Anterior Capsular Contraction Syndrome
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Anterior capsule fibrosis and phimosis, commonly described as anterior capsule contraction syndrome (ACCS), is the centripetal constriction and fibrosis of the capsulorhexis following cataract removal. This is a painless condition that remains asymptomatic unless the constriction progresses into the visual axis potentially resulting in decreased visual acuity, pseudophacodonesis and occasionally intraocular lens dislocation. Treatment consists primarily of Nd:YAG relaxing of the anterior capsulotomy of encroaching tissue and recurrence is rare.
Disease Entity
Anterior capsule fibrosis and phimosis is also referred to as capsule contraction syndrome (CCS) or anterior capsule contraction syndrome (ACCS).
Disease
Continuous curvilinear capsulorhexis openings created in cataract surgery are known to contract slightly in non-pathologic eyes.[1] Anterior capsule fibrosis and phimosis is a condition that can occur after phacoemulsification and intraocular lens (IOL) implantation whereby the anterior capsulotomy excessively contracts and fibroses potentially obstructing the visual axis or causing late secondary complications to the IOL such as pseudophacodonesis and IOL tilt, decentration, or dislocation due to zonular laxity, weakness or dehiscence.
Etiology
While the pathogenesis of ACCS is unknown, a possible cause involves populations of residual viable metaplastic lens epithelial cells (LECs) in or on the capsular bag present after cataract surgery that can undergo mesenchymal transition and differentiation to fiber-like cells.[2] Metaplasia and fibrosis of these cells contribute to the purse-string contracture and constriction or even complete closure of the anterior capsulotomy. This response may be exaggerated when there is an imbalance between centrifugal and centripetal forces that act on the zonules and the capsulorhexis perimeter.
Risk Factors
ACCS has been associated with multiple entities. Most common is a small diameter capsulorhexis. Zonular weakness, chronic intraocular inflammation, uveitis, pseudoexfoliation syndrome, zonular laxity, retinitis pigmentosa, advanced age, diabetes mellitus, Behcet’s syndrome, myotonic muscular dystrophy, and high myopia, are known risk factors. [1][3] [4] [5] [6] [7] [8] [9] [10] [11] [12] [13] Several studies have found that the type of IOL used plays an important role in the development and severity of ACCS. Silicone, acrylic, plate haptic, and polyHEMA IOLs have been associated with higher rates of ACCS and more pronounced phimosis when compared to PMMA IOLs. [1][14] [15] [16]
General Pathology
The onset of decreased visual acuity in ACCS patients can range from 2 weeks to more than 3 months. [8][17]Capsule shrinkage and closure involves contraction of the fibrous membrane following fibrous metaplasia of LECs as well as LEC proliferation and outgrowth from the anterior capsule margin onto the IOL toward the center of the capsular opening,[2][18] likely mediated by LEC cytokine signaling.[19]
It has been suggested that the variable incidence of ACCS in the context of IOL type is due to insufficient peripheral capsule expansion by the IOL.[20]
Primary prevention
ACCS may be prevented by utilizing a larger capsulorhexis size,[1][6][7][21] meticulous LEC cleanup at the time of phacoemulsification,[22] [23] [24] or the use of anterior capsule Nd:YAG relaxing incisions in high risk patients soon after phacoemulsification.[11][25] Use of a can-opener capsulotomy rather than a continuous curvilinear capsulorhexis (CCC) is associated with less ACCS,[3] but is less practical with contemporary phacoemulsification. Different methods that can be used to polish the anterior capsule are polishing using a silicon I/A tip, specialized instruments like the singers sweep, polishing using bimanual I/A handpieces, polishing using micro-brushes and UV-A exposure.
Diagnosis
History
Most patients with ACCS are asymptomatic until the process is in an advanced stage. Some may experience painless, progressive visual acuity decline. Glare, haloes, and monocular diplopia may occur if IOL decentration develops. Sudden severe vision loss may occur if IOL dislocation occurs.
