Arcus Senilis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
This article summarizes the clinical entity known as Arcus Senilis, a ring like opacity by the corneal limbus formed from lipid deposition. It can be associated with hyperlipidemia and several other risk factors, but overall has a good prognosis with little to no effect on visual acuity and ocular health.
Disease Entity
Disease
Arcus senilis (AS), also known as gerontoxon, arcus lipoides, arcus cornae, or corneal arcus, is a deposition of lipid in the peripheral corneal stroma. It is the most common peripheral corneal opacity. It frequently occurs with hyperlipidemia, especially in elderly individuals, and may be associated with dyslipidemia in younger patients (termed arcus juvenilis).[1]
Etiology
This is not entirely known, but it has been linked to hyperlipidemia and dyslipidemia.
Risk Factors
AS is associated with older age, male gender, smoking, systolic hypertension[2][3], African American heritage[4], and increased fasting serum triglyceride[5][6]. Due to its association with hyperlipidemia, AS is particularly common in people with familial hypercholesterolemia and xanthelasma[1][7][8][9].
Despite the risk factors of hyperlipidemia and dyslipidemia, there have been conflicting studies with regards to the association of AS with cardiovascular disease (CVD). In a population-based cross-sectional study in 2011 of 3397 ethnic Indians aged 40 to 80 in Singapore, presence of AS was associated with CVD (OR, 1.31; 95% CI, 1.02 to 1.7; P = .0038) independent of the risk factors in the paragraph above[3]. However, a prospective cohort study of 12,745 Danes followed up for a mean of 22 years found that AS had no clinical value as a predictor of CVD.[10] In a third study of white men (n = 3,930) and women non-hormone users (n = 2,139), ages 30-69, followed for an average of 8.4 years as part of the Lipid Research Clinics Mortality Follow-up Study, AS was associated with CHD (RR, 3.7; 95% CI, 0.9 to 14.7) and CVD mortality (RR, 4.0; 95% CI, 1.2 to 12.9) only in hyperlipidemic men ages 30-49 years[11].
Pathophysiology
AS is due to a deposition of lipid in the peripheral cornea and is generally considered a normal aging process. It is believed that increased permeability of limbal vessels with age allows for low-density lipoproteins to pass through the cornea, which may explain why it is found in > 70% of patients over the age of 60[4][5]. Arcus generally initially begins in the superior and inferior regions of the cornea, which have greater perfusion than the central cornea. [12]Tissue necrosis and atrophy are not present with this anomaly[13]. There is no increase in cellularity, fragmentation of the laminae, phagocytosis, unusual vascularity, nor any difference in lipogenesis on histological examination[4].
Unilateral arcus senilis has been associated with ocular hypotony, carotid artery stenosis, cranial autonomic dysregulation, or asymmetric cranial vascular supply [14][15].
The lipid in AS is found to be concentrated mainly in two layers of the peripheral cornea: Descemet's membrane and Bowman's layer, with more deposition in the former[4][13]. Lipid deposition may not only be confined to the cornea but also found in the ciliary body, ciliary processes, and iris as well[16].
Diagnosis
AS is a clinical diagnosis. There are no lab tests or imaging to be performed to determine a diagnosis. However a lipid panel can help identify aforementioned risk factors.
Physical Examination
Stromal lipid initially deposits in the superior and inferior perilimbal cornea, progressing circumferentially to form a mat-white or yellow-white band about 1 mm wide. The band is usually wider in the vertical than the horizontal meridian. The central border is diffuse and the peripheral edge is sharp and separated from the limbus by a clear interval that may undergo mild thinning[1].
Rarely, AS may contain scintillating crystals or “crystalloid” edges which are characteristic of many lipid keratopathies. Though, these opacities are not regularly fluorescent on exam[4].
Certain changes in the biomechanical properties of the cornea have been noted to be different when AS is present. One study found that corneal hysteresis and corneal resistance factor values of eyes with AS were lower when compared with age-matched controls, but there were no differences in other parameters, such as IOP, central corneal thickness, spherical equivalent value of the refractive error, axial length measurements, and mean keratometry[17].
Signs
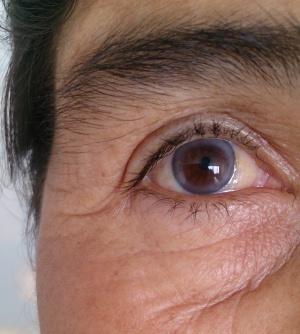
Family members or friends may note a whitish or bluish looking ring-like opacity in the peripheral cornea by the limbus.
Symptoms
AS is usually an incidental finding on exam, as the ring itself is beyond the visual axis and therefore usually asymptomatic.
Clinical diagnosis
This is done at the slit lamp. A whitish yellow band is noted first in the superior and inferior perilimbal cornea, progressing circumferentially to form a mat-white or yellow-white band about 1 mm wide.
Diagnostic procedures
Gross examination or a slit lamp examination are all that is needed to diagnosis AS. A study looking at corneal densitometry and systemic lipid levels on patients with arcus; there was a correlation found between high trigylceride levels and densitometry in the outer most zone of the cornea. [18]
Laboratory test
Lab abnormalities associated with AS include elevated fasting serum triglyceride levels, total cholesterol, and low density lipoprotein[19][20]. Unilateral disease may warrant a work up for carotid vascular disease.
