Bacillary Layer Detachment in Retina
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Bacillary layer detachment (BALAD) is an optical coherence tomography (OCT) finding noted in many uveitic and retinal diseases which refers to splitting at the level of the photoreceptor inner segment myoid and accumulation of intraretinal fluid.
Disease
Bacillary layer detachment (BALAD) is an optical coherence tomography (OCT) finding noted in many uveitic and retinal diseases. It refers to an OCT finding of splitting at the level of the inner segment myoid of photoreceptors leading to development of intraretinal fluid cavities. [1]
There is a separation of the bacillary layer from the other retinal layers due to a split at the photoreceptors immediately posterior to the external limiting membrane (ELM) within the photoreceptor inner segment (IS) myoid.
The intraretinal fluid is bounded by the myoid and externally by the ellipsoid zone (EZ) and photoreceptor outer segments (OS), the latter two usually remain attached to the retinal pigment epithelium (RPE).
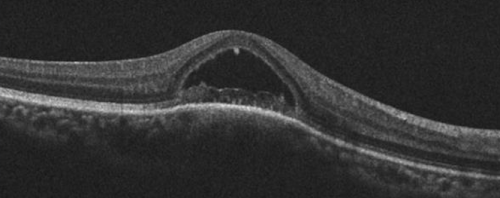
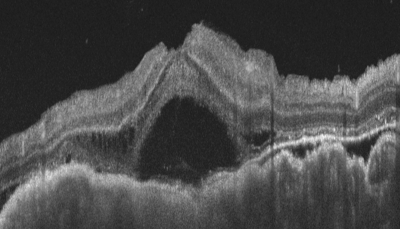
Figure 1 shows an OCT with BALAD
Etiology
BALAD is seen in multiple conditions as shown in Table 1. [2] [3] [4]
Table 1: Retinal and uveitis conditions where BALAD is seen
| Inflammatory conditions – infectious and non-infectious | Toxoplasma Chorioretinitis
Tuberculous Serpiginous Choroiditis Tubercular choroidal granuloma Endophthalmitis Vogt-Koyanagi-Harada (VKH) disease Sympathetic ophthalmia Acute Idiopathic Maculopathy (AIM) Posterior scleritis Acute posterior multifocal placoid pigment epitheliopathy (APMPPE) Chikungunya associated uveitis |
| Degenerative | Neovascular age related macular degeneration (AMD) |
| Pachychoroid conditions | Central serous chorioretinopathy (CSCR)
Peripapillary pachychoroid syndrome Pachychoroid spectrum |
| Vascular | Hypertensive retinopathy
Preeclampsia Diabetic retinopathy Retinal vein occlusion Macular Telengiectasia Type 2 |
| Tumours | Choroidal osteoma
Choroidal lymphoma Choroidal metastasis Choroidal melanoma Bilateral diffuse Uveal melanocytic proliferation (BDUMP) |
| Trauma | Blunt trauma
Choroidal rupture |
| Drug induced | Dabrafenib (anti-BRAF)
Trametinib (anti-MEK) Other immunotherapy related toxicities |
| Laser induced | Laser induced maculopathy
Panretinal photocoagulation Photodynamic therapy|- |
| Others | Pathological myopia
Retinal Detachment |
History
- BALAD was first reported by Mehta et al in 2018 in patients with toxoplasma chorioretinitis and pachychoroid disease. [1]
- The term “Bacillary” was used as it is said to refer the photoreceptor inner and outer segment (IS-OS). [5]
- It was described by van Leeuwenhoek in the 1700s as ‘stratum bacillorum et conorum’. [6]
- Later in the 1940s, Polyak described the bacillary layer as the photoreceptor IS-OS. [5]
- The fluid accumulates between the innermost hyperreflective band ie the ELM and second innermost hyperreflective band ie the ellipsoid zone (EZ).
