All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Canalicular trauma refers to sudden physical injury that results in damage to the canaliculus, part of the lacrimal drainage system of the eye. The lacrimal canaliculi are located within the medial aspect of the eyelid. This area area is unlike the rest of the eyelid because it does not contain a tarsal substructure. Therefore, a force which displaces the eyelid from its strong attachment at the medial canthal tendon, lacrimal, and maxillary bone, tend to cause avulsion in the medial aspect of the eyelid. Many types of trauma to the face may result in damage to the lacrimal drainage system. Dog bites are a common cause of canalicular lacerations because of the propensity of this type of injury to occur near the medial canthus as are blunt shear injuries.[1] Canalicular trauma is best evaluated by a physician experienced in the repair of canalicular lacerations. Members of the American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS) are qualified to perform even complex repair of the lacrimal drainage system.
Disease Entity
Canalicular trauma is recognized by the following codes as per the World Health Organization's (WHO) International Classification of Diseases (ICD) nomenclature:
ICD-9-CM
870.2 Laceration involving lacrimal passages
ICD-10-CM
S01.111A Laceration without foreign body of right eyelid and periocular area, initial encounter
S01.111D Laceration without foreign body of right eyelid and periocular area, subsequent encounter
S01.111S Laceration without foreign body of right eyelid and periocular area, sequela
S01.112A Laceration without foreign body of left eyelid and periocular area, initial encounter
S01.112D Laceration without foreign body of left eyelid and periocular area, subsequent encounter
S01.112S Laceration without foreign body of left eyelid and periocular area, sequela
S01.119A Laceration without foreign body of unspecified eyelid and periocular area, initial encounter
S01.119D Laceration without foreign body of unspecified eyelid and periocular area, initial encounter
S01.119S Laceration without foreign body of unspecified eyelid and periocular area, sequela
*Laceration with foreign body of an eyelid follows the above formatting with the prefix S01.12 instead of S01.11
Anatomy
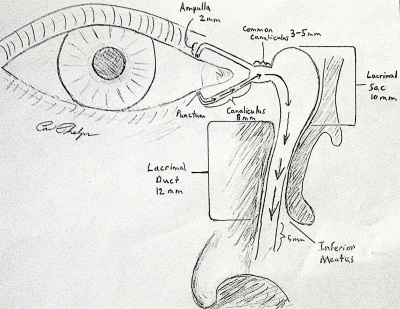
The canaliculus is located in the medial portion of each of the four eyelids. In most patients, the punctum of the eyelid sits against the conjunctiva in the tear lake, approximately 6.5 mm from the medial commissure in the upper eyelid and 6.0 mm from the medial commissure in the lower eyelid. The punctum wicks up tears into the ampulla, which is approximately 2 mm long and perpendicular to the eyelid margin. While some of the tear drainage is passive, there is also an active pumping mechanism through blinking which creates negative pressure in the system and thus draws tears into the drain. There is an elevated junction between the luminal surface of the punctum and beginning of the vertical canaliculus, which at this time is of uncertain physiologic significance.[2] The lacrimal drainage system then makes a 90 degree turn and becomes the canaliculus (which is parallel to the eyelid margin). (Fig. 1) This pathway is approximately 8 mm between the ampulla and the common canaliculus. The common canaliculus (or common opening into the lacrimal sac) is present in 98% of patients.[3] The common canaliculus is 3 to 5 mm long and inserts onto the lateral wall of the lacrimal sac. In the 2% of patients without a common canaliculus, the canaliculi from the upper and lower eyelids separately insert into the lacrimal sac. The lacrimal sac is bounded by the anterior lacrimal crest (maxillary bone) and the posterior lacrimal crest (lacrimal bone). The anterior ramus of the medial canthal tendon inserts on the maxillary bone while the posterior ramus inserts on the lacrimal bone.[4] Medial canthus anatomy is complex and involves several support structures in addition to the canthal tendons and lacrimal drainage system.[5] Damage to the facial bones and other more significant trauma to the eye and ocular adnexa is beyond the scope of this article.
Pathogenesis
An injury to the lacrimal drainage system can lead to scarring and stenosis, which in turn may cause epiphora (a condition in which tears run down over the eyelid margin and onto the cheek). Canalicular trauma may be caused by direct or indirect injury to the canaliculus. Direct injury may be caused by penetrating trauma with foreign objects such as glass, metal, or organic material. A dog bite injury may also result in direct damage to the canaliculus and, in fact, are more likely to result in canalicular injury (35.6%) than in eyelid lacerations from other causes (3.6%).[1] Indirect injury is more likely to occur with a fist punch to the face, finger poke, or diffuse injury from an impact such as may occur in a motor vehicle accident or a fall.
One of the first studies of the pathogenesis of canalicular lacerations retrospectively reviewed 25 patients with canalicular trauma, and demonstrated that 84% of of them had diffuse trauma or trauma remote from the eyelids, while only 16% had direct injury to the canaliculus.[6] The authors postulated that canalicular lacerations are often attributable to stretching of the eyelid to the point of avulsion. A more recent retrospective study, which included 236 patients, found that approximately 55% of patients with canalicular lacerations had direct penetrating injuries.[7] The authors further noted that patients with indirect injuries tended to have more extensive injuries such as orbital wall fractures, ruptured globe, and other bodily injury. One extensive review of canalicular lacerations noted that, of 281 cases, 202 (71.9%) involved an isolated inferior canaliculus, while only 44 (15.7%) involved an isolated superior canaliculus. In 35 cases (12.4%), there were lacerations of both the superior and inferior canaliculi and/or the common canaliculus.[8] Damage to the lacrimal drainage system may lead to stenosis and epiphora.
