Basic Histology of the Eye and Accessory Structures
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Knowledge of the histology of the eye is important for understanding disease pathophysiology and treatment, as many diseases of the eye are manifestations of pathology within specific histological layers. This article describes the histological classification of the tissues of the eye and its external structures.
Accessory Structures
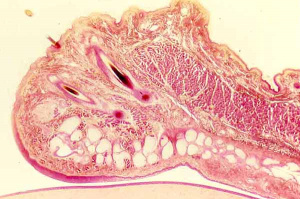
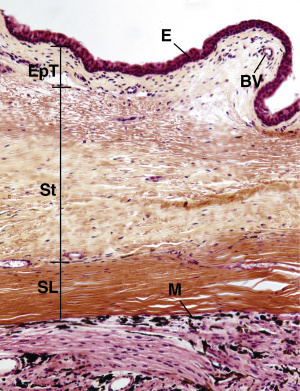
Eyelid
From superficial to deep, the eyelid is made of epidermis, dermis, the orbicularis oculi muscle, the orbital septum, the tarsal plate, and the palpebral conjunctiva.
- The epidermis is composed of layers of keratinocytes with melanocytes, Langerhans cells, and Merkel cells. The underlying basal layer is composed of a single row of columnar-shaped cells containing melanin from adjacent melanocytes.
- The dermis is a composed of delicate collagen fibrils, containing the vasculature, lymphatics, eyelashes, and nerve fibers. It also contains the following glands:
- Glands of Zeis are sebaceous glands of the eyelashes, concentrated at the lid margin
- Glands of Moll are modified apocrine sweat glands that open onto eyelash follicles.
- Eccrine sweat glands are distributed throughout the eyelid skin.
- Sebaceous glands are located in the caruncle and within eyebrow hairs. These tiny glands are associated with the thin hairs covering the periocular skin.
- The orbicularis oculi muscle is the primary protractor muscle for closure of the eyelid. It is composed of thin, circularly oriented skeletal muscle.
- The orbital septum is a thin, fibrous connective tissue that layer that separates the eyelid structures from intra-orbital structures.
- The tarsal plate is the main structural component of the eyelid. It is made of dense connective tissue and contains meibomian glands, eyelash follicles, the middle muscular bundles, and the surface epithelium.
- Meibomian glands are sebaceous glands that secrete an oily substance with a critical lipid component into the tear film in order to decrease evaporation.
- The palpebral conjunctiva is described in further detail below.
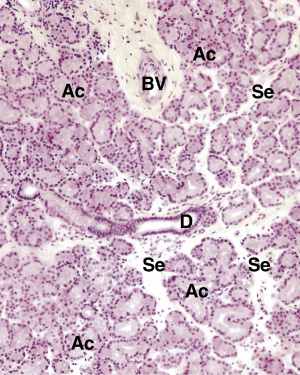
Lacrimal Apparatus
The lacrimal apparatus of the eye produces lacrimal tears in order to prevent dehydration of the eye. Dry eye syndrome is the most common eye disease, and if untreated, it can cause corneal ulcerations, scarring, and even perforation. The lacrimal apparatus is composed of four parts:
- The lacrimal gland is a serous, compound tubuloacinar gland that resembles that parotid gland. It secretes lacrimal fluid (tears) via ducts that open into the conjunctival sac at the lateral portion of the superior conjunctival fornix. Tears are composed of water and lysozyme, an antibacterial agent.
- The lacrimal canaliculi drain the lacrimal fluid away from the surface of the eye via the lacrimal punctum. They are lined by stratified, non-keratinized squamous epithelium.
- The lacrimal sac is the dilated portion of the duct system. It is lined by pseudostratified ciliated columnar epithelium and contains numerous goblet cells.
- The nasolacrimal duct delivers the lacrimal fluid to the inferior meatus on the floor of the nasal cavity. It is also lined by pseudostratified ciliated columnar epithelium.
