Anesthesia for Oculoplastic Surgery
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Digital Diffusion Technique when injecting local anesthetics
The choice of anesthetic in Oculoplastic Surgery is dependent on the nature of the procedure to be performed as well as the patient’s and surgeon’s preference. Informed by this, the choice of inhalational or intravenous anesthetic, concurrent local injection of anesthetic with epinephrine, supplementation with long-acting anesthetics such as Exparel, use of hyaluronidase to disperse the anesthetic and even the addition of topical agents such as tetracaine, proparacaine, cocaine or cophenylcaine are decided preoperatively by the operative surgeon.
Surgical procedures best performed under a general anesthetic are those for which control of the patient’s airway and the deepest level of sedation are required. These procedures may include orbital tumor removal, orbital decompression, orbital fracture repair, enucleation, evisceration, exenteration and dacryocystorhinostomy.
Procedures that are readily performed under local anesthetic with or without intravenous sedation include eyelid surgery (blepharoplasty, ptosis repair, eyelid malposition repair) and eyelid cancer excision and reconstruction,
To review, local anesthetics are membrane stabilizing agents that inhibit voltage-gated sodium channels in the neuronal cell membrane. They increase action potential thresholds and as a result, decrease the perception of pain and inhibit muscular contraction. [1]They consist of three key components: a lipophilic aromatic ring, intermediate ester or amide chain, and terminal amine.
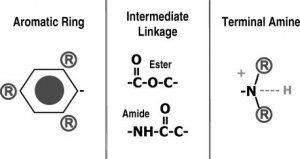
The aromatic ring provides improved lipid solubility of the compound enhancing diffusion through the nerve sheaths and individual axonal membrane. This diffusion correlates with potency of the drug. For example, bupivacaine is more lipid soluble than lidocaine and hence, is prepared as a 0.5% concentration rather than 2% secondary to its higher potency.
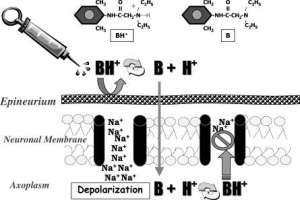
The terminal amine exists in either a tertiary form (3 bonds) which is lipid soluble or a quaternary form (4 bonds) which is water soluble as it is positively charged. It acts as a switch, allowing the molecule to exist in lipid soluble or water-soluble form. This contributes to the time of onset of the local anesthetic- determined by the proportion of molecules that converts to a tertiary, lipid-soluble structure when exposed to the physiologic pH of 7.4. When local anesthetics are in solution, they are formulated as a hydrochloride salt in which the molecules exist in a quaternary, water-soluble form at the time of injection, unable to penetrate the neuron.
The ionization constant (pKa) of the anesthetic represents the pH at which 50% of the molecules exist in the tertiary and the other 50% in quaternary forms. The pKa of all local anesthetics (Table 1) is higher than the physiologic pH and therefore, when injected into skin, a greater proportion of molecules exist in the quaternary water-soluble form. The anesthetics with a lower pKa have a faster onset of neural blockade. In addition, infected or inflamed tissue results in a more acidic environment which further impairs the ability of an anesthetic to convert into the lipid soluble form.
In addition, the intermediate chain of either the amide or ester defines a classification of the anesthetic as well as the pattern of biotransformation. Esters are hydrolyzed by plasma cholinesterase, while amides are metabolized in the liver. The duration of anesthetics is determined by their affinity for plasma proteins, as well as proteins within sodium channels. For example, bupivacaine has the greatest affinity for protein binding and has the longest duration of action. Duration of action is also influenced by constriction of the nearby vasculature. For this reason, vasoconstrictors (epinephrine) are added to anesthetics to delay absorption and prolong the anesthetic effect.
| Drug | pKa | Max dose (w/epi) mg/kg | Class |
| Cocaine | 8.6 | 3 | Ester |
| Procaine | 8.9 | 8 (10) | Ester |
| Tetracaine | 8.5 | 1.5 (1.5) | Ester |
| Bupivacaine | 8.1 | 2 (3) | Amide |
| Lidocaine | 7.9 | 4.5 (7) | Amide |
| Mepivacaine | 7.6 | 5 (7) | Amide |
| Ropivacaine | 8.1 | 3 (3.5) | Amide |
| Exparel | 8.1 | 266mg total | Amide |
Ester local anesthetics are topical preparations including tetracaine, proparacaine, and cocaine. Topical anesthetic eye drops are usually instilled at the start of most oculoplastic procedures to minimize discomfort from antiseptics and help fitting of cornea protectors. The instillation of proparacaine 0.5% eye drops is more comfortable than 0.5% Tetracaine eye drops[4] . Tetracaine has a pKa of 8.5 and high lipid solubility, which places it amongst the most potent of any local anesthetic[5] . It has moderate protein binding, allowing a duration of action up to 200 minutes.
