a blink. A negative test consists of a lid that instantaneously returns to its original position. If the eyelid remains in a suspended state until the patient blinks or if it reverts to its usual position in an exceedingly slow manner, then it counts as a positive test.
The results can be divided into 4 grades
- Grade 0: normal
- Grade I: takes 2-3 seconds
- Grade II: takes 4-5 seconds
- Grade III: takes >5 seconds but returns to normal after blinking
- Grade IV: never returns to normal
Lid Retraction
Laxity within the medial and lateral canthi as well as lower eyelid tone can be assessed with simple lid retraction. Additionally the punctal position can be assessed with this technique. The examiner gently pulls the lower eyelid inferiorly towards the inferior orbital rim. If the puncta moves more than 2mm from the medial canthus, or if there is slow return to resting position, there is canthal tendon laxity present. Additionally the position of the puncta should be appositional to the eye where it is able to appropriately drain from the tear lake.
Surgical Preparation
After the preoperative evaluation has been completed, the surgeon must determine the proper surgical approach. The mechanism of deformity and desired outcomes will heavily influence the treatment plan. The surgeon may take into account the following considerations for some of the common indications listed below (not an exhaustive list).
Trauma or Iatrogenic injury
Goals during canthoplasty in cases of trauma are centered around reconstruction and regaining the natural contour of the eye. Functional properties should also be re-established, such as apposition of the punctum to prevent epiphora. Although achieving symmetry may not always be possible, best efforts should be given to mirror the canthus of the contralateral side of the face. Additionally, these cases pose a unique challenge in which bone and surrounding soft tissues may be missing. Here, obtaining the proper preoperative imaging may be useful for planning and proper surgical approach selection is quintessential. Some surgical techniques listed below address scenarios where anchor points for the canthal tendons are missing.
Congenital
Congenital malposition or syndromic causes of canthal deformity should be addressed for a variety of reasons, especially if the canthal deformity interferes with visual pathway development. There exist many transpositional approaches to modify the canthus to achieve restoration of the normal contour of the eye. Special care should be taken in individuals with epicanthal folds or those with a shallower naso-orbital angle.
Cosmetic
A guiding principle for cosmetic canthoplasty should be to avoid inducing negative functional sequelae from an elective procedure. Risks and benefits should always be discussed and extreme care should be taken during the preoperative evaluation to avoid exacerbating underlying conditions. Goals should be discussed thoroughly and expectations prior to surgery should be managed appropriately.
As detailed above, it is important to take into account various factors such as cultural considerations and individual appearance expectations. It is crucial to prioritize an eye shape that harmonizes with the overall facial features, aligning with the patient's objectives and cultural identity. For instance, cosmetic age-related canthoplasty favors an upward canthal tilt, which is incompatible amongst the Asian population as it consequently produces the impression of a smaller eye. Therefore, surgeons must thoroughly discuss the goals, potential risks and both desired and expected outcomes with patients.
Surgical Techniques
Medial Canthoplasty Techniques
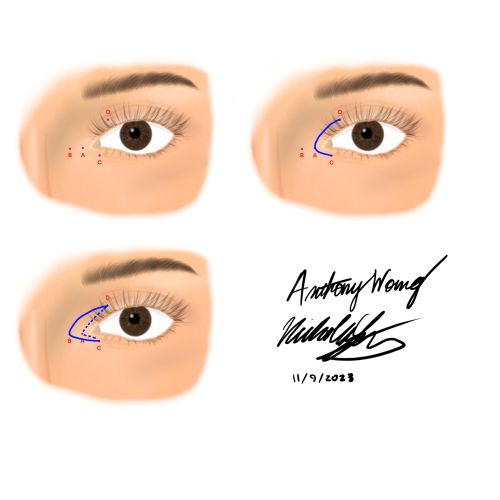
C-U Medial Canthoplasty
Patients with Blepharophimosis-ptosis-epicathus inversus syndrome, or BPES, present with several hereditary abnormalities that may be amenable by surgical procedures. These defects manifest as drooping upper eyelids (blepharophimosis), extended medial lower eyelids (epicanthus inversus), and prolonged intercanthal distances (telecanthus). Typically, multiple surgeries are performed to correct for the multiple malformations. The goal of the C-U medial canthoplasty is to amend epicanthus and telecanthus when used in tandem with lateral canthoplasty.
