Canaloplasty
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction and Background
Lowering intraocular pressure (IOP) is the only proven therapy for glaucoma. Traditional glaucoma filtration surgeries such as trabeculectomy, are highly successful in lowering IOP but have a very high rate of complications. This has led to the search for safer forms of glaucoma surgery. While surgeries like trabeculectomy seek to create a fistula that enables aqueous to be diverted from the anterior chamber into the subconjunctival space bypassing the natural outflow system, canaloplasty is a surgical technique that promotes outflow of aqueous via the natural outflow pathways through the trabecular meshwork (TM) and into Schlemm's canal (SC). It dilates SC with multiple direct injections of an ophthalmic viscoelastic device (OVD) administered in a controlled fashion through a flexible microcatheter that is threaded through the entire length of SC. To maintain this dilation, an intraluminal suture is placed within SC and tied tightly to apply a permanent tensioning effect. This not only keeps SC open and prevents its collapse but it also has the effect of putting the TM on stretch to make it more permeable to aqueous. Figures 1-3 Since filtration of aqueous is being directed into SC and the existing natural outflow pathways this should make this form of surgery unlikely to produce hypotony and all its related complications making it much safer than traditional glaucoma filtration surgeries.
Canaloplasty is a modification of viscocanalostomy, a form of non-penetrating glaucoma surgery. In this older technique, first introduced by Stegman and colleagues,[1] OVD was injected into SC on either side of an external scleral dissection site with a metal cannula. Figure 4 The cannula, because it was not flexible, could only be extended into SC a limited distance and thus could only dilate a limited portion of the canal on either side of the dissection site. The injection of OVD caused an increase in SC dimensions leading to micro-ruptures in the inner wall of the canal, as well as adjacent TM. This created a direct connection between the anterior chamber and the lumen of the canal. The scleral flaps created to uncover SC were sutured watertight to avoid formation of a filtering bleb. Compared to trabeculectomy, viscocanalostomy proved to be a very safe procedure with fewer complications but its IOP lowering was inferior.[2] Its long term efficacy was disappointing presumably due to eventual re-collapse of SC in the postoperative period. [3] Canaloplasty has the advantage of being able to dilate SC along its entire length utilizing a flexible microcatheter.[4] It also has the advantage of using a permanent tensioning suture remaining in SC to maintain its dilation over time. Koerber reported a comparison of canaloplasty performed in one eye compared with viscocanalostomy in the contralateral eye. The viscocanalostomy eyes had a postoperative IOP of 16.1 +/- 3.9 on 0.4 +/- 0.5 medications with 35.7% complete success and 50% unqualified success. By contrast the canaloplasty eyes had an IOP of 14.5 +/- 2.6 on 0.3 +/- 0.5 medications with 60% complete success and 86.7% qualified success. [5]
Canaloplasty has several advantages over trabeculectomy. Under most circumstances, as long as goniopuncture is not performed, there is no bleb so bleb related complications are avoided. Hypotony and all its related complications can also be avoided under most circumstances since aqueous is allowed to drain via the natural outflow system so IOP should not be able to fall below episcleral venous pressure. Postoperative care and follow up is also simpler and less rigorous and visual recovery is typically more rapid. However, canaloplasty is also a more technically challenging surgery than trabeculectomy and typically does not produce IOP quite as low. It also scars an area of conjunctiva that may increase the risk of trabeculectomy failure in the future if it should be needed.
Indications and Contraindications
Indications: Canaloplasty is generally for open angle glaucomas. It is especially good for young patients with a clear lens and is less likely to cause cataract progression. It should also be considered for high myopes who would be at high risk for hypotony with a trabeculectomy surgery. It would also be excellent in ahakic patients where vitreous may obstruct the sclerotomy or tube in traditional glaucoma filtration surgeries.
Some relative contraindications include congenital glaucomas, narrow angle, angle recession, and cases with elevated episcleral venous pressure. An absolute contraindication would be angle closure glaucoma.
