Asian Blepharoplasty (Double Eyelid Procedure)
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Surgical procedure
Double Eyelid Blepharoplasty CPT 1520-1523
Background
The double eyelid blepharoplasty, often colloquially termed the “Asian blepharoplasty” due to its predominance in the East Asian ethnic population, is a voluntary procedure that aims to provide a supra-tarsal crease to improve cosmetic concerns in affected patients. Anatomical differences in the Asian eyelid anatomy lead to a lack or obscuration of a supratarsal crease. About 50% of people of Asian descent do not have an upper eyelid crease.[1] Although Asian Americans comprise 6% of the cosmetic surgical patient population, the double eyelid procedure is the most frequently requested cosmetic surgery in Asia, and the third most popular cosmetic procedure after rhinoplasty and breast augmentation.[1] Therefore, a thorough understanding of Asian blepharoplasty and the methods of achieving a desirable outcome for the patient and the surgeon is of particular importance.
History
The first reported “double eyelid operation” was done in 1896 by Mikamo.[2] Although this cosmetic procedure is often referred to as an attempt to achieve a more “westernized” look, the earliest description of double eyelid blepharoplasty far preceded the influence of the west on Asian culture. Therefore, Mikamo’s development of the double eyelid surgery is regarded to have been motivated by the desire to achieve a more aesthetic, round eyed, and expressive look.[3]
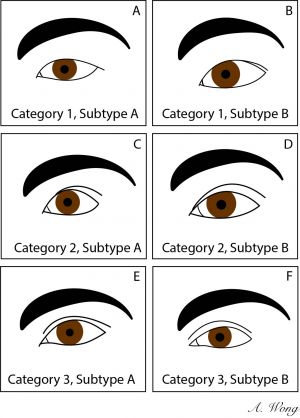
Asian Eyelid Morphologies
Individuals of Asian descent have a broad range of eyelid morphologies. The organization of fat pads, the presence of epicanthal folds, and the arrangement of internal eyelid structures work together to compose unique and characteristic Asian eye shapes. One noticeable difference among Asian eyes that has led to the desire for the double eyelid procedure is the presence or absence of a supratarsal crease. Asian eyelids have been categorized by Kiranantawat et al., into three main categories, each with two respective subcategories. [4]
Category 1 - Single Eyelid Crease
Subtype A - There is a single eyelid with no visible lid crease
Subtype B - There is a low eyelid crease, which is mostly hidden and is tapered toward the nose
Category 2 - Double Eyelid Crease
Subtype A - Infold type: The supratarsal crease height is lower than the epicanthal fold
Subtype B - On fold type: The supratarsal crease height meets or is on the epicanthal fold
Category 3 - Double Eyelid Crease (Outfold types)
Subtype A - Outfold Type 1: The height of the eyelid crease is superior to the epicanthal fold
Subtype B - Outfold Type 2: There is a double eyelid crease, but no epicanthal fold is present
Anatomy of the Asian Eyelid
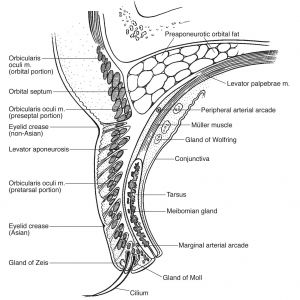
Location of Fusion of the Orbital Septum, Levator Aponeurosis, and Preaponeurotic Fat
The anatomical variance that causes some people to lack a supratarsal crease is due to the different points of fusion between the orbital septum and the levator aponeurosis.[5] In people who possess an eyelid crease, the levator aponeurosis is fused with the orbital septum approximately 8-10 mm above the supra-tarsal border. In people who lack a superior eyelid crease, the levator aponeurosis inserts lower than 8mm above the supra-tarsal border. A lower fusion point allows the preaponeurotic fat pad to extend much lower thus giving the eyelid a much fuller appearance with a tapering crease when the eyelid is opened.[6]
Therefore, a supratarsal crease near the lid margin is created and often appears as a “monolid” or as an obfuscated crease. This is in comparison to individuals with a "double eyelid" where fusion occurs above the supratarsal border. In a study by Jeong, cadaveric Asian eyelids were found to have fusion of the aponeurosis, septum, and tarsal plate approximately 2 mm above the lid margin.[7] In comparison, Caucasian eyes exhibited fusion more superiorly, approximately 3 to 4 mm above the lid margin.[7] Other sources have listed that Caucasian eyes may have fusion as high as 5 to 10mm above the superior tarsal border.[8]
This lower point of fusion also allows for further inferior descent of the fat pad, sometimes extending as far anterior as the tarsal plate. It has been noted that this anterior fat is what often contributes to the “puffy” appearance in some Asian eyes, and may give the illusion of ptosis.[1][4]
Epicanthal Fold
One distinguishing structure that characterizes many Asian eyes is the epicanthal fold. Present in almost all newborns, the epicanthal fold presents with an incidence of 2% in non-Asian adults, and at an incidence as high as 90% in Asian adults.[9] This structure is described as a crescent-shaped portion of skin at the medial aspect of the superior lid that descends along the border of the nose toward the canthus to meet the medial portion of the lower eyelid. The presence of epicanthal folds also leads to a greater intercanthal distance.[10] In 1968, Johnson described and categorized four types of epicanthal folds into the Johnson Classification:[11]
(A) Type I - Epicanthus Supraciliaris
The Epicanthus supraciliaris subtype fold that begins from the brow and travels concavely toward the lacrimal sac. The lacrimal sac and caruncle are often visible.