Physical examination
Diagnosis of ACCS is addressed in the context of a routine ophthalmologic examination. Serial measurements of the CCC opening may help identify eyes undergoing progressive constriction. After phacoemulsification, onset of blurry vision, visual acuity decline, or compromised pupil function should prompt the examiner to look for signs of ACCS.
Signs
The extent of capsule shrinkage can be determined with slitlamp biomicroscopy. The size of the CCC opening created is visibly reduced, often non-circular, malpositioned, accompanied by fibrotic thickening, wrinkling, and in severe cases, complete closure. Also, the equatorial diameter of the capsule is reduced and the IOL can become decentered.
Symptoms
Symptoms often include painless, progressive blurred vision up to counting fingers, but many cases are asymptomatic. Advanced cases may be associated with glare, haloes, or monocular diplopia if IOL decentration is present. IOL dislocation results in sudden severe vision loss. Retinal detachment and ciliary body detachment have been reported.[26] [27] [28] [29]
Clinical diagnosis
The diagnosis of ACCS in post-op cataract patients is made on the basis of the presence of anterior capsule contraction confirmed with slitlamp biomicroscopy with or without decreased visual acuity compared to the postoperative best-corrected visual acuity (BCVA).
Management
General treatment
Most ophthalmologists perform Nd:YAG LASER anterior capsulotomy which is a simple and painless outpatient procedure.[20][30] [31] [32] Typically 4 or more approximately 1mm radial nicks placed onto the fibrotic anterior capsular annulus are effective in stopping the progression of contraction of the anterior capsule. The LASER is set to anterior focus and an energy of 1 to 3mJ. Radial Nick's are preferred, with care taken not to hit the IOL. Some surgeons have tried cutting out an annulus of capsule using the LASER, but it is not recommended as it deposits in the angle and often leads to raised intraocular pressure.
We recommend that this be accomplished when phimosis has progressed to less than 4mm to prevent potential late zonular dehiscence.
Surgery
In less severe phimosis without invasion of the optical zone, the first choice of treatment is neodymium:YAG (Nd:YAG) laser capsulotomy while manually peeling of the fibrotic membrane is the technique of choice in severe cases with dense fibrous plaques to prevent incomplete reabsorption of loose capsular debris and to decrease the risk of inflammation and recurrence.[33] [34]
Prognosis
The prognosis for non-progression of contraction is very good after Nd:YAG anterior capsulotomy. Non-treatment places the eye at risk of pseudophacodonesis, IOL decentration, tilt, or dislocation, which may arise suddenly.
Additional Resources
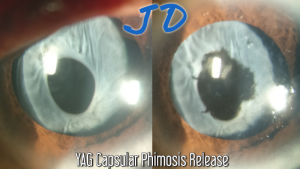
Anterior Capsular Phimosis release and posterior capsulotomy with Nd:YAG LASER. Dr John Davis Akkara, MD
- Above video by Dr John Davis Akkara, MD from India shows posterior capsulotomy and Anterior Capsular Phimosis Release by Radial LASER cuts using NdYAG LASER of 1064nm on. YAG III machine from Zeiss. The posterior capsulotomy is done at posterior focus and anterior using anterior focus. Energy is 1 to 3 mJ per shot titrated according to the response. Abraham capsulotomy lens with a central magnification button can be used, but was not used in this video.
Anterior capsular phimosis release with Nd:YAG anterior capsulotomy. Dr A. John Kanellopoulos, MD
- Above video by Dr John Kanellopoulos, MD from USA shows the procedure of Anterior Capsular Phimosis Release in a patient with DSEK graft in addition to the ACCS.
References
- ↑ 1.0 1.1 1.2 1.3 Joo, C.-K., Shin, J.-A. & Kim, J.-H. Capsular opening contraction after continuous curvilinear capsulorhexis and intraocular lens implantation. J. Cataract Refract. Surg. 22, 585–590 (1996).