Risk Factors
- Age - most injuries occur in children or young adults.[9]
- The eyelids are involved in approximately 20% of all facial lacerations in pediatric patients.[10]
- Patients under 4 years of age are more susceptible to facial dog bite injury.
- Trauma tends to occur more frequently in young adults.
- Middle aged patients are the least likely to be affected by canalicular trauma.
- Elderly patients are more prone to falls, which may result in canalicular injury.
- The eyelids are involved in approximately 20% of all facial lacerations in pediatric patients.[10]
- Sex - males are more often affected by canalicular trauma than females.[11]
- Boys are more likely to experience facial dog bite injuries than girls.
- Young men engage in more physical altercations than young women.
- Environmental - exposure to various activities, animals, or objects may increase risk of canalicular trauma.
- Fist fighting
- This is the most common cause of canalicular trauma.
- May be direct injury to the eyelids or indirect contusion of the cheek causing canalicular avulsion.
- Dogs
- The Pit Bull Terrier breed has been shown to be a disproportionately frequent perpetrator of canalicular trauma.[12]
- Hooks
- Intoxicants
- Impaired persons are often the perpetrator of physical violence and/or motor vehicle accidents.
- Other
- Fist fighting
The risk factors for canalicular trauma overall mirror the overall risk factors for trauma. Children and young adults are more likely to experience canalicular trauma than middle aged and elderly. The most common cause of canalicular injury is blows from fists. One case series of 222 patients who presented to Wills Eye Hospital with canalicular lacerations, showed that blows from fists were the cause of 23.4% of canalicular lacerations.[18] Young children are more likely to experience facial dog bites that result in ocular injury. One study found that 45.2% of children with dog bites had ocular injury vs. 10.8% of adults.[19] The authors found that Pit Bulls were the most common breed of dog which inflicted ocular injury (25%), which agreed with the results of an earlier study which also pointed to the association with childhood canalicular lacerations and Pit Bull Terrier attacks.[12] Young adults are more likely to be involved in physical confrontations, which are another common cause of canalicular lacerations. Many times a punch to the face or a contusion from a fall causes indirect injury with canalicular avulsion. Direct penetrating injury with a knife, glass, or stick may also cause canalicular laceration. Glass tends to cut deeper than may be fully appreciated on initial examination. Elderly patients are at higher risk of falls, which may also result in blunt trauma (falling onto coffee table or stairs, for example) and canalicular trauma.
Diagnosis
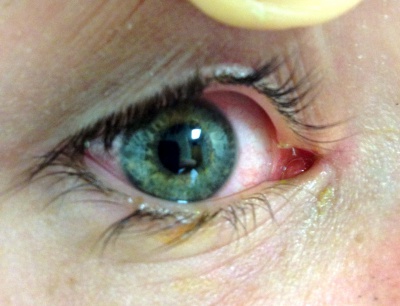
Canalicular lacerations are identified by direct observation of a laceration medial to the punctum or by probing (usually with a Bowman probe or irrigation cannula) of the canalicular system. Canalicular laceration may not be obvious on presentation, but should always be suspected in cases from dog bites or with medial eyelid injury. (Fig. 2) In young children, an examination under anesthesia with dilation and probing may be necessary to make the diagnosis. Severe medial laceration with lateral displacement of the medial canthus alerts the physician to obvious underlying lacrimal system damage. (Fig. 3) The proximal end of the laceration is easily identifiable with the use of a Bowman probe, (Fig. 4) but the distal/nasal portion of the canaliculus is often more difficult to identify. The surgeon begins by cleaning the wound and looking for white circular tissue within the pink area of orbicularis muscle. If this is not identified easily, fluorescein or air may be injected via a 27 gauge cannula into the opposite punctum. The surgeon may then observe dye appearance or bubbles (when the nasal canaliculus of interest is submerged) emanating from the nasal portion of the canaliculus.[20]
History
Any history of upper facial trauma (brow, nose, cheek) may raise suspicion of a possible canalicular laceration. An accurate history is very important to determine the likelihood of deeper laceration (especially with glass injuries), retained foreign bodies, and wound contamination. The possibility of retained organic or other foreign bodies may prompt imaging studies such as a CT scan of the orbits. The patient's tetanus immunization history and history of any allergies to medications may be inquired about prior to beginning any surgical intervention. It is also important to determine if the trauma was caused by an animal bite. Large studies have shown that dog bites to the face have a high incidence of eyelid and canalicular lacerations, particularly in the pediatric population. Rarely, a patient may have had a history of prior ocular or naso-lacrimal surgery, and this is best known before proceeding to surgery.
Physical exam
Examination for canalicular trauma is best preceded by consideration of the patient's overall condition, including ruling out the possibility of life or eye threatening injuries. Once the patient is deemed to be in stable condition and the globe is found to be intact (or has been repaired), the physician may focus on damage to the patient's eyelid and possible canalicular trauma. Canalicular lacerations are identified by direct observation of a laceration medial to the punctum, or by dilation and probing (usually with a Bowman probe) of the canalicular system. As there can be medial canthal tendon avulsion as well, care should be taken to determine this prior to repair or deep probing.