Surgical Approach Adapted from (Amer et al.,[14]):
- General anesthesia is induced and patients are dressed in sterile fashion
- Calculate the amount of tissue to be removed for ideal intercanthal distance by multiplying about half the interpupillary distance by 1.5
- Draw four points on the patient with a surgical marker as follows:
- Point A - 2 mm from medial canthus
- Point B - distance equal to calculation from step 2 medial to point A
- Point C - 2 mm from the lid margin aligned with the lower punctum
- Point D - 3 mm laterally from upper punctum and 2 mm superior to lid margin
- Draw the C portion of the procedure through points C, A, and D
- Draw the U portion of the procedure through points C, B, and D
- Between the C and U arms, remove the skin and orbicularis muscle to reveal the medial canthal tendon. Pay special attention to the location of the lacrimal canalicular system
- Shorten the medial canthal tendon by folding in the excess tendon and fixating it to the anterior lacrimal crest periosteum using 4-0 prolene
- Restore the orbicularis oculi muscle by closing the incision with 6-0 vicryl interrupted sutures
- Close the skin with 6-0 prolene or vicryl interrupted sutures
- Lateral canthoplasty is performed at the same time to extend the horizontal palpebral fissure length
- Frontalis suspension surgery is performed at least 6 months after the initial procedure to correct the blepharoptosis
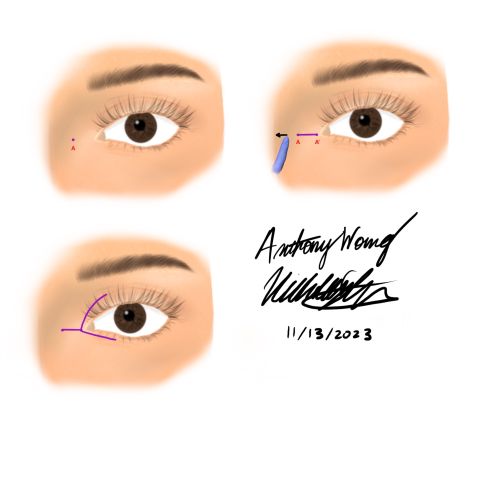
Y-V Medial Canthoplasty
Telecanthus can be caused by any disruption to the medial canthal tendon. Some etiologies include aging, inherited defects, orbital fractures, and iatrogenesis. This procedure aims to shift or reinsert the medial canthal tendon to a proper location. Transnasal wiring is utilized as a solution for eventual slackening of the tendon.
Surgical Approach Adapted from (Kim et al.,[15]):
- General anesthesia is induced and patients are dressed in sterile fashion
- Draw 2 points on the patient - one labeled point A at the location of the new medial canthus and a second labeled point A’ 1 mm medial to the exposed lacrimal lake
- Two 1 cm arms are drawn - a superior limb along the upper eyelid margin and an inferior limb 2 mm from the lower lid lashes
- Make an incision horizontally through points A and A’ and through both of the arms in step 3
- With blunt metzenbaum scissors, dissect to the medial orbital wall periosteum
- Retract the cut edges of tissue and incise the now exposed periosteum
- Lift the periosteum with a periosteal elevator and separate out the medial canthal tendon
- Perform oblique transnasal wiring as follows:
- Make a slit with a no. 11 scalpel on the nasal recession of the opposite frontoglabella area
- Angle a Kirschner wire at 45 degrees superiorly and posteriorly to the lacrimal fossa and drill a hole. Make another hole 5 mm below
- Feed a 2-0 wire through the medial canthal tendon on the affected side and place an 18 gauge needle in the first drill hole, then pass the wire through. Repeat on the second hole
- Secure the medial canthal tendon in the desired position by tightening and twisting the wire
- Close the wound
- Any “dog ear” deformities may be corrected by trimming the excess skin and suturing with 7-0 nylon
Medial Canthoplasty Repair for Canthal Rounding
Canthal rounding is commonly seen after iatrogenic injury or trauma to the canthus. The manner in which the skin heals and scar tissue forms can cause an asymmetric and round appearance to the medial canthus. Not only does this cause potential visual field defects, but it is also socially debilitating. It is important to note that the approach below can be applied to both the medial and lateral canthus.
Surgical Approach (Adapted from Juniat et al., [16]):
- Prepare and drape the patient in a standard sterile fashion
- Mark the area of canthal rounding
- Cut into and separate the anterior lamella from the posterior lamella with a 15 blade and then with Wescott scissors
- Cut the anterior flap along the new superior lid margin with westcott scissors and fold it downward. This creates the new inferior lid margin
- Cut the posterior flap along the new inferior lid margin with wescott scissors and fold it upwards. This creates the new superior lid margin
- Secure the newly created lid margins with 6-0 vicryl sutures in an interrupted fashion
- If there is lid laxity the canthoplasty can be combined with a canthopexy
Modified V-W Medial Canthoplasty
The modified V-W medial canthoplasty is a modified canthoplasty technique used to treat telecanthus. Because the repair shifts the medial canthus and tendon nasally, the resultant shape is sometimes unpredictable. By incorporating the V-W technique, this approach is especially useful in Asian patients because of the presence of an epicanthal fold as well as a shallow orbitonasal angle.
Surgical Approach (Adapted from Sakamoto et al. ,[17]):
- Prepare and drape the patient in a standard sterile fashion
- Mark the skin in the geometric W shape (schematic below)
- Clearly delineate the points as below
- Mark Points O (original) and P (present). These represent the corner of the medial canthus
- Mark Point Q, which is a position ⅔ of the distance through line OP
- Point R is set at the same distance as line OQ from point P
- Draw and arc from point R to point P
- Along this arc, mark an arbitrary point S where the angle SRP is more than 45 degrees
- Mark point N along any arbitrary spot on the supraorbital rim
- Draw an arc equal to the length of NQ from point N to point X
- Draw another arc equal in length to RP from point S to point Y
- Mark point T, which is the intersections of arcs drawn in steps 10 and 11 and X and Y are the ending points of the arcs
- Ensure that the line lengths are equal for lines OQ, PR,RS, and ST. Also ensure that line NQ = NT in length. These distances must be equal so that there is no length discrepancy once the skin is sutured.
