Actinic Keratosis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
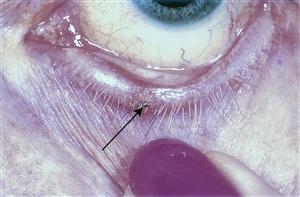
Actinic keratoses are a premalignant squamous lesions. They may appear clinically as a erythematous, scaly macules or papules. Lesions typically present in middle aged or elderly patients. Sun exposed areas are most commonly affected. Squamous cell carcinoma may develop from preexisting actinic keratoses. Thus, biosy of suspected lesions and long term follow-up are necessary in patients with this condition. The risk of subsequent metastastatic dissemination is very low (0.5-3.0%)[1]
Disease Entity
Actinic Keratosis ICD-10-CM L57.0
Etiology and Risk Factors
The most likely factor that leads to the development of actinic keratosis is sunlight exposure, specifically UVA and UVB sunlight.[2] Exposure to these forms of radiation leads to a complex series of genetic events which eventually lead to the development of actinic keratosis and squamous cell carcinoma. History of chronic sunlight exposure. Lack of sunscreen use when outdoors. Fairer skin types (Fitzpatrick types I,II)
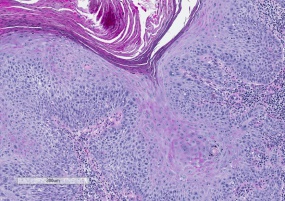
Pathology
Histologically, hyperkeratosis, parakeratosis, dyskeratosis, and solar elastosis are seen. Cellular atypia may be present, with increased nuclear-to-cytoplasmic ratio, pleomorphism, or nuclear hyperchromatism. Exposure to these forms of radiation leads to a complex series of genetic events which eventually lead to the the proliferation of squamous epithelial cells and dysplastic changes in the skin that are characteristic of actinic keratosis.
Diagnosis
Preliminary diagnosis may be made based on the patient's history and clinical appearance. Examination of skin can be performed with a slit-lamp, dermatoscope, or with the naked eye. However, definitive diagnosis of a new lesion requires a biopsy with review by a pathologist.
- Patients will usually present with a slowly developing scaling and erythomatous lesion of the skin.
- Examination of skin can be performed with a slit-lamp, dermatoscope, or with the naked eye. Erythematous (red), scaly macule (flat pigmented lesion) or papule (solid, elevated lesion) may be present on the skin surface. Multiple lesions may be present.
- The skin of affected areas may feel rough, or have a "sandpapery" texture. The lesions may have a round and scaly appearance. Itching or irritation may be present on the skin of affected individuals. It appears clinically as a erythematous, scaly macule or papule.
- Actinic keratoses are most commonly found on the face, lips, ears, back of the hands, forearms, scalp or neck.[3]
- Lesions with bleeding, persistent itching, growth, or changes may be biopsied to confirm diagnosis.
Differential diagnosis
- Squamous cell carcinoma
- Bowen's disease
- Basal cell carcinoma
- Lentigo maligna
Management
Observation, medical, or surgical treatment may be recommended depending on individual circumstances. Progression to squamous cell cancer is generally slow and in elderly patients with multiple comorbidities, for example, observation may be the best choice.
- Medical therapy
- The following topical medications have been FDA approved for treatment of Actinic Keratosis.
- 5-fluorouracil (5-FU)
- Imiquimod cream
- Ingenol mebutate gel
- Topical diclofenac gel
- A systematic review compared the relative efficacy of 5-fluorouracil 0.5% in salicylic acid 10% (5-FU/SA) vs. ingenol mebutate (IMB) and imiquimod 2.5%/3.75% (IMI) for actinic keratosis on the face, forehead or scalp.[4] The study showed both treatments to be effective for actinic keratosis.
- Cryotherapy is typically carried out in a dermatologist's office for facial lesions. Periocular lesions are best treated by an oculofacial plastic surgeon.
- Blue light therapy, also known as photodynamic therapy (PDT), is an FDA-approved in-office treatment for actinic keratosis.[5]
- TCA chemical peels may be useful in patients with diffuse lesions that are challenging to treat one at a time.
- The following topical medications have been FDA approved for treatment of Actinic Keratosis.
- Surgical therapy
- Lesions may be completely excised if there is concern for malignancy. However, in most cases, actinic keratosis may be observed clinically for progression.
- Laser treatments may also be an option if there is no concern for malignancy.
Prognosis and Follow up
Actinic keratosis has a generally good prognosis. It rarely progresses into squamous cell carcinoma or other malignancy.
- Follow up should be determined by the ophthalmologist or dermatologist based on the patient's other underlying risk factors and health
- Actinic keratosis generally has a low chance of progressing to more malignant lesions.
Complications
Medical treatments have various possible complications and side effects, and should be discussed with your physician before starting treatment. Surgical treatments may also have complications, such as wound infection or dehisence, and should be discussed with your surgeon before undergoing surgery. Observation also carries with it the possibility that actinic keratosis will develop into a more malignant lesion.
Additional Resources
References
- ↑ Ophthalmic Pathology and Intraocular Tumors, Section 4. Basic and Clinical Science Course. San Francisco: American Academy of Ophthalmology; 20011-12
- ↑ Ortonne, J.-P. (2002), From actinic keratosis to squamous cell carcinoma. British Journal of Dermatology, 146: 20–23. doi: 10.1046/j.1365-2133.146.s61.6.x
- ↑ http://www.mayoclinic.org/diseases-conditions/actinic-keratosis/basics/definition/con-20030382
- ↑ Stockfleth, Eggert, Gillian C. Sibbring, and Ivette Alarcon. "New topical treatment options for actinic keratosis: a systematic review." Acta dermato-venereologica 96.1 (2016): 17-23.
- ↑ Jeffes, Edward W., et al. "Photodynamic therapy of actinic keratoses with topical aminolevulinic acid hydrochloride and fluorescent blue light." Journal of the American Academy of Dermatology 45.1 (2001): 96-104.