Diagnostic imaging
Canalicular trauma may range from minor to severe, and any clinical suspicion of possible ruptured globe, retained foreign body, or facial fractures may prompt preoperative imaging. One retrospective review of 1,201 children with dog bite injuries to the face demonstrated that seventeen (1.4%) of those patients also sustained facial fractures. Facial bones are ideally imaged with a CT scan. Concern for orbital fractures may prompt a CT-orbit (which gives a more detailed view of the orbital bones). If a foreign body is suspected, CT is also the study of choice because any retained ferromagnetic material is a contraindication to MRI. A MRI also generally also takes longer to obtain and is usually not needed in cases of canalicular trauma. Contrast agents are not helpful in identifying fractures on a CT scan. It is important to identify these fractures because they may require complex surgical repair that is ideally undertaken prior to addressing canalicular trauma.
Management
Prompt evaluation of the globe and adnexal structures is required when trauma to the ocular region is suspected. A ruptured globe is an ophthalmologic emergency and is best treated urgently and prior to eyelid surgery. Patients canalicular lacerations are best evaluated and treated by an experienced professional, usually an ophthalmic plastic and reconstructive surgeon. It is important for the eyelid margin and canaliculus to be repaired so that the eyelid anatomy can be restored and eyelid pump and drainage physiology can return to normal. Repair of the canaliculus lessens the risk of the patient developing epiphora (tearing which rolls down the cheek) and also contributes to obtaining good eyelid position post-operatively.
The nasal (or proximal) cut end of the canalicular laceration may be difficult to identify, and various methods have been developed to help rapidly locate it.[21] The first approach is often to use a Bowman lacrimal probe. By following the natural course of the eyelid and canalicular system, the probe often points toward the nasal portion of the canaliculus. Looking carefully (with loupes or surgical microscope, if necessary) will often allow the surgeon to identify the whitish circular opening of the canaliculus and/or lacrimal sac. It may be useful to inject fluorescein impregnated saline or air into the opposite punctum and simultaneously observe dye appearance or bubbles (when the nasal canaliculus of interest is submerged) to identify the nasal portion of the canaliculus. For the majority of patients with a common canaliculus and single canalicular injury, a pigtail probe can also be helpful. [22]The use of viscoelastic injection has also been described as a useful technique.[23] Topical phenylephrine to the area of injury will cause constriction of the vascular and muscular tissues surrounding the canaliculus, and has also been reported as a useful technique help identify the lacerated lacrimal drainage system.[24]
Immediate surgical intervention is not required in cases of canalicular trauma.[25] A retrospective review of patients undergoing monocanalicular repair at Moorfields Eye Hospital demonstrated that delayed surgery (up to ~72 hours) did not negatively affect outcomes.[26] Another study demonstrated successful repair after as long as 5 days following injury.[27] Monocanalicular canalicular laceration may or may not lead to eventual stenosis and epiphora if it is not repaired. In a study of consultant ophthalmologists in the UK, only 40% would always repair a monocanalicular injury.[28] An experimental model of monocanalicular obstruction demonstrated that only approximately 10% of patients demonstrate severe impairment in drainage outflow when one canaliculus is blocked.[29] It follows that most patients with injury to a single canaliculus will not develop epiphora. Also, older patients are more likely to have dry eye, and therefore may be less affected by the loss of canalicular drainage from one arm of the lacrimal drainage system. If both superior and inferior canalicular lacerations are present, surgical repair of both canaliculi is always indicated,[30] and it is advisable for even a monocanalicular injury to be repaired as soon as feasible.[31] However, even with appropriate and prompt surgical management, some patients will still develop canalicular obstruction, stenosis, and impaired lacrimal outflow, requiring additional revision surgery.
Medical
Patients with canalicular trauma who have not had a tetanus vaccination within the past 10 years are best treated with a tetanus booster (tetanus toxoid 0.5 mL IM) in the emergency department.[32] Rabies may also be considered in any patient who has been exposed to an animal bite. Routine antibiotic coverage for canalicular trauma post-operative infection prophylaxis is controversial. The ocular adnexal tissues and face has an excellent blood supply and tends to have a lower infection rate than elsewhere in the body. However, prophylaxis is generally recommended in all bites that penetrate the skin.[33] The majority of bites wounds are polymicrobial with a mix of aerobic and anaerobic organisms which represent oral flora of the offending animal. Pasteurella canis (~50%) is most common among dog bites and Pasteurella multocida (~50%) is most common in cat bites.[33] Capnocytophaga canimorsus is a commensal organism in the normal flora of cats and dogs. High-risk patient populations are predisposed to contract severe infection, such as meningitis, with C. canimorsus exposure. [34] Elderly patients, immunocompromised (including patients on steroids and other immunomodulators), alcoholics, patients with β-Thalassemia, and smokers are especially at high-risk of developing severe illness following dog or cat bite. Augmentin (amoxicillin/clavulanate) for 3-5 days is the first line of treatment because it covers a broad range of organisms that may be involved.
