Anesthesia in Vitreoretinal Surgery
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
The majority of vitreoretinal surgeries are performed on a one-day (outpatient) surgery basis. Historically, vitreoretinal surgery was mainly performed under general anesthesia due to the prolonged duration of surgery, the need for a motionless field, and the intensity of the surgical stimulus. Over the last two decades, there has been a trend towards vitreoretinal surgeries being completed under monitored anesthesia care with local anesthetic blocks and less usage of general endotracheal anesthesia in both the United Kingdom and the United States.[1] [2] Multiple local anesthesia methods are utilized in vitreoretinal surgery, including subconjunctival, retrobulbar, peribulbar, and sub-tenon blocks.
Anesthesia Techniques
General Anesthesia
General anesthesia involves a state of controlled unconsciousness. This is more suitable for prolonged and complex vitreoretinal procedures and for individuals that may have difficulties remaining motionless during surgery, such as children, patients with developmental delay, patients with movement disorders, and patients with certain psychiatric conditions, such as profound claustrophobia. Additionally, vitreoretinal surgeries with more intense stimuli from manipulation of extraocular muscles, such as scleral buckling surgeries, may also be better suited for general anesthesia. The potential drawbacks of using general anesthesia include prolonged recovery time, risks of general anesthesia, and the potential for abrupt intraocular pressure spikes upon emergence extubation. For the last point, it is important to discuss with the anesthesiologist ways to mitigate extreme movements and valsalva during emergence. There are also increased costs and operation room utilization time with general anesthesia. Anesthesia, surgical, and recovery costs and time are significantly higher in patients who receive general anesthesia compared to local anesthesia.[3] Some surgeons and patients prefer laryngeal mask airway (LMA) ventilation, which is an alternate to endotracheal intubation. Performing general anesthesia with LMA decreases post-operative discomfort for the patient due to avoiding irritation of the subglottic tracheobronchial system[4]. Retrobulbar, sub-tenon, or periorbital anesthesia can be used as an adjunct in general anesthesia cases to decrease post-operative pain and to stabilize intraoperative hemodynamics.
Sedation with local anesthesia (subconjunctival/retrobulbar/peribulbar/sub-tenon blocks)
Local anesthesia is a highly utilized technique for ophthalmic surgeries, including vitreoretinal surgeries. When a patient is anxious or additional sedation is needed, propofol, morphine-class analgesics, and benzodiazepines can be an option. However, it is not a substitute for analgesic, and caution must be used because excessive sedation can become counterproductive due to increased risk of disinhibition with increased patient movement and poor patient compliance. We advise minimal use of sedation to offer opportunity to communicate with the patient and to minimize risks associated with excessive sedation. Additionally, patient anxiety may stem from not understanding what is coming, so it is important to think of local anesthesia as both local and vocal – you must talk to your patient and reassure them.
Subconjunctival anesthesia
Subconjunctival anesthesia is used infrequently in intraocular surgeries, especially in vitreoretinal surgery. A previous single report with subconjunctival anesthesia in selected simple cases of small gauge vitrectomy (25- or 27-gauge) resulted in satisfactory analgesia without increased complication rates from lack of akinesia.[5] A recent prospective randomized clinical trial by Fan et al. showed that subconjunctival anesthesia for selected patients undergoing 23- or 25-gauge pars plana vitrectomy was safe and effective.[6] We advise only using this technique for simple vitrectomy cases if it is ever to be used.
Retrobulbar/peribulbar blocks
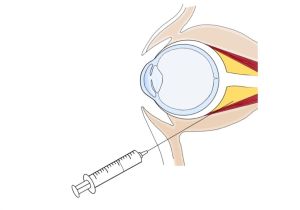
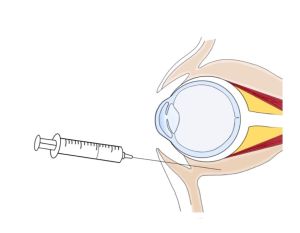
Retrobulbar or intraconal block is performed by advancing a needle tip inside the muscle cone and injecting a low volume (4-5mL) of local anesthesia (Figure 1). Retrobulbar blocks are highly effective and induce a rapid onset of analgesia and akinesia. Peribulbar block is given extraconal with a slightly larger volume of local anesthetic (5-10mL) (Figure 2). Inward diffusion of anesthetic similarly leads to globe akinesia and anesthesia with a more gradual onset compared to retrobulbar blocks. Peribulbar blocks often result in conjunctival chemosis due to its more anterior delivery, and this may affect visualization during the case[7].
Regional blocks for vitreoretinal surgery are generally safe, but there are complications associated with sharp needle blocks (more-so with retrobulbar blocks, but is still possible with peribulbar blocks) including retrobulbar hemorrhage, precipitation of the oculocardiac reflex, postoperative diplopia from inadvertent injury to extraocular muscles, penetration/perforation of the globe with possible intraocular injection of local anesthetics, optic nerve trauma, central retinal artery occlusion, and intravascular injection of local anesthetics. When deciding upon anesthetic technique, the surgeon must consider the increased risk of globe perforation during retrobulbar injection in patients with longer or very short axial length or in patients with a previously placed scleral buckle.