Surgical Technique
Ab-Externo Canaloplasty
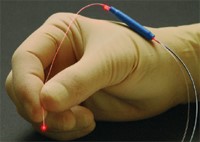
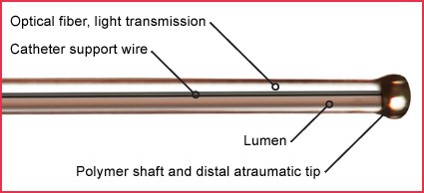
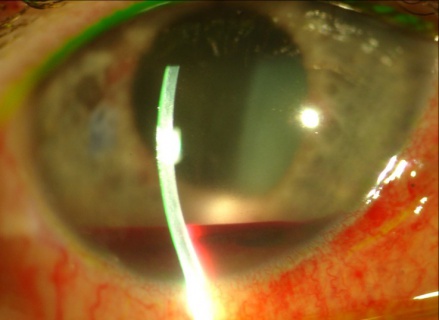
Canaloplasty requires the use of a 200 μm diameter flexible microcatheter with a blunt atraumatic 250 μm tip (iTrack, Nova Eye Medical Limited, Adelaide, Australia). Figure 5 This microcatheter has an internal lumen for injecting OVD. Figure 6 The OVD is injected via a screw driven syringe that allows for precise aliquots to be injected. Figure 7 The microcatheter also has an optical fiber to transmit light and is typically used with the battery powered iLumen Fiberoptic Illuminator (Nova Eye Medical Limited, Adelaide, Australia) which allows the tip of the microcatheter to glow red or blink to indicate its position within SC during the procedure.
- Canaloplasty can be performed with subconjunctival, sub-Tenon's, or retrobulbar anesthesia.
- A fornix based conjunctival peritomy is performed.
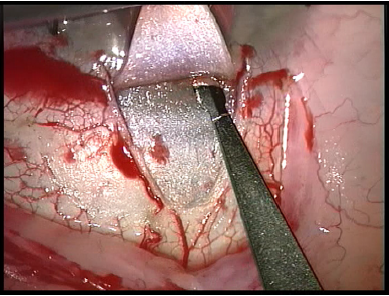
- A superficial scleral flap is created measuring about 5 mm by 5 mm.Figure 8
- A 4 mm by 4 mm deep scleral flap is then created within the borders of the superficial flap dissecting down to within 50 microns of the choroid. Figure 9 This dissection is carried forward into clear cornea. Schwalbe's line is carefully detached. Figure 10 The inner flap is then amputated and a large 500 micron trabeculo-descemetic window is created.
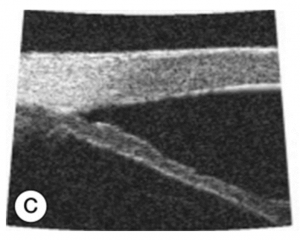
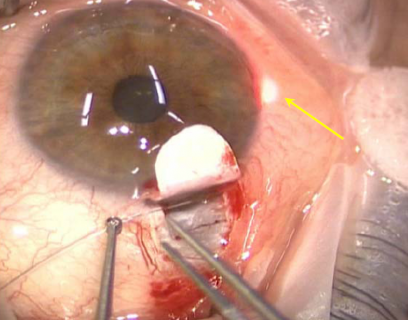
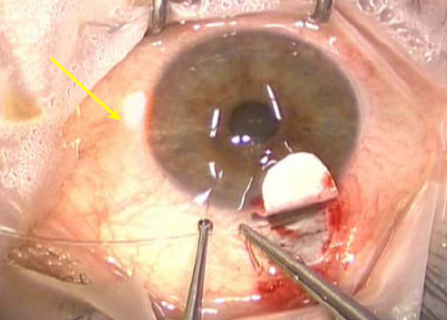
- SC is located and unroofed. A paracentesis is created. The microcatheter is advanced 360° around SC. The optical fiber that illuminates the tip of the microcatheter provides guidance to the path of the catheter as it is advanced. Figure 11
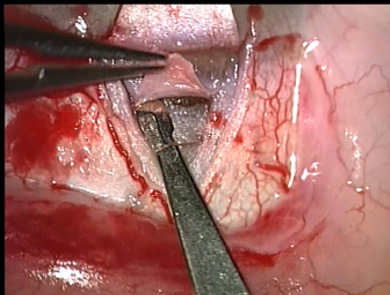
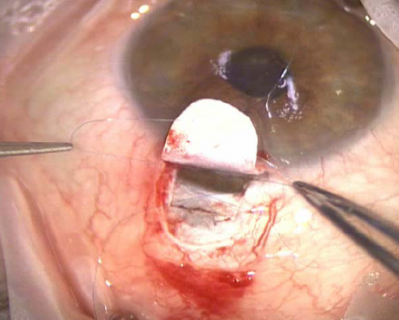
- When the distal tip of the catheter re-emerges at the surgical site, a 9-0 polypropylene (Prolene) suture is tied to it Figure 12 and the microcatheter withdrawn through the canal. Figure 13 Every 2 clock hours a precise aliquot of OVD is injected into SC via the screw driven injector. Care is taken to keep the catheter in perpetual motion through SC when OVD is injected to prevent the creation of a Descemet detachment. The microcatheter pulls the Prolene suture around the canal after it.