(B) Type II - Epicanthus Palpebralis
The epicanthus palpebralis subtype originates from the upper lid and extends inferiorly
(C) Type III - Epicanthus Tarsalis
The Epicanthus tarsalis subtype originates from the upper lid crease and terminates to join the skin at the medial canthus. This is the most common type of epicanthal fold found in Asians. The lacrimal lake and caruncle are often covered.
(D) Type IV - Epicanthus Inversus
The Epicanthus Inversus subtype is unique. It differs from the other subtypes in that it originates from the lower eyelid and extends medially and upward
Fat Pads
Fat in Asian eyes is not only present in a greater quantity, but is also distributed differently within the eyelid. Four types of fat pads in Asian eyelids have been described in the literature: subcutaneous, pretarsal, submuscular or preseptal, and orbital or preaponeurotic fat pads.[12] The fat pads that tend to be more prominent in Asian eyelids and contribute to the lack of a supratarsal crease are pretarsal fat and preseptal fat or submuscular fibroadipose tissue (SMFAT). The SMFAT occupies the space between the orbicularis oculi muscle and the orbital septum. It continues superiorly to become the retro orbicularis oculi fat (ROOF).
In a cadaveric study, Jeong compared the anatomical differences between Caucasian and Asian eyelids. With respect to fat content, the study revealed that Asian eyes contain more subcutaneous and suborbicularis fat, with a pretarsal fat component. There was also diffuse fat on the anterior and posterior surfaces of the orbicularis which was not found in the cadaveric caucasian eyelids.[7] It was also found that Asian eyes with a double eyelid have an intermediate fat content between Asian eyes without an eyelid crease and Caucasian eyes. This highlights the relation between fat content in the presence of a double eyelid.
Lack of Skin Attachments
In individuals with a lid crease, the aponeuroses of the levator palpebrae superioris muscle and orbicularis oculi muscle have attachments to the pretarsal and preseptal skin of the upper eyelid. These attachments help to invaginate the lid skin as the eyes open to create an eyelid crease. In some Asian individuals who appear to have no lid crease, there is a scarcity or absence of these fibrous attachments.[1]
Indications
Double eyelid blepharoplasty is a voluntary procedure that is indicated for any patient lacking a supra-tarsal crease that wishes to have a larger, more rounded eye appearance. It is primarily an aesthetic procedure.
Preoperative Evaluation
The preoperative evaluation should place emphasis on ophthalmologic and periorbital health. The patient’s visual acuity, meibomian gland function, lacrimal gland function, and eyelid symmetry should be evaluated. Additionally, ocular surface disorders like dry eye should be assessed. The accompanying ptosis in patients without a crease may be protective against dry eye and creation of a double eyelid may unmask ocular surface disorders.[13]
The following is a checklist of 16 items to consider in the preoperative assessment for the double eyelid procedure. It is adapted from Sukh et al.,[14]
1. Brow and Forehead
Brow ptosis or blepharoptosis may be hidden in individuals by compensatory hyperactivity of the frontalis muscle. Therefore, surgical correction of blepharoptosis will result in relaxation of the frontalis muscle, and the brow will sit at a position more inferior than intended. To predict proper postoperative brow height and assess frontalis hyperactivity and levator function, negate frontalis function with the Berke’s test.
Berke’s Test or Berke’s Method
- While the patient is in downgaze as far as possible, immobilize and hold the patient’s brow
- Ask patient to look upward, effectively negating contribution from the frontalis muscle
- Check the excursion and final position of the lid margin while preventing the brow from rising
2. Upper Eyelid Skin and Fat
Thicker skin and increased fat in the eyelids of Asian individuals contributes to the absence of a supratarsal crease or double eyelid. During evaluation, note the amount of eyelid fat as it may contribute to lateral hooding or a “puffy” eyelid appearance. It is also important to note any upper lid skin laxity that may contribute to Floppy Eyelid Syndrome.
3. Eyelid Crease
Evaluation of the upper eyelid for a crease or multiple smaller creases is beneficial. Presence of multiple smaller creases may be present and indicate brow ptosis or upper eyelid laxity.