Surgical
There are several varieties of lacrimal stents and surgical approaches which successfully repair canalicular lacerations and avulsions. The instruments and surgical techniques utilized may be chosen based on a case-by-case basis so that they are catered to the individual patient.[35][36] The Mini Monoka monocanalicular stent (FCI Ophthalmics) has become a popular method to repair simple monocanalicular lacerations.[37] [38]Bicanalicular lacerations may be repaired using two Mini Monoka stents, or a bicanalicular stent. The Crawford and Ritleng are two of the most popular bicanalicular stents.
Many cases of canalicular repair can be accomplished in the emergency department or at the bedside without the use of general anesthesia, intravenous sedation or field blocks with those experienced in repair. Children may require sedation, but this is also achievable in the emergency department with the use of ketamine and monitored anesthesia. More severe trauma or otherwise challenging patient care scenarios may require the assistance of intravenous sedation or general anesthesia in the operating room. Additionally, more complicated cases may warrant the use of surgical loupes or an operating microscope. Some surgeons also choose to use loupes or assistance of an operating microscope due to personal preference. Experience of the surgeon and patient selection are important factors in determining the setting for the repair and type of anesthesia.[39]
| Instruments | Medications | Sutures | Implants |
|---|---|---|---|
| Needle driver | Alcohol prep pads | 5-0 polyglactin (Vicryl) on P-2 needle | Mini Monoka canalicular stent |
| Westcott scissors | Povidone-iodine (Betadine) | 6-0 fast-absorbing gut | Optional: |
| Small (0.3-mm) toothed forceps | Tetracaine 0.5% | Optional: | Crawford bicanalicular stent |
| Bowman probe (0-00) | 2% lidocaine with epinephrine 1:100,000 | 4-0 to 6-0 silk, for margin repair | Ritleng bicanalicular stent |
| Lacrimal dilator | Erythromycin ophthalmic ointment | ||
| 3 mL syringe | |||
| Large gauge needle (18-22) to draw up anesthetics | |||
| Small gauge needle (27-30) to inject local anesthetics | |||
| Optional: | |||
| Lacrimal cannula (23-27 gauge) | |||
| Pigtail probe |
Traditional Surgical Repair
The earliest methods of canalicular laceration repair described the use of malleable rods to assist in repair.[40] Several subsequent methods were developed,[41][42][43][44] but the one which found favor for several decades was the pigtail probe.[45][46] This instrument was used to intubate both canaliculi and would be inserted first into the uninvolved canaliculus and rotated until the end of the probe was visualized in the nasal end of the torn canaliculus. A silicone stent was then inserted which connects the two canaliculi. An example of this technique for pediatric canalicular repair using the pigtail probe can be seen on the American Academy of Ophthalmology's One Network website. There are still some circumstances, for example when the severed deep ends of the laceration are difficult to identify, when a pigtail-type may still be a useful instrument.[47] However, the pigtail probe method has been largely abandoned due to its poor long-range effectiveness.[48] One significant weakness of the pigtail probe method is the risk of damaging the uninvolved canaliculus, which may lead to postoperative epiphora in patients who may not have experienced this complication without any surgical intervention. Also, it may not be known prior to surgery whether the patient has a common canaliculus or separate canalicular entrances to the lacrimal sac. If there is no common canaliculus, a false passage may be created with the blind insertion of a pigtail probe. Earlier pigtail probes also had a barb on the end which was used to attach suture material which caused canalicular trauma. So, while it still may be occasionally useful, the pigtail probe is important mainly due to its historical interest.
Many surgeons have advocated direct anastomosis the lacerated ends of the canaliculus.[30] [36][49][50] This technique utilized two or three 8-0 polyglactin sutures to create the anastomosis and was combined with bicanalicular intubation.[30] A similar technique involves the use of 7-0 polyglactin suture material with two or three sutures to create a canalicular anastomosis.[36] A limiting factor of the surgical approach of creating a direct anastomosis of the canaliculus is that it may be difficult to perform the procedure without the use of an operating microscope or surgical loupes. Another technique, the "one-stitch" canalicular anastomosis (in which a silk suture is passed through both the skin and the canaliculus) was effective in one study.[49] The surgeons in that study utilized 5-0 silk sutures that they removed one week after the operation. However, most surgeons have found that direct anastomosis of the canaliculus is not needed for successful outcomes. This is due to the fact that the lacerated ends of the canaliculus naturally come into apposition when a stent is inserted into the canaliculus and the proximal tissues are sutured together. A high success rate has been reported with a simplified approach to repair of canalicular laceration in which a single 7-0 polyglactin horizontal mattress suture anterior to the canaliculus was placed.[51] The authors reviewed 67 patients who had undergone their method for repair and reported only 4% with postoperative symptomatic epiphora and 13% with some delay in outflow with dye disappearance testing.
The two techniques outlined above are not generally utilized in routine canalicular laceration repair. Also, bicanalicular intubation with insertion of the silicone stent through the lacrimal duct and into the nose is not usually required for simple canalicular lacerations. Insertion of a probe into the nose necessitates the assistance of an anesthetist (either intravenous sedation with monitored anesthesia care or general anesthesia) because patients find intubation of the nasolacrimal duct and retrieval of the probes from the nasal cavity intolerable. The advent of monocanalicular intubation with a silicone stent and a method for fixation to the punctum without a suture was a major advance in the treatment of canalicular lacerations.[52] Surgeons may perform a canalicular laceration repair at the bedside or in the emergency department without the need for anesthesia assistance or an operating microscope. Monocanalicular intubation is effective and the most common method of treatment for canalicular laceration today.