Sub-tenon block
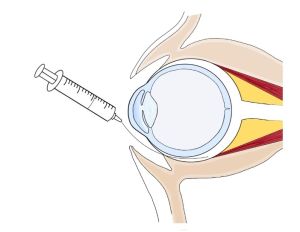
The tenon’s capsule is a layer of connective tissue that surrounds the globe and is in close apposition to the conjunctiva. Sub-tenon block is given in the subtenon’s space after dissection of the conjunctiva in the conventional way. Local anesthesia can then be given with a low volume (4-5mL) into the sub-tenon space, which will then produce analgesia and akinesia by diffusing posteriorly to the retrobulbar space (Figure 3). Another method for sub-tenon’s block without conjunctival cutdown involves use of an 18-gauge needle, conjunctival forceps, and a 20-gauge IV cannula (soft tip angiocatheter) (Figure 4). The 18-gauge needle is used to initiate a puncture in the conjunctiva and Tenon’s capsule in the inferonasal conjunctiva, approximately 3-4 millimeters from the limbus. The 20-gauge IV cannula (soft tip angiocatheter) is secured to a luer lock syringe and navigated along the plane of the sub-Tenon space and along the contour of the globe in the posteromedial direction with slow injection of local anesthetic (AAO Video Link for Modified Sub-tenon Block ). This method avoids conjunctival dissection, is simple, and avoids risks of sharp needle blocks. There are some drawbacks to consider with adopting this method. If the angiocatheter is not maximally inserted, the block may lead to significant chemosis that can make visualization and access to trocars difficult during surgery. This may require conjunctival cutdown to relieve the chemosis. Additionally, the level of akinesia achieved with sub-Tenon blocks is often inadequate for delicate vitreoretinal procedures like internal limiting membrane peeling, as the eye is usually left with a slight, but troublesome, ‘shimmering’ movement. A combination approach can also be used to provide both a peribulbar block (5mL) and a sub-Tenon block (5mL).
Potential problems during vitreoretinal anesthesia
Oculocardiac reflex during scleral buckle surgery
The oculocardiac reflex (OCR) is a well-known phenomenon, in which manipulation of the extraocular muscles, globe, or conjunctiva can result in a heart rate decrease of 20% or more.[8] This is due to the connection between the ophthalmic branch of the trigeminal nerve and the vagus nerve, which mediates the reflex.[8] The OCR is especially important to consider during scleral buckle surgery. Local anesthesia delivered through a retrobulbar, peribulbar, or subtenon block can prevent the OCR. Scleral buckle surgery is commonly performed under general anesthesia, so for these cases, local anesthesia along with general anesthesia can prevent OCR. If OCR is encountered, it can typically be managed by the anesthesiologist, and if significant bradycardia occurs, the anesthesiologist may treat it with certain medications (i.e., atropine). Although extremely rare, serious cardiac arrhythmias leading to cardiac arrest can occur, making OCR an important consideration.
Intraocular perforation with sharp needle anesthesia (retrobulbar/peribulbar blocks)
Iatrogenic globe perforation is a rare complication that can occur with sharp needle blocks. The risk is highest for retrobulbar blocks, although can still occur during subconjunctival and peribulbar injections if sharp needles are used.[9] Inadvertent globe trauma occurs at an incidence of 1 in every 16,000 cases of peribulbar anesthesia and in 0.9 in every 10,000 cases of retrobulbar anesthesia.[9] Complications of globe perforation include retinal toxicity, choroidal hemorrhage, vitreous hemorrhage, retinal tear, retinal detachment, proliferative vitreoretinopathy, and subretinal hemorrhages.[10] Early signs of this serious complication may include the patient reporting sharp pain and vision loss, an abnormal red reflex, and possibly an increase in intraocular pressure.[11] If this complication is suspected then the patient needs timely retinal evaluation and intervention, such as globe exploration, laser photocoagulation, or vitreoretinal surgery.[11] Factors that can increase the risk of globe perforation during sharp needle anesthesia include the use of long and sharp needles, incorrect angle of needle insertion, patient movement during block, previous history of scleral buckle procedure, and long axial length (>26mm).[9] [10] [11]
Valsalva-induced suprachoroidal hemorrhage during pars plana vitrectomy under general anesthesia
Valsalva-induced suprachoroidal hemorrhage is a serious complication that can occur during vitreoretinal surgery.[12] It can happen towards the conclusion of a case when general anesthesia becomes light. Painful stimuli, such as scleral indentations during peripheral retina check, under light sedation can cause the patient to feel the stimulus and react. The patient may then cough or “buck,” which can result in suprachoroidal hemorrhage due to acute rise in intraocular pressure from Valsalva maneuvers. To minimize this risk, it is important to collaborate with the anesthesiologist to maintain deep sedation until the conclusion of the case. In addition, the use of local anesthetic blocks during general anesthesia can provide an additional level of analgesia and can reduce pain with indentation. Given the possibility of coughing and/or Valsalva at the time of extubation, it is advised to suture sclerotomies at the time of closure. Deep extubation (i.e., removal of endotracheal tube while patient is still anesthetized) decreases the risk of coughing and bucking, but not all patients are good candidates for deep extubation, including those with severe reflux. Extubation goals and techniques should be discussed with the anesthesiologist during briefing.