- It was earlier reported in other diseases such as VKH as subretinal sepatae, ocular toxoplasmosis as subretinal fluid and neovascular AMD as atypical outer retinal fluid but was not named until 2018. [7][8]
Anatomy
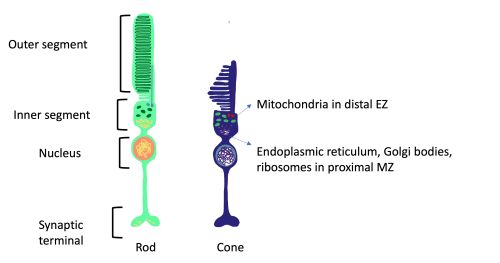
The outer retina consists of the RPE as the outer most layer followed by the the interdigitation zone (IZ), the photoreceptor OS, photoreceptor IS which is divided into a distal ellipsoid zone (EZ) and proximal myoid zone (MZ) and the ELM. The MZ contains Golgi bodies, ribosomes and endoplastic reticulum while the EZ has densely packed mitochondria. [9]
Figure 2 shows anatomy of rod and cone photoreceptors
The outer segment of the photoreceptors attaches to the RPE with the help of RPE microvilli and glycosaminoglycans in the photoreceptor matrix between the outer segments. Muller cells attaches to inner segment of photoreceptors to form a semi-permeable barrier, ie ELM. The photoreceptor IS myoids structure is not as strong as the ELM and EZ which makes it a zone of weakness, susceptible to splitting as seen in BALAD. [4]
General Pathology
- Although histology has shown that the photoreceptor IS myoid and ellipsoid were anatomically continuous in a single cell, Mehta et al noted that there is a zone of weakness in the photoreceptor IS myoid in light microscopy preparations of the retina. [1]
- There is no direct histopathological correlation and BALAD can be either a split within photoreceptor MZ or EZ or junction between the two.
Pathogenesis
- When forces directed outwards leading to attachment of photoreceptor OS to the RPE are more than the photoreceptor IS myoid’s tensile strength, the MZ splits leading to development of BALAD. The photoreceptor EZ is attached to the RPE/Bruch’s membrane complex and intraretinal fluid accumulation lifts the ELM leading to creation of a cleavage plane at the inner segment myoid.
- According to Mehta et al, two factors are required to form BALAD: [1]
- Hydrostatic force from the choroid which has enough strength to split the photoreceptors.
- A space in the zone of weakness of the photoreceptor IS myoid within the ELM and EZ
- Retinal acute fluid accumulation (RAFA) ie sudden and rapid influx of intraretinal and subretinal fluid is said to be more responsible for development of BALAD than underlying inflammation. [10]
- Choroidal ischemia is another possible pathogenesis for BALAD. BALAD patients are found to have increased choroidal thickness which is associated with conditions such as VKH, sympathetic ophthalmia, APMPPE etc which can have BALAD. BALAD also responds well to steroid therapy or plasmapheresis which adds to this theory. [2][11]
- Shearing forces by subretinal hyperreflective material in nAMD and shearing forces in ocular trauma can cause separation of the MZ. [4]
OCT Findings [1] [2]
In a review of BALAD by Ramtohul et al, following OCT hallmarks were noted:[2]
- Splitting of the hyporeflective photoreceptor MZ
- Presence of intraretinal cystic pockets
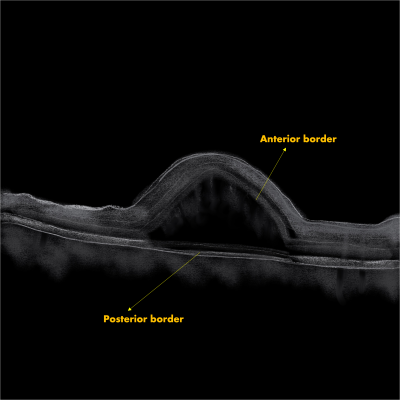
- Borders: Anterior border/ceiling: granular hyperreflective band Posterior border/floor- continuation of EZ of adjacent retina with variable thickness and reflectivity - detached photoreceptor IS and OS which remains adherent to RPE Bruch's complex Figure 3 shows anterior and posterior border of BALAD on OCT
- In almost half of the cases, there is a second hyperreflective band below the posterior border which was continuous with the IZ of adjacent retina
- ELM noted anterior to BALAD in majority of the cases
- Suspended hyperreflective materials in the cystic cavities of BALAD with medium internal optical intensity
- Piriform shape with acute angles at base in a majority of the cases
- Associated SRF
- Focal adhesions between outer retina and RPE-Bruch's complex near margin of BALAD
- Edema/schisis in Henle's layer adjacent to BALAD
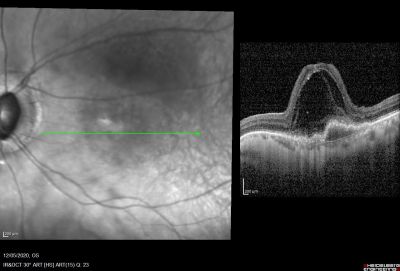
Figure 4 showing BALAD in an OCT of a patient with neovascular AMD
Figure 5 showing BALAD in an OCT of a patient with choroidal metastasis
Clinical Findings & Other Investigations [2][3] [4]
- Most common location fovea > parafoveal > peripapillary region.
