Approach to Generalized Eyelid Edema
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Generalized lid edema can be a diagnostic challenge to most of us in our daily clinical practice. Aetiology of lid edema can be due to trivial local conditions like a hordeolum, but sometimes it can be the herald of significant systemic diseases or neoplastic conditions. Causes of lid edema can be vision threatening or even life threating, which needs a systematic approach to reach the diagnosis and prompt treatment
Various etiologies of lid edema are given below.
•Infective •Inflammatory •Allergic/anaphylactic •Vascular •Neoplastic •Trauma •Age related •Systemic causes •Miscellaneous
Infectious causes
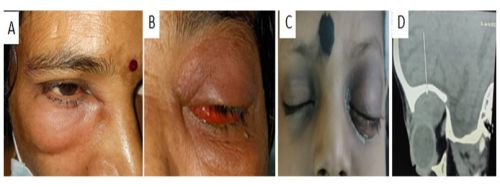
Preseptal cellulitis
Preseptal cellulitis is an inflammation of the tissues anterior to the orbital septum[1]. Clinically, it presents as a rapidly progressive eyelid oedema and erythema with or without conjunctival congestion and chemosis, pain, sometimes a low grade fever also. Seen commonly in children. It is usually caused by contiguous spread of infection from local facial or eyelid injuries, insect etc. Orbital imaging is indicated in patients with suspected orbital cellulitis or patients with worsening of symptoms despite continued systemic antibiotic treatment.
Orbital Cellulitis
Orbital Cellulitis is an infection of the soft tissue of the orbit posterior to the orbital septum. Orbital spread of preseptal infection is associated with onset of proptosis and restriction of ocular movements. Afferent pupillary defect and other signs of optic nerve involvement may be present as well in severe cases. Predisposing factors are sinusitis, trauma with orbital foreign body inoculation, dental abscess, dacryocystitis and systemic conditions like diabetes mellitus, etc. [2]. Orbital cellulitis is an ophthalmic emergency, and management needs imaging, hospitalization and treatment with intravenous antibiotics with close monitoring to identify and treat any complication at the earliest. The clinical spectrum of the orbital cellulitis associated with sinusitis have been demonstrated by Chandler [3], includes preseptal cellulitis, orbital cellulitis, subperiosteal abscess, orbital abscess and cavernous sinus thrombosis.
Lid abscess
Lid abscess is a localized collection of pus, common cause can be extension of infection from sinuses. This needs incision and drainage of the collected pus and oral antibiotics.
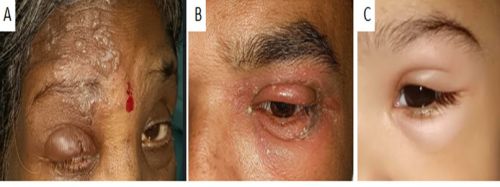
Herpes Zoster Ophthalmicus
Herpes Zoster Ophthalmicus occurs after reactivation of latent varicella-zoster virus characterized by a unilateral painful vesicle in one or more dermatome distributions of the fifth cranial nerve (trigeminal nerve), shared by the eye and ocular adnexa[4].
Erysipelas
Erysipelas caused by beta-haemolytic streptococcus, less often with Staphylococcus [5]. It is the infection of the superficial layer of the skin (upper dermis), characterized by a raised, well-defined, tender, bright red rash, typically on the face or legs, but which can occur anywhere on the skin.
Blister beetle dermatitis
lid edema with vesicles and pustules arising on an intensely inflamed skin, caused by inadvertent skin contact with insects of the genus Paederus, leading to irritant contact dermatitis. Usually vesicles arise towards the centre of the affected area, frequently progressing to pustules[6].
Other infectious causes
Generalized lid edema can be seen in patients with conjunctivitis, hordeolum, dacryoadenitis. Always ask for history of insect bite and look for bite marks.
Inflammatory causes
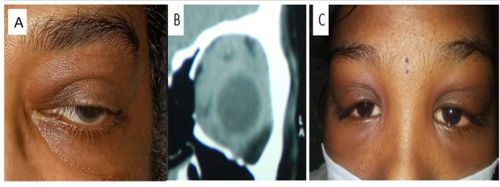
Idiopathic Orbital Inflammation (previously known as Pseudotumor of the Orbit)
Heterogenous group of disorders characterized by orbital inflammation without any identifiable local or systemic causes. Typically characterized by the abrupt onset of proptosis, pain and other orbital inflammatory signs such as swelling and erythema. Unilateral presentation is more typical but paediatric IOI is more commonly characterized by bilateral manifestation, uveitis and disc edema. Other features are diplopia, periorbital edema, EOM restriction, chemosis, decrease vision and ptosis. Orbital inflammation can be secondary to specific systemic diseases such as sarcoidosis, granulomatosis with polyangiitis, Sjögren syndrome, IgG4–related disease (IgG4-RD), lymphoproliferative and histiocytic disorders, xanthogranulomatous disease, or metastatic disease [7].
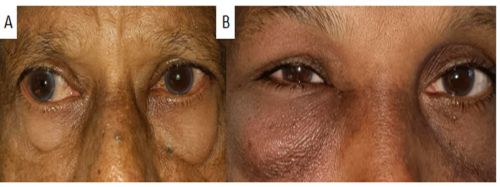
Blepharochalasis:
Episodic inflammation of the eyelids, typically affects the upper eyelids and usually occurs bilaterally. [8] Stages of blepharochalasis syndrome including an active intumescent phase during which attacks of non-pitting edema will occur, and a subsequent atrophic, quiescent phase characterized by the absence of attacks for two years and paper-thin, baggy eyelid skin with a Cigarette paper" appearance have been described. Systemic or topical steroids, antihistamines and other anti-inflammatory agents have not been shown to play a role in acute attacks or in the overall disease course. Surgical interventions are recommended during the quiescent stage, aimed at correcting the complications of blepharochalasis, most commonly ptosis and eyelid skin laxity.