- Excise the area of skin within the points Q, N, T, S, and R
- Excise excessive portions of the orbicularis oculi muscle, and release all points of fascial adhesion
- Transpose Point S to Point R and fix It to the medial candle ligament using non-absorbable suture
- Close the skin (A dog ear dimple appears and is expected). The concern for the orbital-nasal angle is corrected
Medial Canthoplasty with Microplate
Often, canthoplasty requires attachment of the medial canthal tendon to the medial orbital rim. However, in traumatic etiologies, there is likely a portion of soft tissue or bone missing which precludes this type of approach. This technique uses a microplate to bridge the gap, allowing for fixation of the medial canthal tendon.
Surgical Approach (Adapted from Howard, Nerad, and Kersten[18]):
- Prepare and drape the patient in a standard sterile fashion
- Position the plate horizontally with the top of the T pointed anteriorly toward the nasal bone and the base of the T plate pointed toward the ethmoid plate
- Howard et al., selected the Luhr Microplate (6 hole, T shape with a 0.5mm thickness)
- Position the top of the T over the anterior lacrimal crest. This will ensure that the point of fixation happens in the more sturdy underlying maxillary bone
- Bend the plate to the appropriate contour with pin-in-plate forceps and by grasping the center hole of the 3 holes at the top of the T
- Trim any excess portion of the plate that lies posterior to the posterior lacrimal crest when the plate is placed such that top of the T is on the anterior lacrimal crest
- Using the plate as a guide, drill holes with a 5 mm drill bit (0.60 mm in diameter)
- Drill three holes at the top of the T plate which should lie along the anterior lacrimal crest
- Use 4 mm self-tapping screws in the holes previously drilled
- Ensure that there are no screws posterior to the anterior lacrimal crest
- Secure the medial canthal tendon stump with 3-0 polypropylene (authors used FS1 cutting needle) with a vertical mattress suture to the posterior hole along the posterior lacrimal crest
- If the patient lacks the medial portions of the eyelid, sutures may be used to fix the tarsus to the holes of the plate
- If the patient Lacks soft tissue, cover the plate with a myocutaneous flap
- Close the skin
Lateral Canthoplasty Techniques
Dermal Orbicular Pennant
The dermal orbicular pennant is particularly useful in patients who require canthal support or have received unsatisfactory results from horizontal shortening procedures. This is the procedure of choice for patients with lateral canthal dystopia. However, because pupil size fluctuates with light and anesthesia, fixating sutures at the level of the upper border of the pupil may be unreliable and potentially detrimental to the overall visual aesthetic.
Surgical Approach (Adapted from Jelks et a., [19]):
- Prepare and drape the patient in a standard sterile fashion
- Outline a flap laterally from the lateral canthus measuring approximately 1 cm horizontally and 0.5 cm vertically and remove epidermis
- Incise underlying dermis and orbicularis to expose the lateral canthal tendon
- Release lateral retinaculum from the orbital rim
- Fix a double-armed 4-0 Polydek suture on an ME-2 needle to the periosteum inside lateral orbital rim at the level of the upper pupil border
- Secure dermal pennant with sutures, overadjust for lower eyelid elevation and temporal oblique angulation
- Ensure that the lower eyelid achieves sufficient closure with occlusion of inferior cornea by 1 to 2 mm
- Close skin
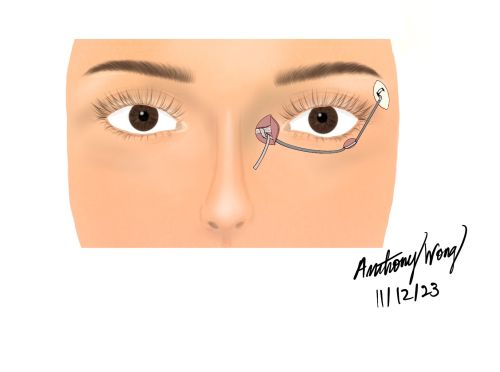
Inferior Retinacular Lateral Canthoplasty
A popular technique for both reconstructive and cosmetic canthoplasty, the inferior retinacular lateral canthoplasty was first described by Jelks et al., in 1997. It was created to be a component of cosmetic blepharoplasty that results in a tightened lower lid. This procedure is best for patients with negative vectors and ideal anatomic relationships. It can be used to reduce lower lid and lateral canthal deformities that are either acquired or caused by other procedures. It is advantageous to the dermal pennant because it does not involve any structures lateral to the lateral canthus, which decreases the likelihood of postoperative edema or paralysis of the orbicularis. Two drawbacks include the appearance of overcorrection in the immediate postoperative phase as well as the lesser degree of tightening when compared to other procedures.