Monocanalicular Repair
Mini Monoka
Step 1) Give the patient a drop of tetracaine (or other topical anesthetic) to achieve conjunctival and ocular surface anesthesia.
Step 2) Clean the wound and surrounding area with an alcohol prep pad
Step 3) Inject 1 or 2% lidocaine with epinephrine (1:100,000) for anesthesia and hemostatic effect.
Step 4) With the patient comfortable (unable to sense sharp pain), irrigate the wound with saline and remove any particulate or foreign body material. The laceration may be irrigated with normal saline solution or saline with 50,000 units of bacitracin per liter.
Step 5) Prep and drape the patient in a standard sterile fashion, using 5% povidone-iodine and a sterile drape.
Step 6) Use a punctal dilator to enlarge the punctum so that the silicone stent can be subsequently passed through the canalicular system. (Fig. 5) The nasal portion of the canaliculus may be identified by directly observing a circular and pale appearing canalicular passage, or injecting the opposite punctum with air (with the canaliculus of interest being submerged under saline or other clear liquid) or fluorescein and observing the bubbling effect or fluorescein efflux from the nasal portion of the lacerated canaliculus.
Step 7) Cut a Mini Monoka stent to approximately 10 mm, with a beveled edge. Insert the stent into the punctum and follow the canaliculus. Retrieve the stent from the proximal end of the canaliculus and pull the stent so that the collar is seated flush with the punctal ampulla (this may require pushing with a second forcep to seat the collar). (Fig. 6)
Step 8) Introduce the distal portion of the stent into the nasal portion of the lacerated canaliculus. Identifying the nasal portion of the lacerated canaliculus is often the most difficult part of the surgery. See the "Physical Exam" section above for specialized techniques used to identify the nasal portion of the canaliculus.
Step 9) Suture the stent into place by using a 5-0 polyglactin suture on a P-2 (1/2 circle, 8.0 mm) needle to make a buried horizontal mattress suture within the peri-canalicular proximal and distal lacerated orbicularis muscle. (Fig. 7) The P-2 needle is convenient to approach the tight surgical space of the medial canthus. Other types of absorbable suture may be used for this step, 7-0 polyglactin has been advocated by some surgeons.[51]
Step 10) Close the eyelid margin using 6-0 fast absorbing gut sutures. Place one suture in the gray line, with approximately 1 mm on each side of the laceration. Cut the suture ends to approximately 5 mm each. A 6-0 fast absorbing gut suture may then be placed second near the cilia of the eyelid. This suture can be tied using a 2-1-1 knot, and after the first throw (2 turns) is placed, lay the suture from the gray line across the lash suture and tie it down with the 1-1 throws. Alternative, 6-0 silk or larger sutures (some advocate 4-0 silk at the eyelid margin) may be placed at the eyelid margin. However, silk sutures will need to be removed 10-14 days after surgical repair.
Step 11) Use 6-0 fast absorbing gut sutures to close the skin.
Step 12) Clean the patient and place antibiotic ointment (Erythromycin or Bacitracin ophthalmic is preferred) on the wound. Dressing the wound is left to the surgeon's discretion. (Fig. 8)
The patient may wear an eye shield, especially at night, in order to protect the recently repaired canalicular laceration.
Bicanalicular Repair
Crawford Stent
Step 1) See step 1-6 from monocanalicular repair above.
Step 2) The olive-tipped metallic guide of the Crawford Bicanalicular Intubation set is introduced into the punctum and advanced for 2 mm (or just inside the ampulla). Then make a 90 degree turn and follow the canaliculus for approximately 8 mm (or up to the distal end of the lacerated canaliculus).
Step 3) The guide wire is then passed through the nasal end of the lacerated canaliculus. This is often the most difficult portion of the surgery because of the challenge of identifying the the nasal portion of the lacerated canaliculus among the traumatized tissues. Techniques above under the heading of "Physical Exam" may be useful if you are having difficulty. The tip of the metallic guide will then make a hard stop at the lacrimal sac fossa.
Step 4) At this point, the metallic guide of the Crawford stent is rotated to follow the direction of the lacrimal duct through the maxillary bone. The direction of the wire guide is generally posterior and lateral from the position of the lacrimal sac fossa (toward the nostril).
Step 5) The olive tip of the Crawford tube can be retrieved from the nose with a Crawford hook.
Step 6) Steps 2-5 above are repeated for the opposite canaliculus.
Step 7) The silicone tubes are tied inside the nose with a square knot or three half throws, taking care to leave enough slack in the loop so that no tension is placed on the puntae. Ideally, the knot is just below the inferior turbinate in the anterior nasal vestibule so that no tubing is visible outside the nose. The silicone is then cut below the knot.
Step 8) The knot may be sutured inside the lateral nare with a 5-0 prolene suture. This may be done to prevent the tubing to inadvertently get pulled out of the punctae, and the suture is ideally placed at the junction of keratinized skin and nasal mucosa.
Step 9) See steps 9-12 from monocanalicular repair above.
Ritleng Stent
Step 1) See step 1-6 from monocanalicular repair above.