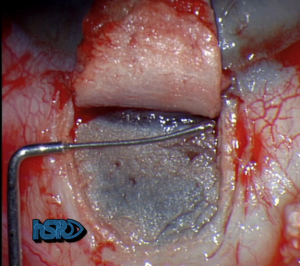
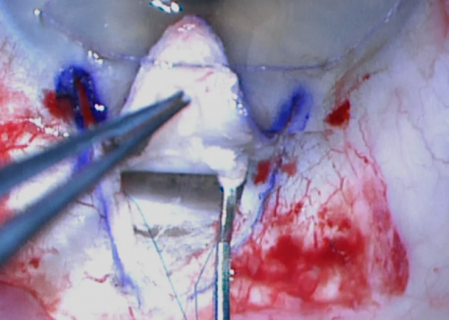
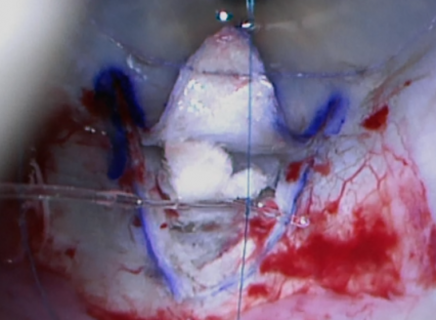
- When the microcatheter has completely cleared the canal, the Prolene suture is detached from the catheter. The suture is then and tightened to apply a long-term, moderate tension to the tissues of the inner wall of Schlemm’s canal. Figure 14 Some surgeons may elect to secure a spacer graft in the space within the scleral flap as is done in deep sclerectomy to allow an intra-scleral lake of aqueous to form.
- The scleral flap is then tightly closed with 10-0 nylon suture if a bleb formation is not desired. Alternatively, the flap can be left loose to allow gentle subconjunctival filtration as in deep sclerectomy.
- The conjunctiva is then closed.[6]
Ab Interno Canaloplasty
More recently, Ab interno approaches to Schlemm's canal that spare conjunctival and scleral incisions have gained favor, including many of the available Microinvasive Glaucoma Surgeries (MIGS).
The ab-interno technique involves creation of at least two clear corneal incisions and creation of a limited goniotomy. After creation of the goniotomy, the iTrack catheter (Nova Eye Medical Limited, Adelaide Australia) is thread through the goniotomy site for up to 360 degrees ab-intrno. The surgeon may visualize the illuminated tip while threading to ensure accurate placement of the device within Schlemm's canal. After threading, the surgeons slowly withdraws the external segment of the cathether in order to "back out" of Schlemm's canal while the surgical assistant injects viscoleastic through the catheter tip in order to dilate and distend Schlemm's canal and collector channel orifices.[7]
Ab interno Canaloplasty has demonstrated effective IOP lowering in the course of short-term follow-up.[8] Similarly, an ab interno 360-degree trabeculotomy, gonioscopy-assisted transluminal trabeculotomy (GATT), shows promising early results in terms of both IOP control and safety profile.[9]
Canaloplasty can also be performed without the use of a catheter using a 6.0 prolene suture, particularly if cost conscious or resource limited. [10]
More recently, the OMNI device has been shown as an effective alternative to the standard ABiC or GATT.[11] For more information about ab interno trabeculotomy such as GATT or OMNI, please visit the Ab Interno Trabeculectomy and Trabeculotomy page.