When assessing patient desires, it is important to maintain a natural, ethnically appropriate appearance. Although an “On Fold” appearance is suitable for many patients, some patients request a high crease (Category 3: outfold) appearance. Doing so on a patient who does not meet the following criteria will eliminate natural ethnic characteristics of the eye and result in unsatisfactory outcomes.[14] The high crease will only result in a natural appearance if the patient meets the following criteria: lack of an epicanthal fold, more than 30 mm of length of the palpebral fissure, minimal orbital fat, good levator function, thin skin, and more exophthalmic than enophthalmic.[14]
4. Cilia Direction
Note the direction of the eyelashes prior to the double eyelid procedure. The presence of an epicanthal fold encourages downturning of the eyelashes, and plays a part in the increased incidence of trichiasis in Asian individuals. Failure to note the direction of the lashes may result in upturned cilia and exposure of the palpebral conjunctiva. [14]
5. Orbicularis Oculi Muscle
Innervated by the temporal and zygomatic branches of the facial nerve (CN VII), the Orbicularis Oculi Muscle plays a role in appropriate lid closure. Recognizing appropriate function of the orbicularis oculi muscle prior to surgery is important to prevent complications such as scleral show and ectropion.
6. Upper Lid Margin
Similar to assessing brow, evaluation of the upper lid for ptosis, levator function, and hyperfunction of the frontalis muscle are necessary. The patient should also be assessed for unilateral ptosis in the dominant eye. Hyperfunction of the levator muscle usually occurs in the non-dominant eye as a compensatory mechanism, and will affect outcomes of blepharoplasty as the previously ptotic eye will allow for relaxation of the levator muscle over the non-dominant eye.
7. Lower Lid Margin
A natural look is achieved when the lower lid margin meets the inferior corneoscleral junction. Note the position of the lower lid margin and if the patient exhibits reverse ptosis. In patients with an MRD2 below the average of 4.5 to 5.5 mm, the resulting appearance may represent a lateral canthal tilt. If the patient has an MRD2 greater than 5.5 mm, it may appear proptotic or like Grave’s Disease.
8. Palpebral Shape
The palpebral fissure slant angle should be noted: upward, downward or horizontal. Creation of a double eyelid without attention to the palpebral slant may result in creation of an excessively positive or negative slant angle. Asian eyes tend to have a natural upward or positive lateral canthal tilt. Creation of a downward tilt will result in a Treacher-Collins appearance. Patients with positive canthal tilt may be candidates for lateral canthoplasty to lower the lateral canthal position.
9. Palpebral Fissure Length
The average length of the Asian palpebral fissure is between 25 and 28 mm. Length measurements are important because the patient may consider concomitant epicanthoplasty and or lateral canthal lengthening procedure with blepharoplasty if their palpebral fissure length is less than 25 mm. These measurements should always be taken and considered within the context of the patient’s face width and proportions.
10. Palpebral Fissure Width
It is important to consider the ideal palpebral fissure width preoperatively. A guideline is that the palpebral width should be more than 10 mm without ptosis or reverse ptosis and with an MRD1 of 4.5 mm. Asian eyes on average have an average MRD1 of 3 to 3.5 mm.[14] An anatomically accepted landmark of the appropriate palpebral aperture is when the upper lid margin lies at the corneoscleral junction.
11. Epicanthal Fold
Knowledge and documentation of the epicanthal fold type of the patient is necessary to predict the outcome of the double eyelid procedure. The epicanthal folds are categorized in the "Anatomy of the Asian Eyelid" section. A commonly desired outcome of double eyelid procedure with epicanthoplasty is an eyelid morphology where the lacrimal lake is only partially covered, and the epicanthal fold meets the skin at the lacrimal lake margin.
12. Lateral Canthal Web
The lateral canthal web should be measured with calipers from the lateral canthus to the intersection of the bulbar and palpebral conjunctiva. An alternate measurement may be taken with calipers after palpating the medial orbital rim and measuring the length of the lateral canthal web. This measurement will prove helpful to determine if the patient is a candidate for lateral canthal lengthening procedure to achieve the final desired outcome.
13. Lower Lid Muscular Tone and Skin
Lower lid tone and skin laxity should be evaluated with the snap back test and distraction test. If the patient requires a lateral canthal lengthening procedure, there will be induced laxity in the lower lid due to iatrogenic damage to the lateral canthal tendon. Therefore, this should go into consideration of the final appearance before proceeding with surgery.
14. Pretarsal Fullness (Love Band)
A popular aesthetic is to have pretarsal fullness of the lower lid, often known as the love band. The fullness is a result of muscular contractions of the preseptal orbicularis oculi muscle and accumulation of pretarsal fat during a smile.
15. Tear Trough
The tear trough ligament is another consideration as it lies in the proximity of the working space. It lies between the palpebral and orbital portions of the orbicularis oculi muscle.
16. Lower Lid Fat
Asian individuals tend to have more prominent cheekbones which serve as a shelf for lower lid fat. Note the presence of lower lid fat prior to surgery to predict the need for further procedures to maintain the love band while reducing the appearance of bulging fat.