Step 2) A Ritleng inserter is introduced into the punctum and advanced for 2 mm (or just inside the ampulla). Then make a 90 degree turn and follow the canaliculus for approximately 8 mm (or up to the distal end of the lacerated canaliculus).
Step 3) The Ritleng inserter is then passed through the nasal (proximal) end of the lacerated canaliculus. This is often the most difficult portion of the surgery because of the challenge of identifying the the nasal portion of the lacerated canaliculus among the traumatized tissues. Techniques above under the heading of "Physical Exam" may be useful if you are having difficulty. The tip of the metallic guide will then make a hard stop at the lacrimal sac fossa.
Step 4) At this point, the Ritleng inserter is rotated to follow the direction of the lacrimal duct through the maxillary bone. The direction of the wire guide is generally posterior and lateral from the position of the lacrimal sac fossa (toward the nostril).
Step 5) The prolene thread of the Ritleng stent is threaded into the inserter until it can be seen in the nasal cavity. It can then generally be removed under direct visualization with a hemostat or Ritleng hook. The Ritleng inserter is then backed out and the probe is separated from the tubing by sliding the narrow section of prolene thread through the slit on the probe.
Step 6) Steps 2-5 above are repeated for the opposite canaliculus.
Step 7) The silicone tubes are tied inside the nose with a square knot or three half throws, taking care to leave enough slack in the loop so that no tension is placed on the puntae. Ideally, the knot is just below the inferior turbinate in the anterior nasal vestibule so that no tubing is visible outside the nose. The silicone is then cut below the knot.
Step 8) The knot may be sutured inside the lateral nare with a 5-0 prolene suture. This may be done to prevent the tubing to inadvertently get pulled out of the punctae, and the suture is ideally placed at the junction of keratinized skin and nasal mucosa.
Step 9) See steps 9-12 from monocanalicular repair above.
Surgical follow up
Canalicular laceration repair is generally followed until complete healing has been observed. The patient is first seen one week after repair or as needed depending on the patient's condition. Any silk sutures placed at the eyelid margin may be removed approximately 10 to 14 days after surgical intervention. Patients may wear a protective eye shield when they sleep and are recommended to avoid rubbing the eyelid for two weeks following surgery. A monocanalicular silicone stent may be removed approximately 8-12 weeks following surgical repair. Silicone stents may be removed simply at the slit-lamp using a forceps to pull the collar of the stent from the punctum. Bicanalicular stents are often left in place for up to 3 months. A scissors and forceps are required to remove a bicanalicular stent. If a suture was placed in the nose, this should be cut. Then the bicanalicular stent may be cut near the eyelid margin and removed from the nose. If a single square not was placed in the silicone tube, it may be removed through the eyelid as well.
Some surgeons have advocated use of antibiotic prophylaxis after canalicular trauma, particularly with animal or human bites.[33][53] It is known that the highly vascular facial tissues tend to be less prone to infection than other areas of injury, and the use of antibiotics is determined on a case by case basis. Patients who have experienced a bite injury may benefit from treatment with augmentin (amoxicillin/clavulanate) for 3-5 days following the injury. This the first line of treatment because it covers a broad range of organisms that may be involved. See medical management above for more information regarding medical treatment in canalicular trauma.
Complications
The benefits of repairing canalicular lacerations far outweigh the alternative of not pursuing surgical repair. Pain, bleeding, infection, loss of vision (although very rare), scarring (or poor healing), and a need for more procedures are considered the most likely risks of any ophthalmic surgery. The complications of canalicular surgery are few, but include premature extrusion of the stent material (with subsequent obstruction of the canaliculus), cheese-wiring of silicone tubes at the level of the punctum, pyogenic granuloma, and epistaxis (nosebleed).[36] Poor healing or inadequate repair may result in corneal exposure or an eyelid notch. Failure of the canalicular laceration repair may also result in poor drainage of the naso-lacrimal duct. Upper eyelid lacerations may damage the levator muscle and/or its aponeurosis with the tarsus, resulting in levator aponeurosis dehiscence, and upper eyelid ptosis. Patients with postoperative complications may require frequent follow up and/or additional surgery. The benefits of maintaining tear drainage generally far outweigh the risk of these potential complications.

Prognosis
The majority of patients who undergo repair of canalicular lacerations have anatomic and functional and anatomic success. (Fig. 9) Functional success is considered the lack of epiphora post-operatively and ability to successfully irrigate the lacrimal system. A recent retrospective review of eyelid lacerations with lacrimal apparatus involvement reported a success rate of 82%.[1] Rarely, patients require a second surgery to treat the epiphora which may result from failure of canalicular laceration repair. Entropion, ectropion, and generally poor eyelid position may necessitate further surgery. Patients may also develop ptosis that can be addressed surgically, depending on the degree of ptosis and the impact on the patient's quality of life.
