Anterograde (Wallerian) or Retrograde Degeneration in the Optic Pathway
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Process
Wallerian degeneration is a phenomenon that occurs when nerve fiber axons are damaged. The axon then undergoes a degeneration process that can be anterograde or orthograde (Wallerian) [1] or retrograde. The skeleton of the axon disintegrates along with the myelin sheath and the remaining debris is cleared by infiltrated macrophages [2][3][4]. Both peripheral and central nerve injury can lead to Wallerian degeneration, but subsequent regeneration differs between the nerve types. In the periphery, the nerve fibers can regenerate and reinnervate the tissues via growth factors produced by Schwann cells [5]. In the spinal cord and central nervous system, where nerves are myelinated by oligodendrocytes, nerve recovery is poor to non-existent [2].
A similar but distinct phenomenon known as retrograde degeneration occurs when the axon degenerates proximal to the injury [5]. This backwards degeneration leads to disruption of the cell body and cell death. This form of degeneration does not allow for regeneration if the cell body dies [2][3][4].
Anatomy
Wallerian degeneration can occur within the nerves of the eye resulting in ophthalmic pathologies. Depending on where the nerve damage occurs, Wallerian degeneration or retrograde degeneration can present with ophthalmoscopically visible optic atrophy (retinal ganglion axon death) [6][7]. This degeneration can occur from lesions proximal to or distal to the site of injury (i.e., anterograde (Wallerian) or retrograde degeneration).
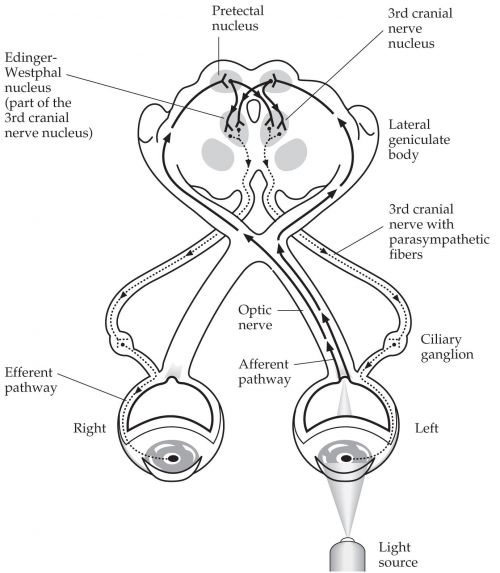
The afferent visual pathway consists of the retina, retinal ganglion cells, retinal nerve fiber layer, the optic nerve, the optic chiasm, optic tract, lateral geniculate nucleus, optic radiations, and visual cortex (Figure 1.). Within the retina, there is an external neuron which is the photoreceptor, which synapses to bipolar cells in the nuclear layer. The internal neuron nearest the vitreous humor is the retinal ganglion cell (RGC). The cell bodies of these neurons make up the ganglion cell layer and the axons form the retinal nerve fiber layer (RNFL) and optic nerve (ON), ultimately synapsing with neurons in the lateral geniculate nucleus (LGN) of the thalamus [8][9].
The axons at the RNFL are initially unmyelinated and later become myelinated with oligodendrocytes when leaving the eye as the ON. The ON is unique in that it is the only part of the central nervous system that can be visualized clinically, allowing neuro-ophthalmologists to diagnose neural defects based on the presentation of the ON. The ON leaves the orbit through the optic canal and then enters the optic chiasm, where approximately half of the fibers cross. Leaving the optic chiasm are the optic tracts which are continuations of the axons that synapse at the LGN [8][9]. Lesions at any point of this pathway can lead to Wallerian or retrograde degeneration [6].
Etiology
Various pathologies can lead to Wallerian degeneration of the RGC axons. Glaucoma is by far the most common cause and can lead to irreversible vision loss as axons of RGCs degenerate (typically due to increased intraocular pressure) [7]. Any optic neuropathy (e.g., optic neuritis, ischemic optic neuropathy, papilledema) however can can damage the nerve fibers within the eye. As the nerve degenerates (Wallerian degeneration) the optic atrophy becomes apparent over time [7].
Damage to the extraocular optic nerve (i.e., intraorbital, intracanalicular, intracranial segments) can occur from many different etiologies (e.g., compressive lesions, trauma) . Retrograde degeneration can still be visualized as optic atrophy via ophthalmoscopy. Initially, the optic nerve may appear normal as the proximal portion of the nerve near the RNFL will be preserved [11] however, over time either form of Wallerian degeneration can eventually result in optic atrophy.
Diagnosis
Optic atrophy is the primary ophthalmoscopic manifestation of Wallerian degeneration and correlates with the patient’s symptoms of loss of visual acuity and/or visual field. Optical Coherence Tomography (OCT) [12] can also quantitatively define both the retinal nerve fiber layer (RNFL) thinning and macular ganglion cell loss over time. Wallerian degeneration typically begins within 24 hours of nerve injury and takes roughly 7 days to complete [11]. During this window, the optic nerve may initially appear normal. Proximal parts of the axon will remain connected to the cell body, which can appear normal and function for 3-4 weeks before degenerating [11] (Figure 2.).