Consideration of Epicanthoplasty
At the preoperative evaluation, it may be appropriate to consider epicanthoplasty in patients with a prominent epicanthal fold. The prominent epicanthal fold may result in an unintended appearance of the double eyelid and prevent the surgeon from achieving the desired eyelid morphology. Therefore, it may be appropriate to consider a concomitant epicanthoplasty with blepharoplasty in these individuals. Another indication for a epicanthoplasty is for patients with epicanthal folds who desire an open or outfold type of eyelid morphology.[13]
Epicanthoplasty Precautions
One noticeable precaution that must be discussed with patients is the possibility of a visible scar in the medial canthal area after epicanthoplasty.[13] Patients who have an intercanthal distance less than 32 mm may be poor candidates for epicanthoplasty. Therefore, preoperative evaluation by stretching the medial canthal skin with tape can help predict the postsurgical outcome of epicanthoplasty with blepharoplasty.[14]
Cultural Considerations in Appearance
Long before Western standards of beauty entered Asia, the “double eyelid” was documented by Japanese surgeon Mikamo in the medical literature.[2] He noted that the double eyelid was present in approximately 18% of Japanese women and determined it was a naturally occurring appearance.[2] Although Asian blepharoplasty was initially intended to create a look that was still within the scope of normal Asian facial anatomy, Western influences eventually played a role in desired outcomes of patients in the following decades. For example, Hata described a higher 10 mm crease and many other authors detailed the excision of muscle and fat to create the appearance of a deeper set eye.[1]
Asian blepharoplasty procedures are continually being modified, but the consensus is that surgeons should consider the patient’s goals and to understand the cultural framework that influences outcome satisfaction. Therefore, during surgical planning for Asian patients, 6 to 8 mm above the lid margin is the generally accepted standard for the height of the eyelid crease. It has been shown that a range of 3 to 10 mm is also aesthetically pleasing.[15][16] Additionally, the creation of an eyelid crease in Asian individuals should parallel the normal curvature of the eyelid margin.
To ensure that the double eyelid procedure does not eradicate an individual of their ethnic identity or characteristic appearance, it is imperative to recognize that the creation of a double eyelid is not synonymous with creating a “western eyelid”. Rather, it is the desire to strike balance when creating an eyelid that is aesthetically pleasing within the context of the patient’s anatomy, culture, and goals.[17]
Surgical Preparation
Whether performing an incisional or non-incisional blepharoplasty, the general preparation in the OR is similar. Pre-operative preparation begins with eyelid marking performed in the upright position to allow visualization of the final gravitational position of the eyelid. This is then assessed in supine position as well. The proposed supra-tarsal crease is drawn at the patient’s desired height, extending from the medial to lateral canthus. Once symmetry of the mark bilaterally is properly assessed in both the upright and supine positions, a sterile preparation can be performed. After this, local anesthetic is applied to the upper eyelids and a corneal shield may be placed. The procedure can be performed with or without IV sedation.[18] The choice of suture material for the procedure is largely based upon surgeon preference as few clinical or animal studies have been performed to evaluate the efficacy of the various suture types in facial surgeries.[19]
Surgical Techniques
The techniques for Asian blepharoplasty or double eyelid procedure can be divided into two categories: the non incisional suture ligation technique or the external incisional surgical technique.
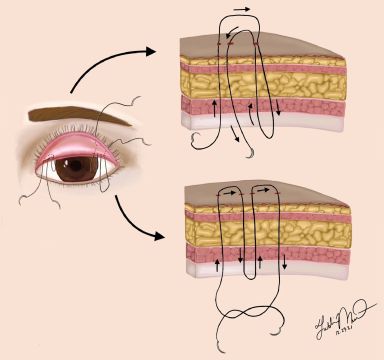
Non-Incisional Suture Ligation Technique
Early medical literature in the late 1890s describes Japanese surgeon Mikamo using a suture ligation technique modified from a surgical procedure intended to correct entropion.[2] His first record of Asian blepharoplasty detailed the use of three sutures, each was 3 mm apart, 6 to 8 mm superior to the lid margin, and removed after 4 to 6 days. The sutures extended through the full thickness of the eyelid to include the tarsus.
Since Mikamo’s time, many modifications have arisen, but the basic principles of the suture ligation technique remain. The underlying concept is to create a supratarsal crease by suture fixating the orbicularis oculi muscle or the subcutaneous tissues to the levator aponeurosis or tarsal plate.[1] This effectively creates a level of attachment more superior than the natural fusion of the levator aponeurosis and orbital septum. Scarring and adhesions postoperatively will further assist with fixation.
Procedural Steps (adapted from Weng[13])
- Prepare and drape the patient in a standard sterile fashion, using 5% povidone-iodine and a sterile drape.
- Find and mark the center of the upper eyelid (6 to 8mm above the lid margin is appropriate for most Asian eyelids).