Additional Resources
- American Society of Ophthalmic Plastic and Reconstructive Surgery
- AAO ONE Network: The Oculofacial Plastic Surgery Center
- Basic and Clinical Sciences Course: Orbit, Eyelids, and Lacrimal
- http://www.eyerounds.org/cases/case26.htm
References
- ↑ Jump up to: 1.0 1.1 1.2 Sadiq MA, Corkin F, Mantagos IS. Eyelid Lacerations Due to Dog Bite in Children. J Pediatr Ophthalmol Strabismus. 2015. 9:1-4
- ↑ Ali MJ, Baig F, Lakshman M, Naik MN. Scanning Electron Microscopic Features of the External and Internal Surfaces of Normal Adult Lacrimal Drainage System. Ophthalmic Plastic and Reconstructive Surgery. 2015. 31(5):414-7
- ↑ Yazici B, Yazici Z. Frequency of the Common Canaliculus. Arch Ophthalmol. 2000. 118:1381-1385
- ↑ http://www.oculist.net/downaton502/prof/ebook/duanes/pages/v5/v5c072.html
- ↑ Kang H, Takahashi Y, Nakano T, Asamoto K, Ikeda H, Kakizaki H. Medial Canthal Support Structures. Ann Plast Surg. 2015;74:508-514.
- ↑ Wulc AE, Arterberry JF. The Pathogenesis of Canalicular Laceration. 1991. Ophthalmology 98(8):1243-1249
- ↑ Jordan DR, Setareh Z, Gilberg SM, Mawn LA. Pathogenesis of Canalicular Lacerations. Ophthalmic Plastic & Reconstructive Surgery. 2008. 24(5):394-398
- ↑ Reifler DM. Management of Canalicular Laceration. Survey of Ophthalmology. 1991. 36:113-132
- ↑ Kennedy RH, May J. Daily J, Flanagan J. Canalicular Laceration: An 11-Year Epidemiologic and Clinical Study. Oculoplastic and Reconstructive Surgery. 1990;6(1):46-53.
- ↑ Hwang K, Huan F, Hwang PJ, Sohn IA. J Craniofac Surg. 2013. 24(2):671-5
- ↑ Murchison AP, Bilyk JR. Pediatric canalicular lacerations: epidemiology and variables affecting repair success. J Pediatr Ophthalmol Strabismus. 2014. 51(4):242-8.
- ↑ Jump up to: 12.0 12.1 Wladis EJ, Dewan MA. Periorbital Trauma from Pit Bull Terrier Attacks. Orbit. 2012. 31(3):200-202.
- ↑ Berris CE, Wilkins RB. Display hook injuries to the eye. Ophthalmic Surg. 1980. 11(8):526-7.
- ↑ Fannin LA, Fitch CP, Raymond WR, Flanagan JC, Mazzoli RA. Eye injuries from merchandise display hooks. American Journal of Ophthalmology. 1995. 120(3)397-399.
- ↑ Naik MN, Kelapure A, Rath S, Honavar SG. Management of canalicular lacerations: epidemiological aspects and experience with mini-monoka monocanalicular stent. American Journal of Ophthalmology. 2008. 145(2)375-380.
- ↑ Harris GJ. Canalicular Laceration at Birth. 1988. 105(3):322-323.
- ↑ Westfall CT, Shore JW, Nunery WR, Hawes MJ, Yaremchuck MJ. Operative complications of the transconjuntival inferior fornix approach. Ophthalmology. 1991. 98(10):1525-1528.
- ↑ Kennedy RH, May J, Daily J, Flanagan JC. Canalicular laceration: an 11-year epidemiologic and clinical study. Ophthalmic Plastic & Reconstructive Surgery. 1990. 6(1):46-53
- ↑ Prendes, MA, Jian-Amadi A, Shu-Hong C, Shaftel SS. Ocular Trauma from Dog Bites: Characterization, Associations, and Treatment Patterns at a Regional Level 1 Trauma Center Over 11 Years. Ophthalmic Plastic & Reconstructive Surgery. 2015.
- ↑ Loff HJ, Wobig JL, Daily RA. The bubble test: an atraumatic method for canalicular laceration repair. Ophthalmic Plastic and Reconstructive Surgery. 1996. 12(1):61-64.
- ↑ Cho SH, Hyun DW, Kang HJ, Ha MS. A simple new method for identifying the proximal cut end in lower canalicular laceration. Korean J Ophthalmol. 2008. 22(2):73-6.
- ↑ Jordan DR, Gilberg S, Mawn LA. The round-tipped, eyed pigtail probe for canalicular intubation: a review of 228 patients. Ophthalmic Plast Reconstr Surg. 2008 May-Jun;24(3):176-80. PMID: 18520830
- ↑ Örge FH, Dar SA. Canalicular laceration repair using a viscoelastic injection to locate and dilate the proximal torn edge. J AAPOS. 2015. 19(3):217-9
- ↑ Ho, Thomas, and Vickie Lee. "National survey on the management of lacrimal canalicular injury in the United Kingdom." Clinical & experimental ophthalmology 34.1 (2006): 39-43.
- ↑ Drnovšek-Olup B, Beltram M. Trauma of the Lacrimal Drainage System: Retrospective Study of 32 Patients. Croatian Medical Journal. 45(3):292-294.
- ↑ Chowdhury HR, Rose GE, Ezra DG. Long-Term Outcomes of Monocanalicular Repair of Canalicular Lacerations. Ophthalmology. 2014. 121(8):1665-1666
- ↑ Dortzbach RK, Angrist RA. Silicone intubation for lacerated lacrimal canaliculi. Ophthalmic Surg. 1985. 1:185-190
- ↑ Ho T, Lee V. National survey on the management of lacrimal canalicular injury in the United Kingdom. 2006. 34(1):39-43.