Conclusion
The majority of vitreoretinal surgeries can be performed under monitored sedation with local anesthesia, which can be safer in certain situations and also quicker than general anesthesia. However, sedation should be minimal to avoid patient disinhibition, excessive patient movement, and reduced patient cooperation from excessive sedation. When deciding on local anesthesia techniques, patient factors should be considered to select an effective and safe option for the patient. Sub-tenon blocks are generally a safer and an effective alternative to sharp needle anesthesia blocks. Lastly, it is important to think of local anesthesia as both local and vocal – you must talk to your patient and reassure them throughout the case.
References
- ↑ Yannuzzi, N.A.; Sridhar, J.; Flynn, H.W.; Gayer, S.; Berrocal, A.M.; Patel, N.A.; Townsend, J.; Smiddy, W.E.; Albini, T. Current Trends in Vitreoretinal Anesthesia. Ophthalmol. Retin. 2019, 3, 804–805. https://doi.org/10.1016/J.ORET.2019.05.020
- ↑ Sallam, A.A.B.; Donachie, P.H.J.; Williamson, T.H.; Sparrow, J.M.; Johnston, R.L. The Royal College of Ophthalmologists’ National Ophthalmology Database Study of Vitreoretinal Surgery: Report 5, Anaesthetic Techniques. Br. J. Ophthalmol. 2016, 100, 246–252. https://doi.org/10.1136/BJOPHTHALMOL-2014-306467
- ↑ Siddiqui M.Z; Chauhan M.Z.; Stewart A.F.; Sallam A.B. Analysis of Operational Efficiency and Cost Differences between Local and General Anesthesia for Vitreoretinal Surgery. Healthcare. 2022, 10, 1918. https://doi.org/10.3390/healthcare10101918
- ↑ Leister N, Heindl LM, Rokohl AC, Böttiger BW, Menzel C, Ulrichs C, Schick VC. Laryngeal Mask Airway Versus Endotracheal Intubation during Lacrimal Duct Stenosis Surgery in Children-A Retrospective Analysis. Children (Basel). 2024 Mar 7;11(3):320. doi: 10.3390/children11030320. PMID: 38539355; PMCID: PMC10969069.
- ↑ Malik, A.; Foster, RE.; Correa, Z.; Peterson, M.; Miller, D.; Riemann, C.; Anatomical and visual results of transconjunctival sutureless vitrectomy using subconjunctival anesthesia performed on select patients taking anticoagulant and antiplatelet agents, Retina, 2012, 32, 905-911. doi: 10.1097/IAE.0b013e31822f55c4.
- ↑ Fan H.; Qian Z.; Tzekov R.; Lin, D.; Wang, H.; Li, W. A New Two-Step Anesthesia for 23- or 25-Gauge Vitrectomy Surgery: A Prospective Randomized Clinical Trial. Ophthalmic Research, 2021, 64, 34-42. doi: 10.1159/000508510
- ↑ Alhassan MB, Kyari F, Ejere HO. Peribulbar versus retrobulbar anaesthesia for cataract surgery. Cochrane Database Syst Rev. 2015 Jul 2;2015(7):CD004083. doi: 10.1002/14651858.CD004083.pub3. PMID: 26133124; PMCID: PMC7175781.
- ↑ Jump up to: 8.0 8.1 Dunville, L.; Sood, G.; Kramer, J. Oculocardiac Reflex. StatPearls 2022.
- ↑ Jump up to: 9.0 9.1 9.2 Al-Shehri, A.; Al-Ghamdi, A.; Al-Shehri, A.; Alakeely, A. Management of iatrogenic globe perforation during peribulbar anesthesia with submacular hemorrhage. Oman J Ophthalmology. 2020, 2, 95-97. doi: 10.4103/ojo.OJO_208_2019
- ↑ Jump up to: 10.0 10.1 Agrawal, N.; Nakhwa, C.; Jhawar, S.; Khare, G. Management of globe perforation during cataract surgery. Journal of Cataract and Refractive Surgery Online Case Reports. 2017, 5, 24-26. doi: 10.1016/j.jcro.2017.03.001
- ↑ Jump up to: 11.0 11.1 11.2 Dai, Y.; Sun, T.; Gong, JF. Inadvertent globe penetration during retrobulbar anesthesia: A case report. World J Clin Cases, 2021, 9, 2001-2007. doi: 10.12998/wjcc.v9.i8.2001
- ↑ Pollack, A.L.; Richard McDonald, H.; Ai, E.; Johnson, R.N.; Dugel, P.U.; Folk, J.; Gilbert Grand, M.; Michael Lambert, H.; Schwartz, S.; Miller, R.D. Massive Suprachoroidal Hemorrhage during Pars Plana Vitrectomy Associated with Valsalva Maneuver. Am J Ophthalmol 2001, 132, 383–387.