- Create two marks, one on the medial ⅓ of the eyelid, and one on the lateral ⅓ of the eyelid to split the difference between the center mark made in step 1. Note: the lateral ⅓ mark can be marked 1 to 1.5 mm wider than the central mark to create a curve on the lateral aspect
- Anesthetize the area with local anesthetic
- Create two incisions 1 to 2 mm horizontally through the skin at each of the three marks
- With 6-0 Prolene, pass the suture through all the tissue layers at the incision site. Emerge through the palpebral conjunctiva
- Pass the same suture back through the palpebral conjunctiva in the opposite direction through to the subdermis via a different track
- Tie the suture to bury the knot subcutaneously
- Repeat steps 6 to 8 at each of the incision sites
- The three small incisions are left open to heal
Variation
Another method exists where mattress sutures are utilized in steps 7 and 8. The needle is driven at a distance of 2 to 3 mm apart, and the knot is buried subcutaneously.
Advantages
The suture fixation method is advantageous because it circumvents a visible scar, endorses a shorter operation, reduces postoperative recovery times, and is easier to revise.
Disadvantages
The main disadvantage with this method is the high failure rate. This is largely due to the reliance on few sutures to hold multiple layers of tissue. Over time, the sutures may be loosened by the frequent use of the levator muscle. Cosmetically, there have been reports that suture material can be seen when the patient closes their eyes.[1] Finally, since the procedure is limited to ligation and creation of a double eyelid, it may not be appropriate for patients in need of accompanying procedures like epicanthoplasty or those in need of excess fat, skin, muscle excision.
Modifications
Modifications to fortify the anchor fixation have been attempted. Lee et al., attempted to do so by debulking the pretarsal muscle and fat and septum through stab incisions prior to suture fixation. Among their 327 patients, the eyelid crease persisted at an average follow up time of 13 months with a range of 2 months to 2 years.[20]
A limited incision modification by Yang also involved removal of preaponeurotic fat. The suture ligations involved anchoring the pretarsal skin to the levator aponeurosis with a single suture through incisions 3 to 4 mm in length. Only 3 out of 76 patients experienced loss of the eyelid crease over a follow up period of 3 years.[21]
Megumi performed another limited incision technique through the conjunctiva to debulk fat from the eyelid. He followed this by using a running suture to construct a sling along the length of the eyelid which secured subdermal tissue and conjunctiva at the superior border of the tarsus. In 280 patients, three reported loss of the surgically created eyelid fold.[22]
Additional Non-incisional techniques
Partial thickness suture techniques are also commonly employed.[23] Again, the first bite takes place transcutaneously or transconjunctivally. However, instead of passing through all planes of tissue, the suture is only passed through a portion of the lid and returned to the plane of the original bite. The layer through which the suture passes typically involves either the subcutaneous or orbicularis oculi planes in a transconjunctival approach, or the tarsus in a transcutaneous approach.[24] Continuous and discontinuous methods can be performed in a similar fashion as described above.
Additionally, newer techniques have reported improved outcomes in patients who undergo debulking of pre-tarsal tissues through small stab incisions on the lid prior to the placement of sutures.[25] However, this is not currently common practice. In all non-incisional techniques, the sutures are typically removed within 4-7 days.
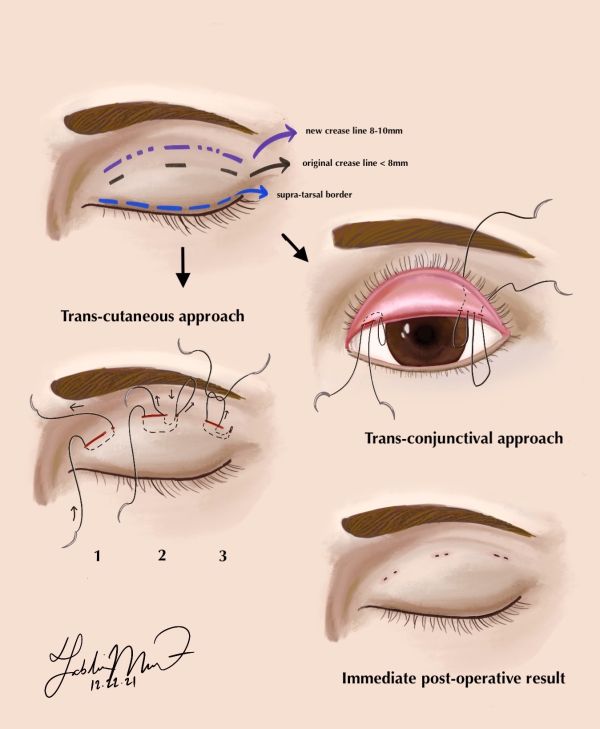
External Incisional Technique
The suture ligation technique remained the only method to create a supratarsal crease until the 1920s, when Maruo documented the first external incision technique. His technique involved creating an incision on the upper eyelid 7 mm from the ciliary margin. This was closed by passing suture through the lid from the conjunctiva to the superior tarsal border of the anterior skin edge to the tarsal plate.[26] Today, like the suture ligation technique, the surgical resection technique has been refined.
Procedural Steps (adapted from Weng[13])
- Prep and drape the patient in a standard sterile fashion, using 5% povidone-iodine and a sterile drape.