- ↑ Meyer DR, Antonello A, Linberg JV. Assessment of tear drainage after canalicular obstruction using fluorescein dye disappearance. Ophthalmology. 1990;97:1370-1374
- ↑ Jump up to: 30.0 30.1 30.2 Hawes MJ, Dortzbach RK, Segrest DR. Lacrimal Canalicular Trauma. 1994. in Ophthalmic Plastic Surgery: Prevention and Management of Complications. edited by Richard K. Dortzbach. Raven Press. Ltd., New York. pp 225-235
- ↑ Rui-feng C, Li-song H, Ji-bo Z, Li-qui W. Emergency treatment on facial laceration of dog bite wounds with immediate primary closure: a prospective randomized trial study. BMC Emerg Med. 2013;13(Suppl 1):S2
- ↑ Friedman NJ, Kaiser PK. Eyelid Trauma. in The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. 3rd Ed. pp 69-73.
- ↑ Jump up to: 33.0 33.1 33.2 Chhabra S, Chhabra N, Gaba S. Maxillofacial injuries due to animal bites. J. Maxillofac. Oral Surg. 2015. 14(2):142-153.
- ↑ Le Moal G, Landrom C, Grollier G, Rober T, and Burucoa C. Meningitis Due to Capnocytophaga canimorsus after Receipt of a Dog Bite: Case Report and Review of the Literature. Clin Infect Dis. 2002. 34:e42-46
- ↑ Pan XJ, Mao A, Zhao GQ, Meng XX, Yang SS. Clinical effects of three types of silicone intubations in repairing lacerations of canaliculus. Chin J Traumatol. 2009. 12(3):173-6.
- ↑ Jump up to: 36.0 36.1 36.2 36.3 Fountain TR. "Management of Canalicular Trauma," in Manual of Oculoplastic Surgery (4th Edition). Levine MR, Ed. 2010. pp. 33-38.
- ↑ Eo S, Park J, Cho S, Azari KK. Microsurgical Reconstruction for Canalicular Laceration Using Monostent and Mini-Monoka. Annals of Plastic Surgery. 2010. 64(4):421-427.
- ↑ Monocanalicular Stents in Eyelid Lacerations: A Report by the American Academy of Ophthalmology. Wladis EJ, Aakalu VK, Tao JP, Sobel RK, Freitag SK, Foster JA, Mawn LA. Ophthalmology. 2019 Sep;126(9):1324-1329. doi: 10.1016/j.ophtha.2019.03.045. Epub 2019 Apr 4. PMID: 30953742
- ↑ Murchison AP, Bilyk JR. Canalicular laceration repair: an analysis of variables affecting success. Ophthalmic Plast Reconstr Surg. 2014 Sep-Oct;30(5):410-4. doi: 10.1097/IOP.0000000000000133. PMID: 24777271
- ↑ Veirs ER. Malleable rods for immediate repair of the traumatically severed lacrimal canaliculus. 1962. 66:263-4
- ↑ Kaufman HE, Chapman RB. Modified probe for canaliculus surgery. Am J Ophthalmol. 1962. 54:461-2.
- ↑ Griffith TP. Polythene tubes in canaliculus surgery. Br J Ophthalmol. 1963. 47:203-10
- ↑ Smith B, Dodick JM. Repair of lid lacerations involving the lower lacrimal canaliculus. Can J Ophthalmol. 1968. 3(3):263-5
- ↑ Simons JN. Useful instrument for repair of lacerated lacrimal canaliculus. Plast Reconstr Surg. 1969. 43(1):78-80.
- ↑ Bernard JA Pasticier M, Offret G. Restoration of lacrimal canaliculi by means of a pigtail probe. Bull Soc Ophthalmol Fr. 1971. 71(4):419-25
- ↑ Kartch MC. French-eye pigtail probe for lacrimal canaliculus repair. Am J Ophthalmol. 1971. 72(6):1145-6
- ↑ Erickson BP, Ko AC, Lee WW. Novel Pigtail Cannula for a Canalicular-Involving Eyelid Laceration. Ophthal Plast Reconstr Surg. 2014. Aug 14. [Epub ahead of print]
- ↑ Saunders DH, Shannon GM, Flanagan JC. The effectiveness of the pigtail probe method of repairing canalicular lacerations. Ophthalmic surgery. 1978;9(3):33-40
- ↑ Jump up to: 49.0 49.1 Tao H, Wang P, Han C, Zhang J, Bai F, H ZY. One-stitch anastomosis through the skin with bicanalicular intubation: a modified approach for repair of bicanalicular laceration. Int J Ophthalmolo. 2013;6(5):656-658.
- ↑ Bi Y, Sui G, Zhou Q, Heindl LM, Bock F, Sun X, Tang S, Wang Z, Cursiefen. Two-step retrograde closed stenting: a novel method for treating canalicular lacerations in Chinese patients. Eye (Lond). 2013. 27(11):1275-1280.
- ↑ Jump up to: 51.0 51.1 Kersten RC. Kulwin DR. "One-stitch" Canalicular Repair. Ophthalmology. 1996;103:785-789.
- ↑ Long JA. A method of monocanalicular silicone intubation. Ophthalmic Surg. 1988;19(3):204-5
- ↑ Slonim CB. Dog bite-induced canalicular lacerations: a review of 17 cases. Ophthalmic Plastic & Reconstructive Surgery. 1996. 12(3):218-22