- ↑ 2.0 2.1 Marcantonio, J. M., Rakic, J. M., Vrensen, G. F. & Duncan, G. Lens cell populations studied in human donor capsular bags with implanted intraocular lenses. Invest. Ophthalmol. Vis. Sci. 41, 1130–41 (2000).
- ↑ 3.0 3.1 Davison, J. A. Capsule contraction syndrome. J. Cataract Refract. Surg. 19, 582–9 (1993).
- ↑ Lüke, C., Dietlein, T. S., Jacobi, P. C., Konen, W. & Krieglstein, G. K. Massive anterior capsule shrinkage after plate-haptic silicone lens implantation in uveitis. J. Cataract Refract. Surg. 27, 333–6 (2001).
- ↑ Hayashi, H., Hayashi, K., Nakao, F. & Hayashi, F. Area reduction in the anterior capsule opening in eyes of diabetes mellitus patients. J. Cataract Refract. Surg. 24, 1105–1110 (1998).
- ↑ 6.0 6.1 Hayashi, K., Hayashi, H., Matsuo, K., Nakao, F. & Hayashi, F. Anterior capsule contraction and intraocular lens dislocation after implant surgery in eyes with retinitis pigmentosa. Ophthalmology 105, 1239–43 (1998).
- ↑ 7.0 7.1 Hayashi, H., Hayashi, K., Nakao, F. & Hayashi, F. Anterior capsule contraction and intraocular lens dislocation in eyes with pseudoexfoliation syndrome. Br. J. Ophthalmol. 82, 1429–32 (1998).
- ↑ 8.0 8.1 Jin-Poi, T., Shatriah, I., Khairy-Shamel, S. T. & Zunaina, E. Rapid anterior capsular contraction after phacoemulsification surgery in a patient with retinitis pigmentosa. Clin. Ophthalmol. 7, 839–42 (2013).
- ↑ Lee, H. J., Min, S.-H. & Kim, T. Y. Bilateral spontaneous dislocation of intraocular lenses within the capsular bag in a retinitis pigmentosa patient. Korean J. Ophthalmol. 18, 52–7 (2004).
- ↑ Najjar, D. M., Igbre, A. O. & Tsai, F. F. Late capsular bag contraction and intraocular lens subluxation in retinitis pigmentosa: a case report. J. Med. Case Rep. 5, 65 (2011).
- ↑ 11.0 11.1 Nikpoor, N. & Stone, D. U. Rapid capsular phimosis in retinitis pigmentosa. Ophthalmic Surg. Lasers Imaging 41 Online, (2010).
- ↑ Sudhir, R. R. & Rao, S. K. Capsulorhexis phimosis in retinitis pigmentosa despite capsular tension ring implantation. J. Cataract Refract. Surg. 27, 1691–4 (2001).
- ↑ Alintaş, A. G. K. & Dal, D. Capsule contraction syndrome in Behcet’s disease. Int. J. Ophthalmol. 3, 358–60 (2010).
- ↑ Cochener, B., Jacq, P. L. & Colin, J. Capsule contraction after continuous curvilinear capsulorhexis: poly(methyl methacrylate) versus silicone intraocular lenses. J. Cataract Refract. Surg. 25, 1362–9 (1999).
- ↑ Gills, J. P. Anterior capsule contraction. J. Cataract Refract. Surg. 29, 1652 (2003).
- ↑ Gonvers, M., Sickenberg, M. & van Melle, G. Change in capsulorhexis size after implantation of three types of intraocular lenses. J. Cataract Refract. Surg. 23, 231–238 (1997).
- ↑ Waheed, K., Eleftheriadis, H. & Liu, C. Anterior capsular phimosis in eyes with a capsular tension ring. J. Cataract Refract. Surg. 27, 1688–1690 (2001).