Conjunctiva
The conjunctiva is a transparent mucous membrane that lines the inner surface of the eyelids (palpebral conjunctiva) and the anterior surface of the sclera (bulbar conjunctiva).
- It has a non-keratinized stratified squamous epithelium about five cell layers deep, containing mucus-secreting goblet cells, immune system Langerhans’ cells, and occasional melanocytes.
- Stroma (substantia propria) underlying the epithelium consists of richly vascularized loose connective tissue.
- Glands of Wolfring and Krause are accessory lacrimal glands embedded in the conjunctival stroma that secrete antibacterial agents and watery and proteinaceous components of the tear film.
- The mucoid secretions of the goblet cells contribute to the tear film that lubricates and protects the eye. The tear film is composed of an external lipid layer, a middle aqueous layer, and an inner mucoid layer that apposes the corneal epithelium.
- Conjunctiva-associated lymphoid tissue (CALT) consists of lymphocytes within the epithelial layers, and it is critical in the ocular surface immune response.
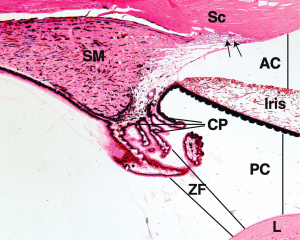
Chambers of the Eye
There are three recognized chambers of the eye:
- The anterior chamber is the space between the cornea and the iris. It is filled with aqueous humor, a water fluid produced by the ciliary body that provides nutrients and oxygen for the lens and cornea.
- The posterior chamber is the space between the posterior surface of the iris and the anterior surface of the lens. It is filled with aqueous humor.
- The vitreous chamber is the space between the posterior surface of the lens and the retina. It is filled with the vitreous body, a transparent gel that is made of 99% water, in addition to extremely delicate type II collagen fibers, hyaluronic acid, and electrolytes.
- Hyalocytes are small cells that can be found at the periphery of the vitreous body, which are believed to synthesize collagen and hyaluronic acid.
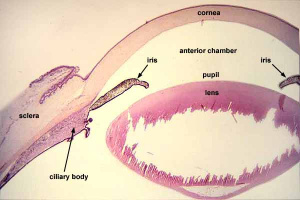
Internal Structures of the Eye
The eyeball is composed of three principal layers: the fibrous tunic, the vascular tunic, and the neural tunic.
- The fibrous tunic is the outer layer, consisting of the sclera and cornea.
- The vascular tunic, also called the uvea, consists of the iris, the ciliary body, and the choroid.
- The lens is a specialized epithelial structure located behind the pupil.
- The inner layer is the neural tunic, consisting of the retina.
Sclera
The white, opaque sclera is a tough fibrous connective tissue layer that provides the architectural support for the shape of the eyeball.
Structure/histology:
- The conjunctiva covers its external surface.
- There are three indistinct layers, described from superficial to deep:
- The episclera is a thin, loose, collagenous connective tissue.
- The stroma is a thick layer of dense, collagenous connective tissue made of interlacing type I collagen fibers alternating with networks of elastic fibers.
- The suprachoroid lamina is a thin connective tissue layer containing fibroblasts and melanocytes.
- The sclera-corneal junction is called the limbus. Here, the deep surface of the suprachoroid lamina is covered by the scleral endothelium, a simple squamous epithelium. The limbus is the location of corneal stem cells.
- The sclera is nearly avascular, although it does have some visible blood vessels that pierce the surface to reach the retina below.
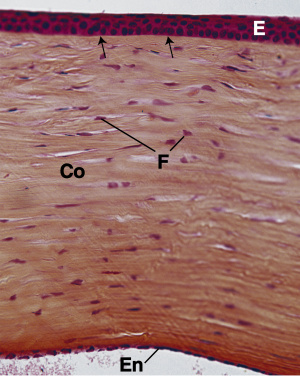
Cornea
The cornea is a modified mucous membrane that covers the anterior portion of the eye. Its tissue elements are highly specialized to order to maintain transparency. It is composed of six histologically distinct layers, from superficial to deep:
- The epithelium is a thin, non-keratinized stratified squamous epithelium composed of approximately 5 layers of cells. It is highly innervated by pain fibers.