Dosing should not exceed 1.5 to 3 mg/kg of actual patient weight. As metabolism occurs via plasma cholinesterase primarily produced from the liver, caution is required for dosing in patients with liver disease, neonates, and patients with atypical homozygous pseudo cholinesterase deficiency [6]. In fact, the use of Tetracaine and Proparacaine would be contraindicated in a patient with a pseudo cholinesterase deficiency. Allergic reactions to Tetracaine are rare, but possible, due to para-amino benzoic acid (PABA) which is a metabolite of preservatives used.
Proparacaine has a pKa of 8.9 and rapid onset of action. The duration of action of proparacaine is 15 minutes and therefore, may require reinstallation during the procedure. The installation of a drop anesthetic during sedation, may serve to determine the level of sedation prior to needle injection- a “canary in the coal mine” of discomfort metric. Pre-treatment with topical anesthetics (cutaneous or conjunctival) may help reduce the discomfort of local anesthetic injection, especially in needle phobic patients.
Most of the injectable local anesthetics are amide local anesthetics including lidocaine, prilocaine, mepivacine, bupivacaine, levobupivacine, and ropivacaine. The most widely used injectable local anesthetic is lidocaine hydrochloride 1%-2% with and without epinephrine (1:100,000 or 1:200,000), which has a pKa of 7.6 and therefore, a rapid onset of action (1 minute). Its duration of action is 1-3 hours depending on the strength of the preparation and the presence of epinephrine[7] . The addition of epinephrine in the local anesthetic provides a hemostatic effect through vasoconstriction[8] and delays diffusion of the anesthetic. Bupivacaine hydrochloride 0.50%-0.75% is a longer acting agent than lidocaine with a duration of 6-8 hours. It has however, a slower onset of action of 10 minutes secondary to the higher pKa of 8.1.
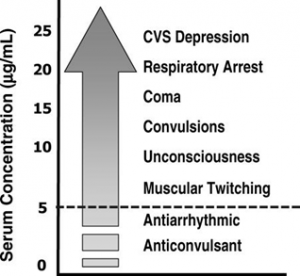
Although the volumes of anesthetics injected tend to be small for most oculoplastic surgical procedures it is important to note that as local anesthetics are absorbed from the injection site and their concentration in the bloodstream rises, the peripheral nervous system and central nervous system are depressed in a dose-dependent manner. At low doses, anesthetics may be used for antiarrhythmic and anticonvulsive purposes; however, at higher doses, they induce seizure activity due to selective depression of central inhibitory tracts, coma, respiratory arrest, and eventually cardiovascular collapse. Lidocaine toxicity is additive and should not exceed the total dose of 4.5mg/kg. In addition, all local anesthetics have CNS depressant properties and therefore, may potentiate respiratory depression associated with sedatives and opioids. Bupivacaine possesses greater potential for direct cardiac toxicity than other agents. Local anesthetics with epinephrine may cause ischemic necrosis of tissues.
These anesthetics presented have a pH of 3.5-5.5. As a result, they are painful upon injection. Mixing the local solution with sodium bicarbonate (1 cc NaHCO3 to 9 cc Lidocaine) alters the pH sufficiently to reduce discomfort. By increasing the pH, as well as the ratio of nonionized to ionized local anesthetic, the duration of sensory blockade is extended, while the onset of action is lessened. [9]
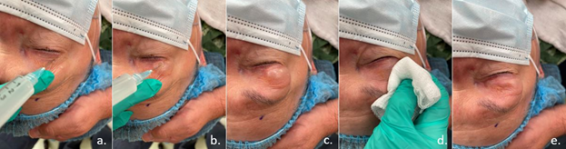
Slow injection with a small gauge needle eases discomfort. For eyelid surgery, the use of a “Digital Diffusion” technique reduces discomfort as well as bruising by decreasing the number of injection sites. In this technique, as described for eyelid surgery, a bolus of anesthetic (2 cc/ eyelid) is slowly injected into the lateral eye aspect of the eyelid (needle pointing away from the globe) in the subcutaneous/ supraorbicularis oculi space (Figure 4a-c). The needle is withdrawn, and the gloved hand of the surgeon slowly wipes the local across the eyelid milking the solution from lateral to medial (Figure 4d-e).
This technique is enhanced by the addition of hyaluronidase to the local solution (100-150 units per 20 cc or so). This technique safely allows for widespread local anesthetic dispersion without multiple needle sticks. Additionally, the hyaluronidase provides for a complete return to normal anatomic skin draping without tissue distortion. This allows for patient marking if needed after anesthetic injection.
