Autokeratoplasty
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Background
Corneal autograft, or autokeratoplasty, is a relatively uncommon procedure which uses one’s own cornea to replace damaged cornea. There are two types: Ipsilateral Rotational Autokeratoplasty (IRA) and Penetrating Bilateral Autokeratoplasty. In this article we will describe and compare both procedures.
History
Corneal autografts have been a known surgical technique to address corneal opacities for many years. Both IRA and bilateral autokeratoplasty were first recorded within the literature in 1912 and 1908, respectively.[1] Now more than a century later, nearly all aspects of the procedure have been further developed for improved visual acuity, safety, cosmetic appearance, and surgical ease. However, given the limited indications and variety of alternatives such as rigid gas permeable and scleral contact lenses, anterior allogenic lamellar keratoplasty, penetrating allogenic keratoplasty, and keratoprosthesis, corneal autografts are relatively rare procedures.
Indications
Ipsilateral Rotational Autokeratoplasty
- Non-progressive central corneal opacity involving the visual axis. Based on previous literature, this may be secondary to blunt and/or penetrating trauma, postinfectious keratitis, congenital opacities, chemical injuries, or advanced lipid keratopathy.[2]
- At least 4[3][4] or 5[5] mm of clear cornea in periphery.
- Patients with high risk of allogenic graft rejection. This may include those with densely vascularized corneal opacities, previous allogenic graft rejection, or children.
- Patients in areas with poor access to donor material.
Penetrating Bilateral Autokeratoplasty
- Primary, non-progressive corneal disease limited to the cornea.
- Contralateral eye with healthy cornea and limited visual potential (e.g. retinal disease, optic nerve disease, amblyopia).
- Patients with high risk of allogenic graft rejection. This may include those with densely vascularized corneal opacities, previous allogenic graft rejection, or children.
- Patients in areas with poor access to donor material.
Contraindications
- Progressive or uncontrolled underlying disease
- Insufficient clear peripheral cornea for IRA
- Useful vision in the contralateral eye in the case of bilateral autokeratoplasty
Surgical Technique
Ipsilateral Rotational Autokeratoplasty
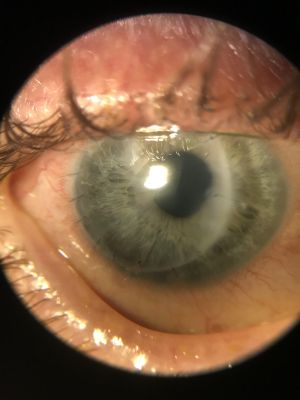
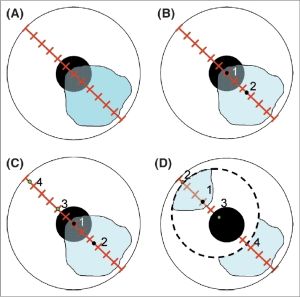
- The goal of this procedure is to achieve 5 mm (minimum 3 mm) of central clear cornea to maximize visual acuity (Fig 1). Additionally, rotation of the opacity below the upper eyelid is desired for maximal cosmetic benefit.
- Optimal Size and Location
- Measuring the size and location of trephination is challenging and complex. While several case studies have been reported, there are no clear guidelines to calculate the area of trephination given the rarity of ipsilateral autokeratoplasty.
- One simplified approach involves a series of 4 marks along the eye. For example, mark the center of the cornea (1), a point 2 mm towards the opacity (2), 1.5 mm from the central mark in the opposite direction, and finally mark a maximal distance toward the limbus (4) (Fig 2). In this case, point 3 is considered the axis of rotation. Exact measurements may depend on the area of opacification and location of clear cornea.[6] Other surgeons have also used more geometric formulae based on digital photographs.[7] Perhaps the most cited formula in the literature is Dt=1.5x Dcl+e (Dt=trephine diameter, Dcl=diameter of largest area of clear cornea, e=shortest distance from center of cornea to the clear-opaque junction).[8] The formula’s ease-of-use and reliability make it a popular choice among surgeons.
- A surgeon may also utilize computer simulation and imaging software to optimize the size, location, and rotation of the graft as well as the opacity position.[9][10]
- After selecting the size and area of the trephine, the following steps should be performed:
- The surgeon may mark the trephine area with an RK marker.
- The cornea is entered with a paracentesis blade and the anterior chamber is filled with viscoelastic.
- The cornea is trephined.
- The trephined cornea is rotated.
- The final steps consist of suturing the trephined cornea, and are similar to that of Penetrating Keratoplasty.
Penetrating Bilateral Autokeratoplasty
- The surgical steps share many commonalities with penetrating keratoplasty.[11]
- Partially trephinate the donor healthy cornea from the eye with limited visual potential.
- Carefully remove the healthy corneal autograft with corneoscleral scissors. Take extra care with the tissue, since there is no alternative autograft available.
- Place a temporary keratoprosthesis in the donor eye to stabilize integrity until completion of autografting in the eye with good visual potential[12]
- Cover the donor eye with an eye shield
- Using a similar procedure, trephinate and remove the diseased cornea from the eye with good visual potential. Take extra care with the tissue, since there is no alternative graft available to suture in the donor eye
- Suture the healthy autograft onto the eye with good visual potential with similar technique to that of Penetrating Keratoplasty.
- Replace the temporary keratoprosthesis in the donor eye with the corneal tissue from the eye with good visual potential suturing with a similar technique to that of Penetrating Keratoplasty
Intraoperative Complications
- Irregular trephination
- Trephinating too close to the visual axis for IRA
- Poor graft centration in bilateral autokeratoplasty
- Damage to the iris or lens
- Damage to the autograft
- Choroidal hemorrhage and effusion
Postoperative Complications
- Wound leak
- Glaucoma
- Endophthalmitis
- Primary endothelial failure
- Persistent epithelial defect
- Microbial keratitis. There is additional risk of microbial keratitis in the contralateral eye after penetrating bilateral autokeratoplasty.