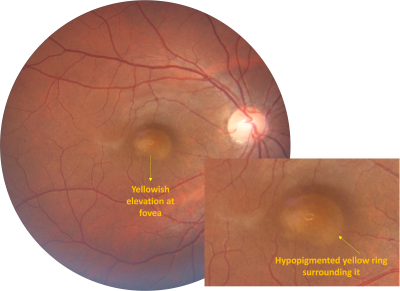
- Fundus examination/photography: Similar to subretinal fluid (SRF)- Well circumscribed round/oval elevation at the fovea, yellow-gray in colour surrounded by a hypopigmented yellow ring (Figure 6)
- Fundus autofluorescence : Central hypoautofluorescence due to masking of RPE autofluroscence by exudation or disruption of RPE or both with a peripheral hyperautofluorescence ring in the lesion
- Near-infrared reflectance & En-face OCT images : Hyporeflective lesions with a thin hyperreflective ring at the edge of BALAD
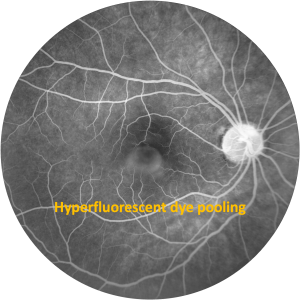
- Fundus fluorescein angiography (FFA): Hyperflurosence due to dye pooling within BALAD similar to serous retinal pigment epithelial detachment. Late phase has hypofluroscent boundaries (Figure 7).
- Indocyanine green angiography (ICGA): May have early hypofluorescence lesions indicating poor choroidal perfusion.
- Optical coherence tomography angiography (OCTA): Subretinal neovascularization in nAMD and type 2 MNV , Reduced capillary blood flow in toxoplasmosis chorioretinitis, APMPPE, and AIM
Yellow margin on fundus photography, hyperreflective ring on near infrared imaging, hypofluorscent borders in late phase of FFA and BALAD angles on OCT all correspond to each other.
Differential diagnosis
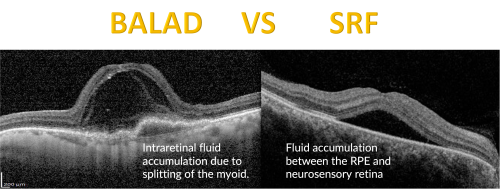
- BALAD needs to be differentiated from SRF/ serous retinal detachment (SRD). SRF is fluid accumulation between the RPE and neurosensory retina, whereas BALAD is splitting of the myoid (Figure 8). Fluid of SRF is more hyporeflective compared to a hyperreflective material in BALAD suggestive of fibrin with IS-OS debris. [1] [12] [13]
- Hemorrhagic BALAD – Blood within BALAD cavity - Seen in cases of macular neovascularisation should be differentiated from submacular hemorrhage as the latter will require different treatment [14]
- BALAD also needs to be differentiates from retinoschisis, the latter has connecting fibres or strands on OCT [2]
Management
Underlying cause has to be identified and treated for resolution of BALAD.
For example, neovascular AMD is treated with appropriate intravitreal anti-VEGF agents and inflammatory conditions are treated with steroids and immunosuppressive agents.