It is important to note that optic atrophy can occur independently of Wallerian anterograde degeneration. Retrograde degeneration following injury to the ON, optic chiasm, or optic tracts can lead to optic atrophy [12]. Retrograde degeneration can lead to death in the affected RGCs by 6-8 weeks [11]. In trans-synaptic degeneration, neuronal degeneration on one side of the synapse can affect the neuron on the other side of the synapse. Via this pathway, damage to neurons from the LGN and visual cortex can lead to optic atrophy as well. This usually occurs when there is occipital lobe damage during utero or early infancy [12].
Treatment
Treatment is based on the underlying lesion or disease (e.g., glaucoma or papilledema) [13]. There is currently no proven regenerative therapy for Wallerian degeneration of the optic nerve. Animal studies in rats with the slow Wallerian degeneration gene (WLDS) have shown temporary axonal protection from Wallerian degeneration but retrograde degeneration still occurred leading to somatic cell death [14]. Further research work is necessary to determine if any of a number of candidate therapeutics may help in regeneration.
Summary
Wallerian (orthograde) degeneration is axonal degeneration occurring distal to the site of injury. It is frequently accompanied by retrograde degeneration, in which axonal degeneration occurs proximal to the site of injury. Injury to the optic nerve anywhere along the pathway from the ganglion cell nucleus to the lateral geniculate nucleus of the thalamus can lead to Wallerian degeneration. The sequelae of Wallerian (anterograde) degeneration will frequently manifest with funduscopic findings consistent with optic atrophy.
Additional Resources
References
- ↑ Maryam Naser, Nafiseh Hashemi. Wallerian Degeneration of Optic Nerve due to Neonatal Intra-cranial Hemorrhage. Journal of Ophthalmology and Research 3 (2020): 61-64.
- ↑ Jump up to: 2.0 2.1 2.2 Gaudet AD, Popovich PG, Ramer MS. Wallerian degeneration: gaining perspective on inflammatory events after peripheral nerve injury. J Neuroinflammation. 2011 Aug 30;8:110. doi: 10.1186/1742-2094-8-110.
- ↑ Jump up to: 3.0 3.1 Conforti L, Gilley J, Coleman MP. Wallerian degeneration: an emerging axon death pathway linking injury and disease. Nat Rev Neurosci. 2014 Jun;15(6):394-409. doi: 10.1038/nrn3680.
- ↑ Jump up to: 4.0 4.1 S.L. Carroll, S.H. Worley, in Reference Module in Neuroscience and Biobehavioral Psychology, 2017
- ↑ Jump up to: 5.0 5.1 Rotshenker S. Wallerian degeneration: the innate-immune response to traumatic nerve injury. J Neuroinflammation. 2011 Aug 30;8:109. doi: 10.1186/1742-2094-8-109.
- ↑ Jump up to: 6.0 6.1 Kanamori A, Catrinescu MM, Belisle JM, Costantino S, Levin LA. Retrograde and Wallerian axonal degeneration occur synchronously after retinal ganglion cell axotomy. Am J Pathol. 2012 Jul;181(1):62-73. doi: 10.1016/j.ajpath.2012.03.030. Epub 2012 May 26.
- ↑ Jump up to: 7.0 7.1 7.2 Ghaffarieh A, Levin LA. Optic nerve disease and axon pathophysiology. Int Rev Neurobiol. 2012;105:1-17. doi: 10.1016/B978-0-12-398309-1.00002-0.
- ↑ Jump up to: 8.0 8.1 Myron Yanoff MD, Joseph W. Sassani MD MHA, in Ocular Pathology (Eighth Edition), 2020.
- ↑ Jump up to: 9.0 9.1 Salazar, Juan & Ramírez, Ana & Hoz, Rosa & Salobrar-Garcia, Elena & Rojas Lozano, Pilar & Fernández-Albarral, Jose Antonio & López-Cuenca, Inés & Rojas, Blanca & Triviño, Alberto & Ramírez, José. (2018). Anatomy of the Human Optic Nerve: Structure and Function. 10.5772/intechopen.79827.
- ↑ Joukal M. (2017) Anatomy of the Human Visual Pathway. In: Skorkovská K. (eds) Homonymous Visual Field Defects. Springer, Cham. doi: 10.1007/978-3-319-52284-5_1
- ↑ Jump up to: 11.0 11.1 11.2 11.3 Alfredo A. Sadun, Michelle Y. Wang, in Handbook of Clinical Neurology, 2011
- ↑ Jump up to: 12.0 12.1 12.2 Amula GM. Optic Atrophy. Medscape. https://emedicine.medscape.com/article/1217760-overview. Published May 1, 2019.
- ↑ Boyd K. Glaucoma Treatment. American Academy of Ophthalmology. https://www.aao.org/eye-health/diseases/glaucoma-treatment. Published December 12, 2020.
- ↑ Beirowski B, Babetto E, Coleman MP, Martin KR. The WldS gene delays axonal but not somatic degeneration in a rat glaucoma model. Eur J Neurosci. 2008 Sep;28(6):1166-79. doi: 10.1111/j.1460-9568.2008.06426.x.