- Bowman’s membrane is a thick acellular layer that underlies the corneal epithelial basal cell basement membrane. It is composed of type I collagen fibers.
- The stroma makes up approximately 90% of the cornea. It is composed of bundles of type I collagen fibers interspersed with fibroblasts and elastic fibers. The collagen bundles are organized into extremely regular layers. The fibers within each layer are parallel to one another, and alternating layers run in different directions.
- Descemet’s membrane is the basement membrane of the corneal endothelium. It is secreted by the endothelium and thickens from 5um at birth to 17um in older adults.
- The endothelium lines the posterior surface of the cornea. It is a single layer of simple squamous to simple cuboidal cells. The cells have sodium pumps in their membranes that transport positively charged sodium ions in the anterior chamber, followed passively by negatively charged chloride ions and water. This keeps the stroma relatively dehydrated in order to maintain transparency.
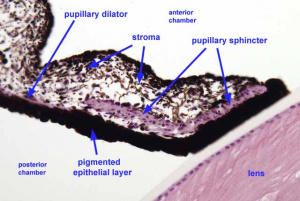
Iris
The iris is a colored, opaque ring that covers the front of the lens and functions to regulate the pupil diameter.
Structure/Histology
- The anterior surface of the iris has no overlying epithelium and consists of loose connective tissue, blood vessels, melanocytes, and fibroblasts. Variation in eye color results from individual differences in the distribution and density of melanocytes.
- The stroma of the iris is a poorly vascularized connective tissue containing numerous fibroblasts and melanocytes.
- The posterior surface of the iris has two cell layers:
- The surface that faces the stroma is a less pigmented anterior epithelium that consists of myoepithelial cells and forms the pupillary dilator muscle. The pupillary dilator muscle receives sympathetic innervation to dilate the pupil.
- The surface that faces the lens is a heavily pigmented posterior epithelium that continues as the ciliary body, described below.
- The papillary sphincter muscle is a band of circularly arranged smooth muscle at the pupillary margin of the iris that receives parasympathetic innervation to constrict the pupil.
- The angle is where the iris meets the cornea. It contains connective tissue with endothelial channels called the trabecular meshwork, which drains aqueous humor in the anterior chamber into the venous canal of Schlemm.
Ciliary Body
The ciliary body is a ring of smooth muscle that spans the inner wall of the eye at the level of the lens. It suspends the lens in place via suspensory ligaments and functions primarily to control the shape of the lens and produce aqueous humor.
Aqueous humor production
- The medial surface of the ciliary body that projects towards the lens is folded into small projections called ciliary processes.
- The ciliary processes are covered by 2 layers of epithelium:
- The inner layer is a pigmented layer of simple columnar epithelium that is rich in melanin. These cells are responsible for aqueous humor production.
- The outer layer that faces the lumen is a non-pigmented columnar epithelium that is continuous with the ganglion cell layer of the retina. These cells are highly eosinophilic due to their high mitochondrial content and ion channels.
- Once produced, aqueous humor seeps into the anterior chamber through the pupillary aperture between the iris and the lens.
Lens control
- The bulk of the ciliary body is composed of the ciliary muscle, which consists of three bundles of smooth muscle.
- Thin fibers of collagen called zonules or suspensory ligaments surround the lens at the equator. They run from the lens to the ciliary body, anchoring the lens and allowing the ciliary muscle to determine the curvature of the lens.
- During accommodation for near vision, the ciliary muscle contracts. This decreases tension on the suspensory ligaments, causing the lens to relax and become thicker and more spherical, thus increasing its focal power.
- For distance vision, the muscles relax, which increases tension on the suspensory ligaments. This stretches and flattens the lens, decreasing its focal power.