Surgical Approach (Adapted from Jelks et al.,[20])
- General anesthesia is induced and patients are dressed in sterile fashion
- Make an upper eyelid crease incision
- Raise a skin-muscle flap to expose the lateral canthal tendon
- Once the inferior portion of the lateral retinaculum is found, it may be separated
- Divide the lateral canthal tendon into superior and inferior parts
- Cut the inferior aspect of the tendon with scissors to release the lower lid
- Attach the inferior component to a 4-0 Polydek suture on a ME-2 needle
- Fix the complex to the inside of the lateral orbital rim at the level of the superior edge of the pupil
- Ensure that the lower eyelid has sufficient closure to cover the inferior cornea by 1-2 mm
- Close skin
Lateral Retinacular Suspension
Surgical Approach (Adapted from Fagien et al.,[21])
Note: this approach is commonly performed along with an upper eyelid blepharoplasty
*under the assumption that an upper blepharoplasty incision is already made
- General anesthesia is induced and patients are dressed in sterile fashion
- Make a transcutaneous incision below the lateral canthal tendon
- With a double-armed 5-0 nylon suture, pass both arms through the inferior incision superolaterally through the lateral retinaculum and then outward from the upper blepharoplasty incision
- Secure the sutures to the periosteum inside of lateral orbital rim at the level of the superior edge of the pupil
- Close skin
Lateral Tarsal Strip
The lateral tarsal strip combines horizontal lid shortening and lateral support either with or without the use of grafts. The traditional technique can result in a length disparity between the upper and lower canthal tendons, along with misalignment of the mucosal or mucocutaneous elements of the canthal junction. The mucocutaneous region may show scarring. Too much tarsal removal predisposes to rounding of the canthal angle. Incisions at the canthal angles may compromise lymphatic drainage or weaken the orbicularis oculi.
Surgical Approach (Adapted from Anderson et al.,[22])
- General anesthesia is induced and patients are dressed in sterile fashion
- Perform a 1 cm lateral canthotomy and inferior cantholysis with scissors
- Separate the tarsus from the orbicularis oculi as well as the inferior border of the tarsus from its attachments
- Incise the inferior and superior orbital rim attachments of the lateral canthal tendon
- Split the eyelid at the gray line with scissors into anterior and posterior lamellae
- Cut a 3-4 mm wide strip of tarsus that is equal to the incision in the previous step
- Move the stip laterally until the lateral border of the lower eyelid reaches the limbus
- Pass a double-armed 5-0 nylon suture posterior to anterior through the strip
- Attach the strip to the periosteum inside the lateral orbital rim
- Reform the lateral canthal angle with 6-0 gut suture
- Adjust the double-armed suture so that the lower lid margin meets the limbus
- Close the skin
Tarsal Sandwich
At times, traditional techniques are not adequate to correct certain lower eyelid malpositions, such as with trauma and infection. The tarsal sandwich procedure is a combination between the tarsal strip technique and lateral tarsorrhaphy that allow for increased lateral canthal elevation.
Surgical Approach (Adapted from Hesse et al.,[23])
- General anesthesia is induced and patients are dressed in sterile fashion
- Make a 1 cm horizontal incision at the lateral canthal laugh line and reveal the lateral orbital rim periosteum
- Stretch the lid and remove the remnants of the inferior crus of the lateral canthal tendon using scissors
- Divide the lid into anterior and posterior lamellae to create a tarsal strip
- Split the upper lid at the gray line, starting at the canthus and extending medially by 1 cm
- Create a tarsorrhaphy pocket and pass a double-armed 4-0 nylon mattress suture through the tarsal strip approximately 4 to 5 mm from its edge
- Vary the measurement of the suture placement to accommodate the required shortening of the lower lid
- Place both arms of the suture into the tarsorrhaphy pocket and out through the skin, tying them over a bolster and leaving them for 10 days
- Secure both margins at the medial extent of the "sandwich" with an additional suture
- Trim the redundant anterior lamella of the lower lid
- Close the skin with interrupted sutures
Adapted Aesthetic Lateral Canthoplasty for Asians
Surgical Approach (Adapted from Hesse et al.,[24])
- General anesthesia is induced and patients are dressed in sterile fashion
- Anesthetic eye drops (Alcaine 0.5%, proparacaine hydrochloride) are administered and a mixture of 1:100,000 epinephrine with 1:1 0.5% bupivacaine hydrochloride and saline is injected
- Create traction sutures to the upper and lower eyelids
- Make an incision along the lateral canthus crease line to a marked end point laterally
- Incise and dissect the lateral palpebral raphe and superficial lateral palpebral ligament
- Perform a canthopexy with 6-0 nylon at the periosteum and lower lid, making sure to suture at 2 locations and fixate within 3 mm of the lower lid margin
- Close the skin with 7-0 black silk
Alternative or Concurrent Treatments
Blepharoplasty
With the normal aging process, both upper and lower lid skin undergoes stretching, and underlying supporting muscles experience a decline in strength. Blepharoplasty is a surgical intervention that addresses this by eliminating surplus skins for the lids. Ectropion is a common indication for lower lid blepharoplasty. Essentially, the lower lid turns outward exposing the conjunctiva as a consequence of reduced elasticity and heightened laxity.
Surgical approach for transconjunctival lower eyelid blepharoplasty (Adapted from Patel et al., [25])
- This procedure may be done in the office using a mixture of lidocaine and epinephrine local anesthetic, however, IV sedation is typically recommended due to highly associated discomfort and the need for proper equipment and techniques.
- Markings of the three lower lid fat pads are made with the patient in a sitting position.
- A corneal shield is placed for protection and comfort.
- A Desmarres retractor is used to retract the lower eyelid.
- An infratarsal incision is made approximately 6 mm below the inferior tarsal border, through the conjunctiva and lower lid retractors.
- 4-0 silk traction sutures can be applied in the proximal conjunctival edge in order to enhance visibility.