In contrast, enucleation and evisceration are commonly performed under general anesthesia with the administration of a retrobulbar and subconjunctival injection of local anesthetic pre- and postoperatively.[10] The delivery of local anesthetics to the retrobulbar space prior to enucleation and evisceration has been shown to provide significant control of bleeding, the need for less inhalational or intravenous anesthesia as well as decreased postoperative pain [11]. A commonly used anesthetic “cocktail” is the combination of lidocaine 2% with 1:100,000 epinephrine and bupivacaine 0.75% with 1:200,000 epinephrine, hyaluronidase (adjuvant to facilitate the spread of the anesthetic) and sodium bicarbonate (to decrease the pH and improve the comfort of injection).
Liposomal bupivacaine (trade name: Exparel, Pacira Biosciences, Inc.), an extended-release liposomal formulation of bupivacaine administered as a depot injection, with a duration of action of up to 72 hours, has been used successfully for effective postoperative pain management after enucleation and evisceration[12]. Liposomes are amphipathic (containing both hydrophilic and hydrophobic parts) molecules that form lipid bilayer spherical vesicles that allow for a sustained release of drug delivery without the need for continuous infusion or risk of toxicity[13] . Be aware that Exparel should not be combined with Lidocaine in the same injection, as it may cause an immediate release of bupivacaine from Exparel. The administration of Exparel may follow lidocaine after 20 minutes or more.
Anesthesia is constantly undergoing innovation and improvement. The use of intravenous sedation with effective and short acting agents such as Propofol has enabled many surgeons to convert from general anesthesia effectively and painlessly to deep intravenous sedation. Combined with short, mid, and long-acting injectable anesthetics, surgeons are able to provide safe, effective, and comfortable pain sedation/anesthesia with a minimum of post operative downtime and a rapid recovery.
- ↑ Lucia Bianconi M, Bianconi M. Mechanism of action of local anaesthetics: a practical approach to introducing the principles of pKa to medical students. Biochemical Education. 1998;26(1):11–13.
- ↑ Becker DE, Reed KL. Essentials of Local Anesthetic Pharmacology. Anesthesia Progress. 2006 Fall; 53(3): 98–109.
- ↑ Milam SB, Giovannitti Jr JA. Local anesthetic in dental practice. Dental Clinics of North America. 1984; Jul;28(3):493-508
- ↑ Bartfield JM, Holmes TJ, Raccio-Robak N. A comparison of proparacaine and tetracaine eye anesthetics. Acad Emerg Med. 1994;1(4): 364–367.
- ↑ Stringer CM, Lopez MJ, Maani CV, Tetracaine. StatPearls Publishing. 2021 Jan.
- ↑ Rico-Mora DA, Walton L, Navas-Blanco JR. Prolonged neuromuscular blockade in a middle eastern female patient homozygous for atypical plasma cholinesterase. Saudi J Anaesth. 2018 Oct-Dec;12(4):651-652.
- ↑ Ing B E. Philteos J. Sholohov G. Kim T D. Nijhawan N. Mark W P. Gilbert J. Local anesthesia and anxiolytic techniques for oculoplastic surgery. Clinical Ophthalmology. 2019; 13: 153-160
- ↑ Sheikh R, Dahlstrand U, Memarzadeh K, Blohmé J, Reistad N, Malmsjö M. Optimal epinephrine concentration and time delay to minimize perfusion in eyelid surgery: measured by laser-based methods and a novel form of extended-wavelength diffuse reflectance spectroscopy. Ophthalmic Plast Reconstr Surg. 2018;34(2):123–129.
- ↑ DiFazio CA, Carron H, Grosslight KR, Moscicki JC, Bolding WR, Johns RA. Comparison of pH-adjusted lidocaine solutions for epidural anesthesia. Anesth Analg 1986; 65:760-4.
- ↑ Calenda E, Retourt A, Muraine M. Is evisceration of the eye more painful than enucleation? Eur J Anaesthesiol 1999; 16:117.
- ↑ Lesin M, Sundov ZD, Jukic M, Puljak L. Postoperative pain in complex ophthalmic surgical procedures: Comparing practice with guidelines. Pain Med 2014; 15:1036‑42.
- ↑ Ang, M and Silkiss, RZ The Use of Long-Acting Liposomal Bupivacaine (Exparel) for Postoperative Pain Control Following Enucleation or Evisceration OPRS
- ↑ Taylor, A and McLeod G., Basic Pharmacology of local anesthetics. BJA Education, 2020; 20(2): 34-41