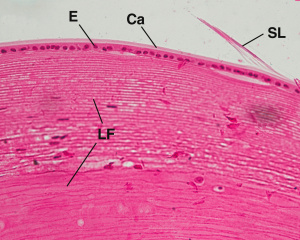
Lens
The lens is a transparent biconvex disc located directly behind the pupil. It consists of three parts: the lens capsule, the subcapsular epithelium, and the lens.
Structure/Histology
- The lens capsule is the basement membrane of the underlying lens epithelium. It is the thickest basement membrane in the body, containing mostly type IV collagen and glycoprotein. It envelops the entire lens, and the underlying epithelial cells are unable to desquamate.
- The subcapsular epithelium is located immediately deep to the lens capsule, on the anterior and lateral aspects of the lens. It is composed of a single layer of cuboidal cells that are more squamous anteriorly and become taller posteriorly, towards the lens equator. These cells give rise to the cells that ultimately mature into lens fibers.
- The lens fibers make up the substance of the lens. They are hexagonal shaped cells that arise from the subcapsular epithelium and lose their nuclei and organelles, elongating until they reach a length of 7-10um. Eventually, the cells become filled with special lens proteins known as crystallins that increase the refractory index of the lens.
Choroid
The choroid is a heavily pigmented layer containing a dense network of blood vessels that serves to provide nutrients to the retina and absorb light. It is loosely attached to the sclera and separated from the retina by Bruch’s membrane.
Structure/Histology
- The choroid is composed of loose connective tissue containing numerous fibroblasts and other connective tissue cells.
- The layer closest to the sclera is a layer of pigmented melanocytes, which gives the membrane a black color.
- The inner surface is known as the choriocapillary layer due to the abundance of small blood vessels. This layer is responsible for providing nutrients to the retina.
- The choroid is separated from the retina by the 1-4um Bruch’s membrane. Bruch’s membrane consists of an inner layer of elastic fibers surrounded by collagen fibers. The collagen is covered by the basement membrane of the choroid on one side and the basement membrane of the retinal pigment epithelium on the other side.
- Bruch’s membrane consists of an inner layer of elastic fibers surrounded by collagen fibers. The collagen is covered by a basement membrane that belongs to the choroid on one side and the retinal pigment epithelium on the other side.

Retina
The retina is formed by the outer retinal pigment epithelium (RPE) and the inner neural retina, a multilayered structure containing photoreceptor cells and supportive cells. It can be organized into 10 distinct layers, beginning with the RPE, which lies adjacent to Bruch’s membrane and the choroid, to the internal limiting membrane, which meets the vitreous humor:
1. Retinal pigment epithelium (RPE): The RPE consists of cuboidal to columnar epithelial cells that contain an abundance of melanin granules in order to absorb light and reduce random reflections of unabsorbed light.
- The lateral cell membranes form the blood-retina barrier and contain gap junctions for intercellular communication.
- The cell apices contain processes that interdigitate with, but are not attached to, the outer segments of rods and cones.
- Clinical correlate: retinal detachment occurs when the pigmented epithelial cells disengage with the photoreceptor rod and cone tips due to sudden hard jolts.
2. Layer of rods and cones (photoreceptor layer): This layer contains the outer segments of the photoreceptor cells—the rods and cones. Rods are the photoreceptor cells specialized for perceiving dim light, while cones are specialized for perceiving bright light and color.
- Clinical correlate: Vitamin A deficiency can cause night blindness because vitamin A is converted into a component of rhodopsin, a light-sensitive pigment contained in rods.
3. External limiting membrane (ELM): The ELM is not a true membrane, but it is a region of zonulae adherents between the photoreceptor cells and Muller cells. Muller cells provide structural and nutritional support for the retinal neurons.
4. Outer nuclear layer: This layer contains the cell bodies of the photoreceptor cells. Rods and cones can be distinguished histologically by their nuclei—the nuclei of rods are smaller, more rounded, and more darkly stained than the nuclei of cones.
5. Outer plexiform layer: This layer contains the synapses between the axons of photoreceptor cells and the dendrites of intermediate neurons (bipolar and horizontal cells).