Dacryoadenitis
Dacryoadenitis the inflammation of the lacrimal gland, either the main or the accessory lacrimal gland. It may result from mainly viral infections, also be of bacterial and rarely fungal and parasitic aetiology. It can be due to autoimmune disorders also. Symptoms of dacryoadenitis include pain in the superolateral orbit, pain on eye movements, droopy upper eyelid mainly lateral, redness etc. In case of bilateral and recurrent dacryoadenitis, screen for autoimmune disorders like sarcoidosis, Wegener's granulomatosis, grave's disease, sjogren's syndrome, granulomatosis with polyangiitis.
Allergic/anaphylactic edema
Acute allergic edema
Acute allergic edema occurs on exposure to various allergens. Characterized by painless edema, this process can be associated with chemosis.
Contact dermatitis
It is a type IV hypersensitivity response may be induced by a variety of allergens, including ingredients commonly found in eye makeup and perfumes. Clinical features are periocular oedema, excoriations, scaling, fissuring, papillary conjunctivitis etc. Treatment includes avoidance of allergens, topical and systemic anti histamine agents and corticosteroids.
Angioedema
It is an unpredictable edematous episode of cutaneous and mucosal tissues. It can be hereditary, drug induced or as an allergic reaction to various allergens. It should be considered as a medical emergency as it may cause life threatening respiratory distress.
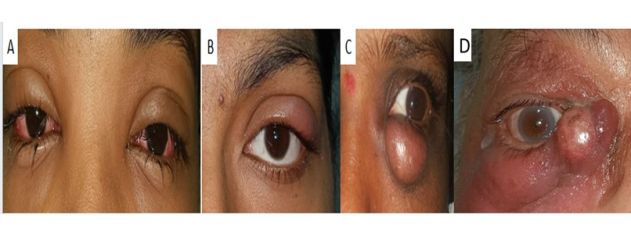
Vascular causes
Vascular lesions of orbit and adnexa like veno-lymphatic malformation, capillary hemangioma, artero-venous malformations can present with a diffuse lid swelling with a bluish tinge. Look for pulsations, variation in size with valsalva maneuver, reducibility, compressibility etc.
Neoplastic causes
Sometimes lid can masquerade of underlying malignant conditions like lymphoma or any adnexal tumors. Look for feeder vessels, salmon patch appearance, necrosis and ulceration. Always make a habit of checking for enlargement of lymph nodes. Traumatic causes Take a detailed history regarding the mode of injury. Trauma can cause lid edema due to soft tissue selling, subcutaneous emphysema, hematoma, retrobulbar hemorrhage etc.
Aged patients can present with a boggy lid due to dermatochalasis, or prolapse of orbital fat due to weakening of the connective tissue and loss of skin elasticity. Dermatochalasis is the presence of loose and redundant eyelid skin. More common in upper lid, but can also affect lower eyelids as well. Weakening of the orbital septum and herniation of the orbital fat adds to the bulging appearance, known as steatoblepharon.
Systemic causes:
Lid edema can be a manifestation of systemic diseases like renal disease, congestive cardiac failure, myxoedema, obstruction of superior vena cava, Fabry's disease, drug induced etc. In case of renal diseases, lid edema usually increases during morning hours. Eyelid lagophthalmos, retraction, temporal flare, and various lid signs of thyroid eye disease are seen in thyroid eye disease.
Miscellaneous causes
Lid edema can be due to dependent collection of fluid in bedridden patients as a part of inflammatory reaction in the forehead or scalp. Sometimes eye ball itself can protrude and present as lid edema ass in the case of microphthalmos with cyst.
References
1. Duke-Elder S, MacFaul PA. System of Ophthalmology. Vol. XIII, Part 2: The Ocular Adnexa: Lacrimal, Orbital and Para-Orbital Diseases. St Louis: CV Mosby, 1974; 859-89.
2. Basic and Clinical Science Course 2019-2020: Oculofacial Plastic and Orbital Surgery. San Francisco, CA: American Academy of Ophthalmology; 2019.
3. Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970;80:1414
4. Liesegang TJ. Herpes Zoster Ophthalmicus. Ophthalmology 2008;115:S3-S12.
5. BELLOWS J. OCULAR COMPLICATIONS OF ERYSIPELAS. Arch Ophthalmol. 1934;11(4):678–683. doi:10.1001/archopht.1934.0083011009601
6. Tamilselvan B, Shanmugam S, Shakthi P. A Case Series of Paederus Dermatitis: Understanding Its Varied and Diverse Clinical Presentations. Cureus. 2024 Feb 13;16(2):e54148. doi: 10.7759/cureus.54148. PMID: 38496106; PMCID: PMC10942126.
7. Mombaerts I, Bilyk JR, Rose GE, McNab AA, Fay A, Dolman PJ, Allen RC, Devoto MH, Harris GJ; Expert Panel of the Orbital Society. Consensus on Diagnostic Criteria of Idiopathic Orbital Inflammation Using a Modified Delphi Approach. JAMA Ophthalmol. 2017 Jul 1;135(7):769-776. doi: 10.1001/jamaophthalmol.2017.1581. PMID: 28570731; PMCID: PMC5710199.
8. rtiz-Perez S, Patel BC. Blepharochalasis Syndrome. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560620/Add text here