- Mark the center of the eyelid at 6 to 8 mm superior to the lid margin for Asian eyes
- Mark two lines horizontally across the eyelid
- The first line demarcates the location of the new eyelid crease on the upper eyelid at the distance from the lid margin determined in Step 1. The line should be drawn after redundant eyelid skin is pulled upward by the brow with one finger. The eyelashes should not be everted while exposing redundant skin. This line should gently curve downward with the medial tip reaching under the natural epicanthal fold
- The second line should be drawn superiorly to the first line and demarcates the amount of redundant skin to be excised. The appropriate amount can be determined with a pair of forceps
- The lines should then be connected at the lateral ends and medial ends
- Inject Lidocaine with 1:200,000 epinephrine into the subcutaneous space beginning at the lateral aspect of the upper eyelid
- Excise the skin marked between the drawn lines with curved Stevens scissors, exposing the orbital septum
- Inject local anesthetic into the septal space to assist with dissection into the space without causing iatrogenic damage to the levator aponeurosis
- Begin to open the orbital septum, traveling laterally to medially. The distal aspect of the levator aponeurosis should be visible, inserting onto the tarsal plate
- At this stage, excision of orbital fat may be performed. ROOF may be removed at the lateral third of the eyelid
- Using 6-0 clear Prolene, take a bite of the levator aponeurosis and pass the suture through the inferior edge of the orbicularis oculi muscle.
- Tie this suture down and evaluate the location of the new supratarsal fold by asking the patient to open his or her eyes
- Continue with 3 or 4 stitches with 6-0 Prolene to complete attachment of the levator aponeurosis and orbicularis oculi. Ensure there is enough tension to create slight eversion of the eyelids for an optimal result
- Close the incision with 6-0 silk suture in a running fashion
Advantages
The surgical incision technique is advantageous in many aspects. The eyelid structures are surgically fixated rather than reliance on scar formation and adhesion of tissues in the suture ligation method above. Additionally, it offers the chance to excise excess fat or tissue and perform concomitant procedures like an epicanthoplasty.
Disadvantages
Disadvantages of this method arise from the increased risk of iatrogenic injury to surrounding structures, especially when dissecting into the septal space. The procedural time and postoperative recovery times are also increased.
Alternative Treatment Methods
Among the general public, alternative treatments in the form of double-sided tape or liquid glue is a common nonsurgical option for patients wishing to achieve a double eyelid effect. Utilizing these methods creates an impermanent fold by attaching to the eyelid skin, as the tape or glue can be removed. Although individual products vary, the concept is similar. Double eyelid tape is a thin, clear strip that is placed roughly 4 to 6 mm above the upper eyelid margin. The eyelid is cleaned before a Y-shaped applicator is used to push the upper eyelids up to secure the adhesive and create a fold in the desired area.
Disadvantages
These nonsurgical treatment options have raised questions about their detrimental effects on ocular health and comfort. In a four-week study of 26 Chinese females without previous history of ocular diseases and a supratarsal crease, it was reported that use of double-sided eyelid tape significantly decreased the occurrence of complete blinking due to the physical prevention of eyelid closure.[27] This adverse result was shown to lead to other complications, such as increased tear evaporation, meibomian gland dysfunction (MGD), conjunctival staining, and corneal staining. Effects of the tape can be worsened or expedited if used along with other eye cosmetics such as mascara and eyeliner.
While full-incision blepharoplasty is a more invasive and expensive alternative, dry eye symptoms tend to disappear three months after surgery. This raises concern over the overall benefit of using eyelid tape, as the anterior ocular health of individuals may be jeopardized at the expense of temporarily meeting standards of beauty. Patients and physicians must be aware of the risks of using double eyelid tape over an extended period of time.
Post-Operative Care
Post-operative, daily wound care and antibiotic ointment is recommended. It is highly advised that patient’s avoid strenuous activity or submerging wound site in water. The patient should follow up for suture removal in 5-7 days, with follow up for preliminary results typically around two weeks.[6]
Postoperative Complications
Asymmetric and Excessively High Folds
Eyelids with uneven height or shape are the most common complication, with occurrence rates as high as 35%.[28][29][30] Differences in preoperative marking, discrepancies in amount of skin excised, unequal tension on skin during supratarsal fixation, and unequal amounts of fat excision are some causes of asymmetric eyelid folds.
Around 7% of patients present with excessively high folds postoperatively.[1] The folds are considered too far superior if they exist above the superior border of the tarsal plate. Mentioned previously, the ideal location of the eyelid crease is 6 to 8mm above the lid margin. This unnatural appearance can be caused by adhesions between the orbicularis and the skin above the level of surgical fixation. High folds can also be the result of overly aggressive resection of preaponeurotic fat pads.
Blepharoptosis
The appearance of a drooping eyelid after Asian blepharoplasty can be caused by iatrogenic damage to the levator palpebrae superioris muscle and its aponeurosis. Unintentional separation of the levator from the tarsal plate and scarring from excessively high fixation of the aponeurosis to muscle disrupts appropriate function of the levator.