- The three lower eyelid orbital fat pads are debulked or repositioned to regions beneath the orbital rim that exhibit concavity.
- It is important to visualize the inferior oblique muscle in order to avoid injury.
- 6-0 catgut sutures can be used to close the conjunctiva, or the wound may be left open to close on its own.
Tarsorrhaphy
A tarsorrhaphy is a procedure that connects the upper and lower lids in order to close the eye for corneal protection. A temporary tarsorrhaphy utilizes bolsters over the upper and lower lid to fully close the eye, which can be opened and closed during examination. A permanent tarsorrhaphy utilizes interrupted sutures to join the lateral third of the upper and lower lid and maintain a central opening for visibility.
Surgical approach for temporary tarsorrhaphy (Adapted from Rajak et al., [26])
- A mixture of lidocaine with epinephrine is injected for local anesthesia. Iodine is used for sterilization.
- Sutures are tied over bolsters in order to protect the skin from being cut. A total of two 2 cm and one 1 cm bolster is needed.
- One of the 2 cm bolsters is aligned over the upper lid with a suture placed through it and the skin 3-4 mm above the lid margin, through the tarsal plate. The needle is then passed through the lower lid and again into the tarsal plate, exiting the skin 2-3 mm below the lower eyelid margin.
- Another 2 cm bolster is aligned along the lower lid with a 1 cm bolster on top of it. A suture is passed through the upper bolster, then upper lid, followed by lower lid and finally the lower bolster.
- The two lower lid bolsters are moved superiorly to shut the lids. The 1 cm bolster is used to secure the lid closed. The 1 cm bolster can be pulled back down in order to open the lids.
Surgical approach for permanent tarsorrhaphy (Adapted from Rajak et al.,[26])
- A mixture of lidocaine with epinephrine is injected for local anesthesia. Iodine is used for sterilization.
- A No. 11 or 15 blade is used to separate the anterior and posterior lamella. The incision is then expanded approximately 5 mm.
- The epithelium is removed by excising 1 mm of the posterior lamella, improving healing.
- A 5-0 or 6-0 absorbable suture is used to close the posterior lamella. The needle is first passed through the posterior lamella of the upper lid, and then through the posterior lamella of the lower lid. This is again with a second suture.
- A 4-0 or 6-0 suture is used to close the anterior lamella. The needle is passed through the upper lid, 2-3 mm above the lid margin, and then into the anterior lamella of the lower lid, exiting 2-3 mm below the lid margin. This step is done at least twice with the sutures set 3 mm apart until the eyelid skin completely closes over the posterior lamella.
Lower Eyelid Sling
A lower eyelid sling may be utilized as management of combined medial and lateral canthal tendon laxity to target repairing lower lid malposition and laxity.
Surgical Technique with fascia lata graft (adapted form Morisada et al.[27])
- The patient is prepped and draped with sterile precautions.
- A fascia lata graft is taken from the lateral thigh or palmaris longus tendon, and is cut to be about 35mm x 10mm.
- An incision is made about 6 cm superior to the lateral tibial condyle to retrieve the lateral thigh fascia lata.
- The inferior tarsus, medial canthal tendon, and lateral canthal tendon are exposed by either a subciliary incision, lateral canthotomy/cantholysis or medial transcutaneous incision.
- 5-0 polydioxanone sutures are used to attach the tarsal plate medially to the nasal bones and supero-laterally to the orbital rim using the fascia lata graft.
- A 5-0 fast gut suture is used to close the final skin incisions of the canthotomy/canthoplasty.
Postoperative Care
After surgery, patients are given antibiotic, steroid, and artificial tear eye drops. Oral antibiotics and ophthalmic ointment may also be prescribed. Steroid eye drops should be tapered and discontinued once palpebral conjunctival swelling subsides. Patients are advised to avoid impact to the surgery site and to not rub the eye for three weeks to avoid dehiscence. Patients should also refrain from activities that increase blood flow to the eyes, such as heavy lifting or bending. Swimming pools, saunas, and contact lenses should be avoided for three weeks, although face washing and light showers are permitted. The head may be kept in a raised position to improve any bruising or swelling. Sunglasses are recommended during the recovery period to protect from irritation resulting from sun and wind exposure.
Postoperative Complications
Ectropion
Proactive management of potential secondary ectropion development is important. Certain individuals may have abundant lid laxity putting them at risk for developing secondary ectropion over time after canthoplasty. Preventative measures such as proper evaluation for selection of the most appropriate technique specific to each individual should be taken in order to decrease risk of postoperative secondary ectropion development[28].
Trichiasis
Trichiasis refers to a condition that develops as a result of misdirected eyelashes toward the surface of the eye, consequently leading to irritation, discomfort, and corneal morbidity[29]. Trichiasis can potentially occur after canthoplasty surgery which may manifest at any point. Efficacy of the procedure technique or the body’s healing mechanisms may be linked to trichiasis shortly after the operation, while ongoing trachomatous scarring may be linked to chronic trichiasis. Cryoepilation may be used as efficacious management to resolve corneal irritation secondary to postoperative trichiasis after canthoplasty[30].
Chemosis
Swelling of the eyelids and conjunctiva are commonly seen following eyelid surgeries. Usage of cryotherapy and cautery can disrupt the lymphatic drainage system, increasing the likelihood of this complication [31]. Patients typically experience this directly after surgery and most cases are self-limiting.