Postoperative Care
Antibiotics are typically given for one week and topical corticosteroids are used and tapered over 4 weeks. At one month postoperatively, if the IOP is not at target a YAG laser goniopuncture or bleb needling can be performed to convert the procedure into a full thickness filtration surgery (for ab-externo cases).
Outcomes
Lewis and colleagues reported the 3 year results of a multicenter trial of 157 eyes that received ab-externo canaloplasty. Preop IOP was 23.8 +/- 5 on 1.8 +/- 0.9 medications. The overall postoperative IOP at 3 years was 15.2 +/- 3.5 on 0.8 +/- 0.9 medications, representing a 36.1% reduction in IOP. There was a subset of 36 eyes that received cataract surgery concomitantly with canaloplasty had significantly better results with an IOP of 13.6 +/- 3.6 (a 42% reduction) on 0.3 +/- 0.5 medications. [12]
Canaloplasty is thought to be safer than trabeculectomy but it is also generally considered to be inferior in terms of efficacy in IOP lowering. Tam and colleauges challenged this notion, showing that in certain circmstances canaloplasty can perform quite comparably to trabeculectomy. In their retrospective comparison of 101 eyes, 50 receiving canaloplasty and 51 receiving trabeculectomy they reported equal result in IOP and medication use. The canaloplasty cohort went from preop IOP 26.4 +/- 6.5 on 3.6 +/- 0.9 medications to postop IOP 13.4 +/- 2.7 on 0.6 +/- 1.1 medications. The trabeculectomy cohort went from preop IOP 26.8 +/- 8.1 on 3.6 +/- 1.1 medications to postop IOP 12.3 +/- 3.5 on 0.7 +/- 1.3 medications. [13]
Surgical outcomes with the ab-interno technique were reported by Gallardo in 2021.[14] In this retrospective, comparative, and consecutive case series of 53 patients that underwent iTrack canaloplasty as standalone procedure or in combination with cataract surgery, intraocular pressure was reduced from 20+4.9 mmHg at baseline to 13.6+1.9 mmHg after 24-months of follow-up. respectively (P<0.001). This translated to significant reduction in topical medication usage in both the standalone and combined treatment groups. With this ab-interno technique, there were no serious adverse events or complications.
Effects on Corneal Endothelial Cell Health
It is important to consider potential adverse effects on corneal endothelial cell health with any intraocular surgical procedure. The stability of corneal endothelial cell density one year after ab-interno canaloplasty combined with cataract surgery was reported in 2021.[15] In a prospective trial of 77 eyes of 46 patients, specular microscopy was performed preoperatively and at 6 and 12 months postoperatively. Endothelial cell density was analyzed at each time point. One-year endothelial cell density results were compared with historical controls in eyes that underwent cataract surgery alone. After one year, mean endothelial cell density loss was 80 cells/mm2 in eyes treated with ab-interno canaloplasty in combination with cataract surgery and overall cell density did not differ from preoperative range (P=0.21). This translated to 3.2% reduction in endothelial cell density, which was numerically lower than historical controls that underwent cataract surgery alone in FDA pivotal trials for other MIGS devices. Future studies are planned to analyze results out to five years of follow-up.
Complications
Intraoperative Complications
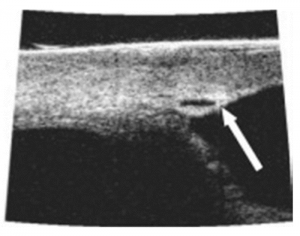
If the deep scleral flap is dissected too deep (using the ab-externo technique) the trabeculo-descemetic window can be perforated. Figure 15 If this occurs a sclerotomy can be created with an iridectomy and the procedure can be converted to a trabeculectomy.