- ↑ Kurosaka, D. et al. Fibrous membrane formation at the capsular margin in capsule contraction syndrome. J. Cataract Refract. Surg. 25, 930–5 (1999).
- ↑ Nishi, O. & Nishi, K. Intraocular lens encapsulation by shrinkage of the capsulorhexis opening. J. Cataract Refract. Surg. 19, 544–5 (1993).
- ↑ 20.0 20.1 Dahlhauser, K. F., Wroblewski, K. J. & Mader, T. H. Anterior capsule contraction with foldable silicone intraocular lenses. J. Cataract Refract. Surg. 24, 1216–1219 (1998).
- ↑ Taguri, A. H. & Devlin, H. Capsular phimosis following phacotrabeculectomy. Ophthalmic Surg. Lasers Imaging 36, 245–8
- ↑ Tadros, A., Bhatt, U. K., Abdul Karim, M. N., Zaheer, A. & Thomas, P. W. Removal of lens epithelial cells and the effect on capsulorhexis size. J. Cataract Refract. Surg. 31, 1569–74 (2005).
- ↑ Sacu, S. et al. Effect of anterior capsule polishing on fibrotic capsule opacification: three-year results. J. Cataract Refract. Surg. 30, 2322–7 (2004).
- ↑ Hanson, R. J., Rubinstein, A., Sarangapani, S., Benjamin, L. & Patel, C. K. Effect of lens epithelial cell aspiration on postoperative capsulorhexis contraction with the use of the AcrySof intraocular lens: randomized clinical trial. J. Cataract Refract. Surg. 32, 1621–6 (2006).
- ↑ Hayashi, K., Yoshida, M., Hirata, A. & Hayashi, H. Anterior capsule relaxing incisions with neodymium:YAG laser for patients at high-risk for anterior capsule contraction. J. Cataract Refract. Surg. 37, 97–103 (2011).
- ↑ Tielsch, J. M. et al. Risk factors for retinal detachment after cataract surgery. A population-based case-control study. Ophthalmology 103, 1537–45 (1996).
- ↑ Lanzl, I. M. & Kopp, C. Ciliary body detachment caused by capsule contraction. J. Cataract Refract. Surg. 25, 1412–4 (1999).
- ↑ Srinivasan, S., van der Hoek, J., Green, F. & Atta, H. R. Tractional ciliary body detachment, choroidal effusion, and hypotony caused by severe anterior lens capsule contraction following cataract surgery. Br. J. Ophthalmol. 85, 1261–2 (2001).
- ↑ Salzmann, J., Khaw, P. T. & Laidlaw, a. Choroidal effusions and hypotony caused by severe anterior lens capsule contraction after cataract surgery. Am. J. Ophthalmol. 129, 253–4 (2000).
- ↑ Toldos, J. J. M., Roig, A. A. & Benabent, E. C. Total anterior capsule closure after silicone intraocular lens implantation. J. Cataract Refract. Surg. 22, 269–271 (1996).
- ↑ Reeves, P. D. & Yung, C.-W. Silicone intraocular lens encapsulation by shrinkage of the capsulorhexis opening. J. Cataract Refract. Surg. 24, 1275–1276 (1998).
- ↑ Gallagher, S. P. & Pavilack, M. a. Risk factors for anterior capsule contraction syndrome with polypropylene or poly(methyl methacrylate) haptics. J. Cataract Refract. Surg. 25, 1356–61 (1999).
- ↑ Reyntjens, B., Tassignon, M.-J. B. R. & Van Marck, E. Capsular peeling in anterior capsule contraction syndrome: surgical approach and histopathological aspects. J. Cataract Refract. Surg. 30, 908–12 (2004).
- ↑ Koizumi, K., Watanabe, A., Koizumi, N. & Kinoshita, S. Peeling the fibrous membrane from the anterior capsule for capsulorhexis contraction after phacoemulsification in aphakic patients. J. Cataract Refract. Surg. 28, 1728–32 (2002).