Symblepharon
If enough trauma is inflicted to the area during canthoplasty, symblepharon can develop, which is an abnormal adhesion between the bulbar and palpebral conjunctiva. In a study of postoperative complications of cosmetic oculoplastic surgeries, symblepharon was seen in 5.9% of patients undergoing lateral canthoplasty [32].
Corneal Erosion
Exposed suture material after ocular surgery may lead to corneal erosion[32], which presents as foreign body sensation, photophobia, and painful, red, watery eyes. Treatment involves lubricating drops, antibiotics, bandage contact lenses, and removal of the foreign material. If left untreated, this can lead to granuloma formation, infection, and ulceration.
Lacrimal Fistula
Patients who have undergone previous orbitofacial surgeries may have damage to the lacrimal ligaments, causing prolapse of the lacrimal gland[33] . This is more common when the palpebral conjunctivae of the upper fornix is displaced laterally and inadvertently sutured to the skin immediately surrounding the lateral canthus. This can result in the formation of a fistula between the gland and the overlying skin.
Bleeding and Scarring
As with any procedure, there is a risk for extensive and unpredictable bleeding that can compromise eyesight. Scars may also improperly heal because of excess scar tissue, genetic predisposition, or misplaced incision. If the patient is dissatisfied with the cosmetic appearance, revision surgeries can be performed but do not guarantee resolution of the problem.
Lacrimal Drainage System Injury
The close relationship of the medial canthal tendon to the lacrimal drainage system makes this structure particularly susceptible to injury during medial canthoplasty. Obstruction or damage to the drainage system leads to excessive tearing and irritation. It is a challenge to repair and restore the function of the lacrimal drainage system. Conjunctivodacryocystorhinostomy (CDCR) is a reliable method that may be used to rebuild a drainage system by adding a tear drainage tube that circumvents the upper lacrimal system [11].
Misalignment
Movement of one eyelid or tendon in relation to the opposing eyelid or tendon on the same eye may lead to canthal disparity and misalignment of the mucocutaneous junction.
The desired result from overcorrecting the lateral canthal angle is dependent on inadequate healing and an unpredictable descent of the anatomic structures. Improper fixation of the canthal tendons with the periosteum is unlikely to maintain position of the canthus if there is excessive tendinous strain or orbicularis oculi paralysis [34]. This can result in overly round lateral canthal angles and a “dog leg” deformity of the lower eyelid[35] .
Wound Dehiscence
Patients must be properly educated on postoperative wound care to ensure the best chance of uncomplicated healing. Rubbing of the eye or impact to the surgery site may result in dehiscence of the wound and a subsequent scar. However, this can be easily corrected by a simple scar revision.
Prognosis and Outcomes
The prognosis and outcome for both a medial canthoplasty and lateral canthoplasty depends on various factors such as the surgical technique utilized and the patient’s overall health. In a study done by Maamari et al., 73 patients underwent medial canthoplasty for treatment of exposure keratopathy. Postoperatively, 95% of these patients had improved symptoms of dryness, pain, irritation and tearing. Moreover, 85% had decreased lagophthalmos and 90% exhibited enhancements in ocular surface findings. Only 0.01% had a complication of wound dehiscence[36]. However, this issue was addressed through revision without resulting in any enduring complications. In another study done by Cho et al., 202 women and 44 men underwent cosmetic lateral canaloplasty. All 246 procedures were done successfully with no severe complications[37].
Other possible but uncommon complications include asymmetry, scarring, infection, or changes in eyelid function such as eyelid drooping or double vision due to eyelid muscle damage. If excess skin was removed, patients may have difficulty with complete eyelid closure. Nonetheless, with a skilled and experienced surgeon these complications are exceedingly rare. As with any surgical procedure, temporary swelling, bruising and discomfort are possible but subside throughout recovery. Swelling typically resolves almost completely throughout the duration of one month and bruising typically settles within 7-10 day postoperatively[38]. Stitches are typically removed after 5 to 7 days postoperatively, and the incision may remain erythematous for up to 3 months[38]. Overall, the operation is considered safe with good cosmetic results and reliability.
For the medial canthoplasty for rounding technique listed above, all patients in the study except one reported good surgical outcomes. This was defined as subjective acceptable cosmetic and functional outcomes by both the patient and surgeon. The one patient among 12 had a recurrence of medial canthal rounding.[16]
References
Add text here
- ↑ Qin Y, Li D, Chen T. Management of the delayed traumatic medial telecanthal deformity. Aesthet Surg J. 2010 Jul-Aug;30(4):516-21. doi: 10.1177/1090820X10380387. PMID: 20829248.
- ↑ Jump up to: 2.0 2.1 2.2 Labib A, Patel BC, Milroy C. Lower Eyelid Laxity Examination. [Updated 2023 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK576403/
- ↑ Glat PM, Jelks GW, Jelks EB, Wood M, Gadangi P, Longaker MT. Evolution of the lateral canthoplasty: techniques and indications. Plast Reconstr Surg. 1997 Nov;100(6):1396-405; discussion 1406-8. doi: 10.1097/00006534-199711000-00003. PMID: 9385950.