Differential diagnosis
Pseudogerontoxon can develop in recurrent limbal disease. It is characterized by a peri-limbal band of superficial scarring adjacent to a previously inflamed segment of the limbus resembling AS. An example of this is a mild superior pannus which may be seen in long-standing superior limbic keratoconjunctivitis[1]. The fine yellow-white refractile stromal opacities of Terrien marginal degeneration may resemble AS[1]. Ocular manifestations of osteogenesis imperfecta include blue sclera, megalocornea, and corneal arcus[1].
Management
Patients can be followed at yearly intervals as would be expected for follow up in a patient with a normal eye exam. There is no specific management necessary. Prominent AS is often associated with decreased clarity on surgical view, as are other stromal opacities.
Medical follow up
Regular follow up exams as indicated for any patient.
Prognosis
Prognosis is generally good in terms of vision and ocular health.
Additional Resources
- Turbert D, Mendoza O. Arcus Senilis. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/diseases/arcus-senilis-list. Accessed November 17, 2022.
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 1.5 Kanski, J. J. & Bowling, B. Clinical Ophthalmology: A Systematic Approach. (Elsevier Health Sciences, 2011).
- ↑ Hashemi, H., Khabazkhoob, M., Emamian, M. H., Shariati, M. & Fotouhi, A. A population-based study of corneal arcus and its risk factors in Iran. Ophthalmic Epidemiol. 21, 339–344 (2014).
- ↑ Jump up to: 3.0 3.1 Ang, M. et al. Corneal Arcus is a Sign of Cardiovascular Disease, Even in Low-Risk Persons. Am. J. Ophthalmol. 152, 864–871.e1 (2011).
- ↑ Jump up to: 4.0 4.1 4.2 4.3 4.4 Patterson, L. Arcus senilis. Am. J. Forensic Med. Pathol. 3, 115–118 (1982).
- ↑ Jump up to: 5.0 5.1 Raj, K. M., Reddy, P. A. S. & Kumar, V. C. Significance of corneal arcus. J. Pharm. Bioallied Sci. 7, S14–5 (2015).
- ↑ Finley, J. K., Berkowitz, D. & Croll, M. N. The physiological significance of gerontoxon. Arch. Ophthalmol. 66, 211–213 (1961).
- ↑ Forsius, H. Arcus senilis corneae; its clinical development and relationship to serum lipids, proteins and lipoproteins. Acta Ophthalmol. Suppl. 42, 1–78 (1954).
- ↑ Rodstein, M. & Zeman, F. D. ARCUS SENILIS AND ARTERIOSCLEROSIS IN THE AGED. Am. J. Med. Sci. 245, 104–111 (1963).
- ↑ Winder, A. F. Factors influencing the variable expression of xanthelasmata and corneal arcus in familial hypercholesterolaemia. Birth Defects Orig. Artic. Ser. 18, 449–462 (1982).
- ↑ Chambless, L. E. et al. The association of corneal arcus with coronary heart disease and cardiovascular disease mortality in the Lipid Research Clinics Mortality Follow-up Study. Am. J. Public Health 80, 1200–1204 (1990).
- ↑ Walton, K. W. & Dunkerley, D. J. Studies on the pathogenesis of corneal arcus formation II. Immunofluorescent studies on lipid deposition in the eye of the lipid-fed rabbit. J. Pathol. 114, 217–229 (1974).
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK554370/#article-17807.s2
- ↑ Jump up to: 13.0 13.1 Walton, K. W. & Dunkerley, D. J. Studies on the pathogenesis of corneal arcus formation II. Immunofluorescent studies on lipid deposition in the eye of the lipid-fed rabbit. J. Pathol. 114, 217–229 (1974).
- ↑ Naumann GO, Küchle M. Unilateral corneal arcus lipoides. Lancet. 1993 Nov 6;342(8880):1185. PubMed PMID: 7901520.
- ↑ Dysli M, Abegg M, Kerkeni H, Kalla R, Tappeiner C. Unilateral corneal arcus and conjunctival vessel alterations in cranial autonomic dysregulation: A case report. Eur J Ophthalmol. 2023 Sep;33(5):NP91-NP94. doi: 10.1177/11206721221136426. Epub 2022 Nov 3. PMID: 36325686.
- ↑ Walton, K. W. & Dunkerley, D. J. Studies on the pathogenesis of corneal arcus formation II. Immunofluorescent studies on lipid deposition in the eye of the lipid-fed rabbit. J. Pathol. 114, 217–229 (1974).
- ↑ Ayhan, Z., Ozturk, T., Kaya, M., Arikan, G. & Gunenc, U. Corneal Biomechanical Properties in Patients With Arcus Senilis. Cornea 35, 980–982 (2016).
- ↑ Yilmaz YC, Ipek SC, Ozer MD, Celebi T. Corneal densitometry in patients with arcus senilis and its correlation with serum lipid levels. Indian J Ophthalmol. 2022 May;70(5):1556-1563. doi: 10.4103/ijo.IJO_2696_21. PMID: 35502026; PMCID: PMC9332968.
- ↑ Wu, R., Wang, J. J., Tai, E. S. & Wong, T. Y. Cardiovascular risk factors, inflammation, and corneal arcus: the singapore malay eye study. Am. J. Ophthalmol. 150, 581–587.e1 (2010).
- ↑ Macchiaiolo, M. et al. Corneal arcus as first sign of familial hypercholesterolemia. J. Pediatr. 164, 670 (2014).