- Recurrence of primary disease
- Introduction of new disease process to eye with good visual potential from corneal tissue of donor eye
- While graft rejection may be a primary concern for penetrating keratoplasty, there is no separate donor in an autograft. Therefore, there is theoretically no risk of graft rejection with autokeratoplasty.
Outcomes
Ipsilateral Rotational Autokeratoplasty
Due to the low surgical volume of IRAs, current data is limited to several case series of widely varying quality.[13] Analysis shows significant improvement in visual acuity in isolation and decreased endothelial cell loss when compared to penetrating keratoplasties (PKs). However, one study also noted significantly lower post-op visual acuity and higher post-op astigmatism when compared to PKs.[14] There are several theories for the increased astigmatism, including eccentric trephination, disparity of corneal thickness at the junction site, and proximity of the junction site to the corneal pupillary zone.
Penetrating Bilateral Autokeratoplasty
Penetrating Bilateral Autokeratoplasty is a rarely performed procedure, given the scarcity of patients with both the specific corneal opacity requirements, and a healthy contralateral cornea with limited visual potential. A Spanish 2020 study by Sanjuán, et al. reviewed 31 eyes of 31 patients receiving penetrating bilateral autokeratoplasty. The cumulative probabilities for anatomic success were 100%, 72%, and 38%, and 77%, 59%, and 29% for functional success at 1, 10, and 40 years, respectively. The most significant risk factor for graft failure was glaucoma, present in 50% of anatomic failures and 77% of functional failures.[15]
References
- ↑ Andrew E. Forster. A Review of Keratoplastic Surgery and Some Experiments in Keratoplasty. American Journal of Ophthalmology, Volume 6, Issue 5, 1923, Pages 366-375, ISSN 0002-9394, https://doi.org/10.1016/S0002-9394(23)90004-8.
- ↑ Arnalich-Montiel, F., Dart, J. Ipsilateral rotational autokeratoplasty: a review. Eye 23, 1931–1938 (2009). https://doi.org/10.1038/eye.2008.386
- ↑ Sah WJ, Myoung YW, Hahn TW, Kim JH. Rotational autokeratoplasty in advanced lipid keratopathy. Ophthalmic Surg Lasers 1997; 28: 1020–1024.
- ↑ McDonnell PJ, Falcon MG. Rotational autokeratoplasty. Eye 1989; 3 (Part 5): 576–580.
- ↑ Murthy S, Bansal AK, Sridhar MS, Rao GN . Ipsilateral rotational autokeratoplasty: an alternative to penetrating keratoplasty in nonprogressive central corneal scars. Cornea 2001; 20: 455–457.
- ↑ Rao SK, Lam DS. Calculating graft size and position in rotational corneal autografting: a simplified approach. Indian J Ophthalmol. 2008 May-Jun;56(3):233-5. doi: 10.4103/0301-4738.40364. PMID: 18417826; PMCID: PMC2636109.
- ↑ Afshari NA, Duncan SM, Tanhehco TY, Azar DT. Optimal Size and Location for Corneal Rotational Autografts: A Simplified Mathematical Model. Arch Ophthalmol. 2006;124(3):410–413. doi:10.1001/archopht.124.3.410
- ↑ William M. Bourne, Richard F. Brubaker, A Method for Ipsilateral Rotational Autokeratoplasty, Ophthalmology, Volume 85, Issue 12, 1978, Pages 1312-1316, ISSN 0161-6420, https://doi.org/10.1016/S0161-6420(78)35561-5.
- ↑ Agarwal T, Sharma N, Jhanji V, et al. Computer simulation-assisted rotational autokeratoplasty with pupillary enlargement for management of cases with partial corneal opacification. Br J Ophthalmol. 2010;94:24–25.
- ↑ Bower KS, Mines MJ, Stutzman RD. Digital imaging to assist preoperative planning for ipsilateral rotational autokeratoplasty. J Telemed Telecare. 2006;12:374–376.
- ↑ Sharma, Namrata M.D.; Sachdev, Ritika M.S.; Titiyal, Jeewan S. M.D.; Tandon, Radhika M.D.; Vajpayee, Rasik B. M.D.. Penetrating Autokeratoplasty for Unilateral Corneal Opacification. Eye & Contact Lens: Science & Clinical Practice 38(2):p 112-115, March 2012. DOI: 10.1097/ICL.0b013e318243e82c
- ↑ Rao SK, Fogla R, Sitalakshmi G, Padmanabhan P. Ophthalmic Surgery, Lasers and Imaging Retina, 2013;31(6):457–461. https://doi.org/10.3928/1542-8877-20001101-04
- ↑ Arnalich-Montiel, F., Dart, J. Ipsilateral rotational autokeratoplasty: a review. Eye 23, 1931–1938 (2009). https://doi.org/10.1038/eye.2008.386
- ↑ Jonas JB, Rank RM, Budde WM . Autologous ipsilateral rotating penetrating keratoplasty. Am J Ophthalmol 2001; 131: 427–430.
- ↑ Sanjuán P, Julio G, Bolaños J, Álvarez de Toledo J, García de Oteyza G, Temprano J, Barraquer RI. Long-term anatomical and functional outcomes after autokeratoplasty. Br J Ophthalmol. 2021 Aug;105(8):1063-1068. doi: 10.1136/bjophthalmol-2020-316289. Epub 2020 Aug 22. PMID: 32829305.