- ↑ Kashkouli MB, Abdolalizadeh P, Abolfathzadeh N, Sianati H, Sharepour M, Hadi Y. Periorbital facial rejuvenation; applied anatomy and pre-operative assessment. J Curr Ophthalmol. 2017 Apr 25;29(3):154-168. doi: 10.1016/j.joco.2017.04.001. Erratum in: J Curr Ophthalmol. 2018 Mar 06;30(2):188-189. PMID: 28913505; PMCID: PMC5587258.
- ↑ Machiele R, Lopez MJ, Czyz CN. Anatomy, Head and Neck: Eye Lacrimal Gland. 2023 Jul 24. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 30422509.
- ↑ Zhang W, Huang Q, Li J. Case report of conjunctival sac fistula after cosmetic lateral canthoplasty. BMC Ophthalmol. 2020 Apr 3;20(1):127. doi: 10.1186/s12886-020-01402-3. PMID: 32245437; PMCID: PMC7119172.
- ↑ Paul A. Harris, Bryan C. Mendelson, CHAPTER 5 - Eyelid and Midcheek Anatomy, Editor(s): Steven Fagien, Putterman's Cosmetic Oculoplastic Surgery (Fourth Edition), W.B. Saunders, 2008, Pages 45-63, ISBN 9780721602547, https://doi.org/10.1016/B978-0-7216-0254-7.50011-0.
- ↑ Jeffrey A. Nerad, 12 - Eyelid Reconstruction, Editor(s): Jeffrey A. Nerad, Techniques in Ophthalmic Plastic Surgery (Second Edition), Elsevier, 2021, Pages 465-504, ISBN 9780323393164, https://doi.org/10.1016/B978-0-323-39316-4.00012-0.
- ↑ Whitaker LA. Selective alteration of palpebral fissure form by lateral canthopexy. Plast Reconstr Surg. 1984 Nov;74(5):611-9. doi: 10.1097/00006534-198411000-00004. PMID: 6494318.
- ↑ Rostami S, de la Torre JI, Czyz CN. Lower Eyelid Blepharoplasty. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448181/
- ↑ Jump up to: 11.0 11.1 11.2 Sun H, Li Y, Huang Q, Ding JW, Hou ZJ, Li DM. Medial Canthoplasty Combined with Conjunctivodacryocystorhinostomy for the Treatment of Delayed Medial Telecanthal Deformity. Chin Med J (Engl). 2017 Mar 20;130(6):698-702. doi: 10.4103/0366-6999.201594. PMID: 28303853; PMCID: PMC5358420.
- ↑ Naugle TC. Lateral canthoplasty. J Dermatol Surg Oncol. 1992 Dec;18(12):1075-80. doi: 10.1111/j.1524-4725.1992.tb02786.x. PMID: 1430569.
- ↑ Jump up to: 13.0 13.1 13.2 13.3 Kim YJ, Lee KH, Choi HL, Jeong EC. Cosmetic Lateral Canthoplasty: Preserving the Lateral Canthal Angle. Arch Plast Surg. 2016 Jul;43(4):316-20. doi: 10.5999/aps.2016.43.4.316. Epub 2016 Jul 20. PMID: 27462563; PMCID: PMC4959973.
- ↑ Amer AA, Abdellah MM, Hassan NHF, Mounir A. Surgical outcome of epicanthus and telecanthus correction by C-U medial canthoplasty with lateral canthoplasty in treatment of Blepharophimosis syndrome. BMC Ophthalmol. 2022 May 19;22(1):226. doi: 10.1186/s12886-022-02455-2. PMID: 35590300; PMCID: PMC9118630.
- ↑ Kim TG, Chung KJ, Kim YH, Lim JH, Lee JH. Medial canthopexy using Y-V epicanthoplasty incision in the correction of telecanthus. Ann Plast Surg. 2014 Feb;72(2):164-8. doi: 10.1097/SAP.0b013e31825c081d. PMID: 23407259.
- ↑ Jump up to: 16.0 16.1 Juniat V, Joshi S, Hersh D, Selva D, Joshi N. Canthoplasty repair for canthal rounding. Eye (Lond). 2022 Mar;36(3):564-567. doi: 10.1038/s41433-021-01497-y. Epub 2021 Mar 21. PMID: 33746208; PMCID: PMC8873483.
- ↑ Sakamoto Y, Nakajima H, Tamada I, Kishi K. New technique for medial canthoplasty that incorporates modified v-w epicanthoplasty. Arch Facial Plast Surg. 2012 Jan-Feb;14(1):59-61. doi: 10.1001/archfacial.2011.1125. PMID: 22250269.
- ↑ Howard GR, Nerad JA, Kersten RC. Medial canthoplasty with microplate fixation. Arch Ophthalmol. 1992 Dec;110(12):1793-7. doi: 10.1001/archopht.1992.01080240133046. PMID: 1463424.
- ↑ Jelks GW, Jelks EB. Repair of lower lid deformities. Clin Plast Surg. 1993 Apr;20(2):417-25. PMID: 8485950.
- ↑ Jelks GW, Glat PM, Jelks EB, Longaker MT. The inferior retinacular lateral canthoplasty: a new technique. Plast Reconstr Surg. 1997 Oct;100(5):1262-70; discussion 1271-5. doi: 10.1097/00006534-199710000-00030. PMID: 9326791.