Clinical Significance and Prognosis
- Visual recovery is associated with resolution of BALAD – faster initiation of treatment, more rapid recovery of photoreceptors and better visual prognosis [3]
- Hemorrhagic BALAD and SHRM are risks for development of subretinal fibrosis, which has a poor visual prognosis. [2]
- BALAD can be a biomarker for poor visual prognosis in VKH [15]
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 1.5 Mehta N, Chong J, Tsui E, Duncan JL, Curcio CA, Freund KB, et al. Presumed foveal bacillary layer detachment in a patient with toxoplasmosis chorioretinitis and pachychoroid disease. Retin Cases Brief Rep 2021;15:391–8.
- ↑ Jump up to: 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Ramtohul P, Engelbert M, Malclès A, Gigon E, Miserocchi E, Modorati G, Cunha de Souza E, Besirli CG, Curcio CA, Freund KB. BACILLARY LAYER DETACHMENT: MULTIMODAL IMAGING AND HISTOLOGIC EVIDENCE OF A NOVEL OPTICAL COHERENCE TOMOGRAPHY TERMINOLOGY: Literature Review and Proposed Theory. Retina. 2021 Nov 1;41(11):2193-2207. doi: 10.1097/IAE.0000000000003217. PMID: 34029276.
- ↑ Jump up to: 3.0 3.1 3.2 Durmaz Engin C, Saatci AO. The revival of an old term with optical coherence tomography: Bacillary layer detachment. EUROPEAN EYE RESEARCH. 2022 Dec 1;2(4):180-8.
- ↑ Jump up to: 4.0 4.1 4.2 4.3 Di X, Yishuang X, Changzheng C. Conception and features of bacillary layer detachment.
- ↑ Jump up to: 5.0 5.1 Polyak SL. The Retina: The Anatomy and the Histology of the Retina in Man, Ape, and Monkey, Including the Consideration of Visual Functions, the History of Physiological Optics, and the Histological Laboratory Technique. Chicago: University of Chicago Press; 1941.
- ↑ Van Leeuwenhoek A. Historical review. Acta Ophthalmol 1935;13:13–28.
- ↑ Ishihara K, Hangai M, Kita M, Yoshimura N. Acute Vogt-Koyanagi-Harada disease in enhanced spectral-domain optical coherence tomography. Ophthalmology. 2009;116(9):1799–1807.
- ↑ Liakopoulos S, Keane PA, Ristau T, Kirchhof B, Walsh AC, Sadda SR. Atypical outer retinal fluid accumulation in choroidal neovascularization: a novel OCT finding. Ophthalmic Surg Lasers Imaging Retina. 2013;44(6 Suppl):S11–18.
- ↑ Spaide RF, Curcio CA. Anatomical correlates to the bands seen in the outer retina by optical coherence tomography: lit- erature review and model. Retina 2011;31:1609–1619.
- ↑ Agarwal A. Commentary: Bacillary layer detachment in retinochoroidal pathologies: The concept of retinal acute fluid accumulation. Indian J Ophthalmol Case Rep 2021;1:665-6
- ↑ Kohli GM, Bhatia P, Shenoy P, Sen A, Gupta A. Bacillary layer de- tachment in hyper-acute stage of acute posterior multifocal placoid pigment epitheliopathy: A case series. Ocul Immunol Inflamm 2020;30:703–6.
- ↑ Agarwal A, Freund KB, Kumar A, Aggarwal K, Sharma D, Ka- toch D, et al. Bacillary layer detachment in acute Vogt-Koyan- agi-Harada disease: A novel swept-source optical coherence tomography analysis. Retina 2021;41:774–83.
- ↑ Jung JJ, Soh YQ, Yu DJ, Rofagha S, Lee SS, Freund KB, et al. Bac- illary layer detachment because of macular neovasculariza- tion. Retina 2021;41:2106–14.
- ↑ Ramtohul P, Comet A, Denis D, Gascon P. Hemorrhagic bacillary layer detachment in macular telangiectasia Type 2. Retina 2021;41:e42–3.
- ↑ Missaka RF, Goldbaum M, Machado CG, Souto FM, Nóbrega PF, Lavezzo MM, et al. Bacillary layer detachment in Vogt-Koy- anagi-Harada disease: A biomarker with prognostic value. In- vest Ophthalmol Vis Sci 2022;63:3361–F0170.