Postoperative Complications
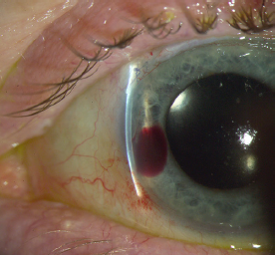
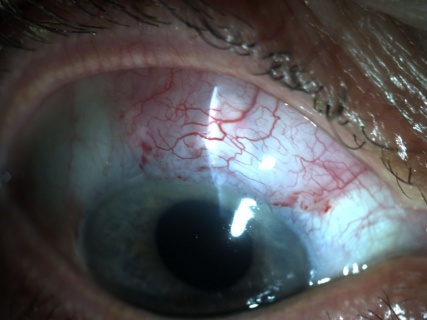
Lewis' study reported only 16 adverse events in 12 eyes using the ab-externo technique. Mild hyphema is common and was seen in 10.2% of eyes and all except in 3 eyes were resolved by 1 month. Figure 16 A Descemet detachment with intrastromal corneal blood was seen in 3.2% of eyes. Figure 17 3 eyes had persistent IOP elevated > 30 within the first 90 days. 2 were converted to trabeculectomies and 1 underwent YAG goniopucture. Figure 18A and Figure 18B 7 eyes had increased IOP in the late postoperative course of which 5 required procedures including goniopuncture, iridoplasty, cyclophotocoagulation, and a trabeculectomy. There was only a 0.6% rate of early hypotony but there were no flat anterior chamber, choroidal detachment, or endophthalmitis reported.[12]
References
- ↑ Stegmann R, Pienaar A, Miller D. Viscocanalostomy for open-angle glaucoma in black African patients. J Cataract Refract Surg. 1999;25:316Y322.
- ↑ Yalvac IC, Sahin M, Eksioglu U, et al. Primary viscocanalostomy versus trabeculectomy for primary open-angle glaucoma: three-year prospective randomized clinical trial. J Cataract Refract Surg. 2004;30:2050-2057.
- ↑ Sunaric-Megevand G, Leuenberger PM. Results of viscocanalostomy for primary open-angle glaucoma. Am J Ophthalmol 2001 Aug;132(2):221-8
- ↑ Kearney JR, Ball SF, Field MW, et al. Circumferential viscodilation of Schlemm’s canal with a flexible microcannula during non-penetrating glaucoma surgery. DJO.
- ↑ Koerber NJ. Canaloplasty in one eye compared with viscocanalostomy in the contralateral eye in patients with bilateral open angle glaucoma. J Glaucoma. 2012;21:129-134.
- ↑ Koerber, NJ. Canaloplasty New Approach to Nonpenetrating Glaucoma Surgery. Techniques in Ophthalmology 5(3):102–106, 2007.
- ↑ https://www.healio.com/news/ophthalmology/20210727/itrack-microcatheter-system-offers-efficacy-versatility-in-glaucoma-surgical-space
- ↑ Davids AM, Pahlitzsch M, Boeker A, et al. Ab interno canaloplasty (ABiC)-12-month results of a new minimally invasive glaucoma surgery (MIGS). Graefes Arch Clin Exp Ophthalmol 2019;Epub ahead of print.
- ↑ Grover DS, Godfrey DG, Smith O, et al. Gonioscopy-assisted transluminal trabeculotomy, ab interno trabeculotomy: technique report and preliminary results. Ophthalmology 2014;121:855-61.
- ↑ Aktas Z, Ucgul AY, Bektas C, et al. Surgical outcomes of prolene gonioscopy-assisted transluminal trabeculotomy in patients with moderate to advanced open-angle glaucoma. J Glaucoma 2019;28:884-8.
- ↑ Hirsch L, Cotliar J, Vold S, et al. Canaloplasty and trabeculectomy ab interno with the OMNI system combined with cataract surgery in open-angle glaucoma: 12-month outcomes from the ROMEO study. J Cataract Refract Sure 2021;47:907-15.
- ↑ Jump up to: 12.0 12.1 Lewis RA, von Wolff K, Tetz M, et al. Canaloplasty: Three year results of circumferential viscodilation and tensioning of Schlemm’s canal using a microcatheter to treat of open-angle glaucoma J Cataract Refract Surg. 2011;37:682-690.
- ↑ Tam DY, Calafati J, Ahmed I. Non-penetrating Schlemm’s Canaloplasty vs Trabeculectomy. Presented at the American Glaucoma Society meeting, Naples, FL, March, 2010.
- ↑ Gallardo MJ. Clinical Ophthalmology 2021:15;1591-1599.
- ↑ Lubeck DM, Noecker RJ. One year evaluation of endothelial cell density and loss following iTrack ab-interno canal based surgery. Presented as a scientific poster at The 2021 American Society of Cataract and Refractive Surgery Annual meeting.