- ↑ Fagien S. Algorithm for canthoplasty: the lateral retinacular suspension: a simplified suture canthopexy. Plast Reconstr Surg. 1999 Jun;103(7):2042-53; discussion 2054-8. doi: 10.1097/00006534-199906000-00039. PMID: 10359271.
- ↑ Anderson RL, Gordy DD. The Tarsal Strip Procedure. Arch Ophthalmol. 1979;97(11):2192–2196. doi:10.1001/archopht.1979.01020020510021
- ↑ Hesse RJ. The tarsal sandwich: a new technique in lateral canthoplasty. Ophthalmic Plast Reconstr Surg. 2000 Jan;16(1):39-41. doi: 10.1097/00002341-200001000-00007. PMID: 10674731.
- ↑ Shin YH, Hwang K. Cosmetic lateral canthoplasty. Aesthetic Plast Surg. 2004 Sep-Oct;28(5):317-20. doi: 10.1007/s00266-003-0060-7. PMID: 15666047.
- ↑ Patel BC, Volner K, Malhotra R. Transconjunctival Blepharoplasty. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
- ↑ Jump up to: 26.0 26.1 Rajak S, Rajak J, Selva D. Performing a tarsorrhaphy. Community Eye Health. 2015;28(89):10-1. PMID: 26435586; PMCID: PMC4579993.
- ↑ Morisada, M. V., Hoshal, S. G., & Tollefson, T. T. (2021). Periorbital reconstruction in facial paralysis. Operative Techniques in Otolaryngology-Head and Neck Surgery, 32(4), 213–218. https://doi.org/10.1016/j.otot.2021.10.012
- ↑ Baek S, Chung JH, Yoon ES, Lee BI, Park SH. Algorithm for the management of ectropion through medial and lateral canthopexy. Arch Plast Surg. 2018 Nov;45(6):525-533. doi: 10.5999/aps.2018.00836. Epub 2018 Nov 15. PMID: 30466232; PMCID: PMC6258983.
- ↑ Karademir S, Agaoglu G. Treatment of Trichiasis by Releasing Follicle Roots of Eyelashes: A New Technique. Plast Reconstr Surg Glob Open. 2021 Mar 22;9(3):e3480. doi: 10.1097/GOX.0000000000003480. PMID: 33968553; PMCID: PMC8099408.
- ↑ Lackner PA. Techniques for surgical correction of adnexal disease. Clin Tech Small Anim Pract. 2001 Feb;16(1):40-50. doi: 10.1053/svms.2001.22805. PMID: 11373827.
- ↑ Bagheri A, Javadi M, Shahraki K. Treatment of Persistent Chemosis after Upper Lid Blepharoplasty by Hand-Held Fine-Tip Cautery: Report of a Case. Middle East Afr J Ophthalmol. 2019 Aug 26;26(2):120-122. doi: 10.4103/meajo.MEAJO_218_18. PMID: 31543673; PMCID: PMC6737782.
- ↑ Jump up to: 32.0 32.1 Baek JS, Kim KH, Lee JH, Choi HS. Ophthalmologic Complications Associated With Oculofacial Plastic and Esthetic Surgeries. J Craniofac Surg. 2018 Jul;29(5):1208-1211. doi: 10.1097/SCS.0000000000004515. PMID: 29554075.
- ↑ Ahn YJ, Jung SK, Paik JS, Yang SW. Lacrimal gland fistula after cosmetic lateral canthoplasty. J Craniofac Surg. 2013 Jul;24(4):1317-8. doi: 10.1097/SCS.0b013e3182953a4d. PMID: 23851797.
- ↑ Taban M, Nakra T, Hwang C, Hoenig JA, Douglas RS, Shorr N, Goldberg RA. Aesthetic lateral canthoplasty. Ophthalmic Plast Reconstr Surg. 2010 May-Jun;26(3):190-4. doi: 10.1097/IOP.0b013e3181baa23f. PMID: 20489545.
- ↑ Shorr N, Goldberg RA, Eshaghian B, Cook T. Lateral canthoplasty. Ophthalmic Plast Reconstr Surg. 2003 Sep;19(5):345-52. doi: 10.1097/01.IOP.0000087069.83107.A4. PMID: 14506418.
- ↑ Maamari RN, Custer PL, Neimkin MG, Couch SM. Medial canthoplasty for the management of exposure keratopathy. Eye (Lond). 2019 Jun;33(6):925-929. doi: 10.1038/s41433-019-0347-9. Epub 2019 Feb 1. PMID: 30710111; PMCID: PMC6707211.
- ↑ Cho YK, Suh BI, Park KM. The Effective Fixation Level for Cosmetic Lateral Canthoplasty. J Craniofac Surg. 2019 Jun;30(4):e362-e365. doi: 10.1097/SCS.0000000000005378. PMID: 30839464.
- ↑ Jump up to: 38.0 38.1 Chae SW, Yun BM. Cosmetic Lateral Canthoplasty: Lateral Canthoplasty to Lengthen the Lateral Canthal Angle and Correct the Outer Tail of the Eye. Arch Plast Surg. 2016 Jul;43(4):321-7. doi: 10.5999/aps.2016.43.4.321. Epub 2016 Jul 20. PMID: 27462564; PMCID: PMC4959974.