Bleeding
As with any procedure, bleeding is a potential risk that can range from prolonged ecchymosis to massive hematoma. The rates of bleeding are similar to those for blepharoplasty across all ethnicities.[31]
Weakening of Sutures
With time, some patients may experience recurrence of skin laxity and elimination of the surgically created upper eyelid crease. However, this is present in less than 3% of cases and occurs more often with the suture ligation technique and if absorbable suture is used. This is due to weakening of the anchoring suture and failure of adhesion between the levator and muscle or dermis.[32] Prevention of this complication can be achieved via debulking of orbital fat or purposeful suturing to fortify the levator-dermal junction and the tarso-dermal junction during creation of supratarsal crease.[14]
Upturned Cilia
The presence of an epicanthal fold encourages downturned eyelashes, which is reflected in the increased incidence of trichiasis in Asian individuals. Creation of a double eyelid can alleviate and assist with eversion of the cilia. However, if proper preoperative planning and care during surgery is not taken, the upper lid eyelashes can evert and expose the palpebral conjunctiva.
Ocular Surface Disease
As mentioned in the preoperative evaluation section, creation of a double eyelid may create or exacerbate mild dry eye symptoms. The ptosis which sometimes accompanies individuals without an eyelid crease may be protective against the development of dry eye. Therefore, it is important in the preoperative period to assess the patient for development of these complications.
Ectropion
Injury to the zygomatic or recurrent buccal branches of the facial nerve during surgery may impede proper function of the orbicularis oculi muscle. This can not only alter the position of the lower lid margin, but create complications such as ectropion. Ectropion will also occur if the tension of the eyelid levator is higher than is what is allowed by normal skin. This is due to the misplacement of the inferior incision or inferior skin flap on the levator.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Nguyen MQ, Hsu PW, Dinh TA. Asian blepharoplasty. Semin Plast Surg. 2009 Aug;23(3):185-97. doi: 10.1055/s-0029-1224798. PMID: 20676313; PMCID: PMC2884917.
- ↑ 2.0 2.1 2.2 2.3 Mikamo M. Plastic operation of the eyelid. J Chugaiijishimpo. 1896;17:1197.
- ↑ Fakhro A, Yim HW, Kim YK, Nguyen AH. The Evolution of Looks and Expectations of Asian Eyelid and Eye Appearance. Semin Plast Surg. 2015;29(3):135-144. doi:10.1055/s-0035-1556847
- ↑ 4.0 4.1 Kiranantawat K, Suhk JH, Nguyen AH. The Asian Eyelid: Relevant Anatomy. Semin Plast Surg. 2015;29(3):158-164. doi:10.1055/s-0035-1556852
- ↑ Doxanas MT, Anderson RL. Oriental eyelids. An anatomic study. Arch Ophthalmol. 1984;102(8):1232-1235. doi:10.1001/archopht.1984.01040031002036
- ↑ 6.0 6.1 Fagien, S. (2008). Putterman's cosmetic oculoplastic surgery. Saunders Elsevier.
- ↑ 7.0 7.1 7.2 Jeong S, Lemke BN, Dortzbach RK, Park YG, Kang HK. The Asian upper eyelid: an anatomical study with comparison to the Caucasian eyelid. Arch Ophthalmol. 1999 Jul;117(7):907-12. doi: 10.1001/archopht.117.7.907. PMID: 10408455.
- ↑ Anderson RL, Beard C. The levator aponeurosis. Attachments and their clinical significance. Arch Ophthalmol.1977 Aug;95(8):1437-41. doi: 10.1001/archopht.1977.04450080147019. PMID: 889520.
- ↑ McCurdy JA Jr. Beautiful eyes: characteristics and application to aesthetic surgery. Facial Plast Surg. 2006 Aug;22(3):204-14. doi: 10.1055/s-2006-950179. PMID: 17048162.
- ↑ Wu XS, Jian XC, He ZJ, Gao X, Li Y, Zhong X. Investigation of anthropometric measurements of anatomic structures of orbital soft tissue in 102 young han chinese adults. Ophthalmic Plast Reconstr Surg. 2010 Sep-Oct;26(5):339-43. doi: 10.1097/IOP.0b013e3181c94e97. PMID: 20592637.
- ↑ Johnson CC. Epicanthus. Am J Ophthalmol. 1968 Nov;66(5):939-46. doi: 10.1016/0002-9394(68)92817-1. PMID: 4234938.
- ↑ Uchida J. A surgical procedure for blepharoptosis vera and for pseudo-blepharoptosis orientalis. Br J Plast Surg. 1962 Jul;15:271-6. doi: 10.1016/s0007-1226(62)80041-1. PMID: 13923412.
- ↑ 13.0 13.1 13.2 13.3 13.4 Weng CJ. Oriental upper blepharoplasty. Semin Plast Surg. 2009;23(1):5-15. doi:10.1055/s-0028-1110096
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 14.6 Suhk JH, Kiranantawat K, Nguyen AH. Physical Evaluation of the Asian Blepharoplasty Patient. Semin Plast Surg. 2015 Aug;29(3):145-57. doi: 10.1055/s-0035-1556851. PMID: 26306081; PMCID: PMC4536068.