6. Inner nuclear layer: This layer contains the cell bodies of the intermediate neurons (bipolar, horizontal, and amacrine cells) and Muller cells.
7. Inner plexiform layer: This layer contains the synapses between the axons of bipolar cells and the dendrites of ganglion cells and amacrine cells.
8. Ganglion cell layer: This layer contains the cell bodies of ganglion cells, the neurons whose axons travel in the optic nerve and project to the brain.
9. Optic nerve fiber layer: This layer contains the axons of ganglion cells. The nerve fibers are formed of unmyelinated axons, which become myelinated as the nerve exits the sclera.
10. Internal limiting membrane (ILM): The ILM is composed of the basement membrane of Muller cells, which separates the retina from the vitreous humor.
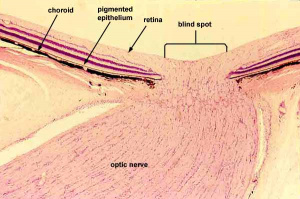
Optic disc
The optic disc is the site at which the axons from the retinal ganglion cells converge and exit the eye via the optic nerve. The optic disc contains no photoreceptor cells and creates the blind spot of the retina.
Macula and Fovea
The macula is a yellow-pigmented zone lateral to the optic disc, approximately 5.5mm in diameter. The fovea is an approximately 1.5mm area of specialized avascular retina that can be identified as a depression in the retina in cross-section. The foveola is the central floor of the fovea, approximately 0.35mm in diameter, and is the area of retina with the greatest visual acuity. It can be differentiated from the fovea histologically by an absence of ganglion cells and rods. The cones in this area are narrower than in other parts of the retina, allowing for more cones per unit area.
Additional Resources
- Boyd K, Gregori NZ, Mendoza O, Porter D, Turbert D. Aqueous Humor. Bowman's membrane. Choroid. Ciliary Body. Cones. Cornea. Descemet's Membrane. Endothelium. Epithelium. Eye Anatomy Overview. Fovea. Fundus. Iris. Lens Capsule. Lens. Meibomian Glands. Parts of the Eye. Retina. Sclera. Stroma. Uvea. Vitreous. Zonules. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health Accessed November 17, 2022.
References
- Bloom J, Motlagh M, Czyz CN. Anatomy, Head and Neck, Eye Iris Sphincter Muscle. [Updated 2020 Aug 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-.Available from: https://www.ncbi.nlm.nih.gov/books/NBK532252/
- Cochran ML, Lopez MJ, Czyz CN. Anatomy, Head and Neck, Eyelid. [Updated 2020 Aug 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482304/
- Delamere NA. Ciliary Body and Ciliary Epithelium. Adv Organ Biol. 2005;10:127-148. doi:10.1016/S1569-2590(05)10005-6.
- Goel M, Picciani RG, Lee RK, Bhattacharya SK. Aqueous humor dynamics: a review. Open Ophthalmol J. 2010;4:52-59. Published 2010 Sep 3. doi:10.2174/1874364101004010052.
- Hejtmancik JF, Shiels A. Overview of the Lens. Prog Mol Biol Transl Sci. 2015;134:119-127. doi:10.1016/bs.pmbts.2015.04.006
- Joyce C, Le PH, Sadiq NM. Histology, Retina. [Updated 2020 Sep 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546692/
- Lowe JS. Chapter 19: Special Senses: Eye. In: Stevens & Lowe’s human histology, 5th edition. Elsevier; 2020.
- Nickla DL, Wallman J. The multifunctional choroid. Prog Retin Eye Res. 2010;29(2):144-168. doi:10.1016/j.preteyeres.2009.12.002.
- Pradeep T, Mehra D, Le PH. Histology, Eye. [Updated 2020 Jul 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544343/
- Salmon JF. Kanski’s clinical ophthalmology. Elsevier, 2020.
- Sridhar MS. Anatomy of cornea and ocular surface. Indian J Ophthalmol. 2018;66(2):190-194. doi:10.4103/ijo.IJO_646_17
- Yanoff M. Ocular Pathology. Elsevier, 2020.