- ↑ Boo-Chai K. Plastic construction of the superior palpebral fold. Plast Reconstr Surg. 1963 Jan;31:74-8. doi: 10.1097/00006534-196301000-00010. PMID: 13968908.
- ↑ Mutou Y, Mutou H. Intradermal double eyelid operation and its follow-up results. Br J Plast Surg. 1972 Jul;25(3):285-91. doi: 10.1016/s0007-1226(72)80065-1. PMID: 4558502.
- ↑ Motaparthi K. Blepharoplasty in asian patients-ethnic and ethical implications. Virtual Mentor. 2010 Dec 1;12(12):946-9. doi: 10.1001/virtualmentor.2010.12.12.msoc1-1012. PMID: 23186822.
- ↑ Lee CK, Ahn ST, Kim N. Asian upper lid blepharoplasty surgery. Clin Plast Surg. 2013;40(1):167-178. doi:10.1016/j.cps.2012.07.004
- ↑ Joshi AS, Janjanin S, Tanna N, Geist C, Lindsey WH. Does suture material and technique really matter? Lessons learned from 800 consecutive blepharoplasties [published correction appears in Laryngoscope. 2007 Aug;117(8):1510. Lindsey, Charlie [corrected to Lindsey, William H]]. Laryngoscope. 2007;117(6):981-984. doi:10.1097/MLG.0b013e31804f54bd
- ↑ Lee YJ, Baek RM, Chung WJ. Nonincisional blepharoplasty using the debulking method. Aesthetic Plast Surg. 2003 Nov-Dec;27(6):434-7. doi: 10.1007/s00266-003-3096-9. Epub 2004 Mar 4. PMID: 14994171.
- ↑ Yang SY. Oriental double eyelid: a limited-incision technique. Ann Plast Surg. 2001 Apr;46(4):364-8. doi: 10.1097/00000637-200104000-00002. PMID: 11324876.
- ↑ Megumi Y. Double eyelid procedure by removal of transconjunctival orbital fat and buried sutures combined with sling technique to avoid wounding the eyelid. Aesthetic Plast Surg. 1997 Jul-Aug;21(4):254-7. doi: 10.1007/s002669900120. PMID: 9263547.
- ↑ Song RY, Song YG. Double eyelid operations. Aesthetic Plast Surg. 1985;9(3):173-180. doi:10.1007/BF01570847
- ↑ Bae KH, Baek JS, Jang JW. Nonincisional Blepharoplasty for Asians. Facial Plast Surg Clin North Am. 2021;29(4):523-532. doi:10.1016/j.fsc.2021.06.005
- ↑ Nguyen MQ, Hsu PW, Dinh TA. Asian blepharoplasty. Semin Plast Surg. 2009;23(3):185-197. doi:10.1055/s-0029-1224798
- ↑ Maruo, M. "Plastic construction of a ‘double eyelid’." Jpn Rev Clin Ophthalmol. 1929:393-406.
- ↑ Yong PT, Arif N, Sharanjeet-Kaur S, Hairol MI. Double Eyelid Tape Wear Affects Anterior Ocular Health among Young Adult Women with Single Eyelids. Int J Environ Res Public Health. 2020 Oct 22;17(21):7701. doi: 10.3390/ijerph17217701. PMID: 33105550; PMCID: PMC7672649.
- ↑ Kikkawa DO, Kim JW. Asian blepharoplasty. Int Ophthalmol Clin. 1997 Summer;37(3):193-204. doi: 10.1097/00004397-199703730-00014. PMID: 9279651.
- ↑ Chen SH, Mardini S, Chen HC, Chen LM, Cheng MH, Chen YR, Wei FC, Weng CJ. Strategies for a successful corrective Asian blepharoplasty after previously failed revisions. Plast Reconstr Surg. 2004 Oct;114(5):1270-7; discussion 1278-9. doi: 10.1097/01.prs.0000135951.55118.59. PMID: 15457048.
- ↑ Weng CJ, Noordhoff MS. Complications of Oriental blepharoplasty. Plast Reconstr Surg. 1989 Apr;83(4):622-8. doi: 10.1097/00006534-198904000-00005. PMID: 2928401.
- ↑ Fernandez LR. Double eyelid operation in the Oriental in Hawaii. Plast Reconstr Surg Transplant Bull. 1960 Mar;25:257-64. doi: 10.1097/00006534-196003000-00007. PMID: 13822307.
- ↑ Kim YW, Park HJ, Kim S. Secondary correction of unsatisfactory blepharoplasty: removing multilaminated septal structures and grafting of preaponeurotic fat. Plast Reconstr Surg. 2000 Nov;106(6):1399-404; discussion 1405-6. doi: 10.1097/00006534-200011000-00030. PMID: 11083574.