Conjunctival Inclusion Cyst: Difference between revisions
(Text copyedits and formatting.) |
(Text copyedits and formatting.) |
||
| Line 180: | Line 180: | ||
== Surgery == | == Surgery == | ||
Excision of the conjunctival inclusion cyst can be performed under topical anesthesia with 0.5% proparacaine, associated with subconjunctival infiltration of lidocaine around the cyst. A | Excision of the conjunctival inclusion cyst can be performed under topical anesthesia with 0.5% proparacaine, associated with subconjunctival infiltration of lidocaine around the cyst. A nontraumatic tweezer can be used to assist in removal of the cyst. A small incision is made and the blunt tip of scissors introduced between the cyst and Tenon capsule to separate the cyst from the surrounding tissue. After blunt dissection around the anterior aspect of the cyst, the next step is to carefully free the base of the cyst. Removing the cyst intact decreases chances of recurrence. If there is no conjunctiva remaining for primary closure over the wound, then the scleral bed may be left open or a conjunctival autograft or amniotic membrane may be used to cover the defect. The excised presumed cyst should be sent to pathology. | ||
'''''Check the videos below for a better understanding:''''' | '''''Check the videos below for a better understanding:''''' | ||
| Line 204: | Line 204: | ||
== Surgical Follow-up == | == Surgical Follow-up == | ||
The follow-up time for | The follow-up time varies for patients who undergo surgical excision of cysts. Figure 12 shows a patient 2 months after excision. | ||
== Complications of Surgical Excision == | == Complications of Surgical Excision == | ||
Because the cysts are thin walled, rupture is common during excision. Recurrence is the main postoperative concern. Careful and intact removal of the cyst is necessary to prevent recurrence.<ref name=":10" /> | |||
== Prognosis == | == Prognosis == | ||
The prognosis for a conjunctival inclusion cyst is usually very good. | |||
= Additional Resources = | = Additional Resources = | ||
Revision as of 15:16, March 10, 2025
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Conjunctival inclusion cysts are thin-walled, benign cystic lesions lined with a nonkeratinizing epithelium containing serous fluid. They are usually symptomless but can cause cosmetic disfigurement, reduced motility, foreign-body sensation, and dry eye due to unstable tear film when they increase in size.
Disease Entity
| Conjunctival Cyst |
|---|
| ICD-9 DATA 372.75 |
| ICD-10 DATA H11.44 |
Conjunctival Cyst is recognized by the following codes as per the International Classification of Diseases (ICD) nomenclature:
ICD-9
- ICD-9 DATA
- 372.75 Conjunctival Cysts
ICD-10
- ICD-10 DATA
- H11.44 Conjunctival Cysts
- H11.441 Conjunctival cysts, right eye
- H11.442 Conjunctival cysts, left eye
- H11.443 Conjunctival cysts, bilateral
- H11.449 Conjunctival cysts, unspecified eye
Other links
- Links:
Disease
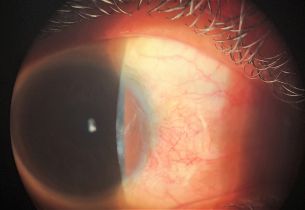
Inclusion cysts are benign cysts filled with clear serous fluid containing shed cells or mucoid material (Figure 1).[1] Inclusion cysts constitute 80% of all cystic lesions of the conjunctiva. The average age of onset is 47 and occurrence has no gender predilection.[2]
The cysts develop from an inclusion of the conjunctival epithelium into the substantia propria, forming a central cystic cavity due to epithelial cell proliferation. The cyst wall is composed of nonkeratinized lining epithelium and connective tissue.[3] Cysts can be primary or secondary and are usually asymptomatic. Treatment is required if discomfort develops or any impairment of function due to the size.[1]
Etiology
Primary conjunctival inclusion cysts are congenital. Secondary cysts can be spontaneous or, most commonly, due to inflammatory conditions of the conjunctiva,[4] such as pterygium, pingueculitis,[5] chronic keratoconjunctivitis,[6] or pyogenic granuloma,[7] or following ocular trauma[8] or surgery, such as cataract,[9] strabismus,[10] enucleation,[11] or scleral buckle placement.[12]
Risk Factors
The following causes have been cited for secondary conjunctival inclusion cysts:
- Inflammatory conditions of the conjunctiva (e.g., pterygium, pingueculitis,[5] chronic keratoconjunctivitis,[6] or pyogenic granuloma[7])
- Trauma[8]
- Surgery[9][10][11][12]
- Sub-Tenon anesthesia[13]
General Pathology
A cyst is an abnormal vesicle containing gas, fluid, or semisolid material, with a membranous framework. It can develop in various locations (e.g., eyelids, conjunctiva, anterior segment).[14] Posttraumatic or postsurgical cystic formation is often seen.[15]
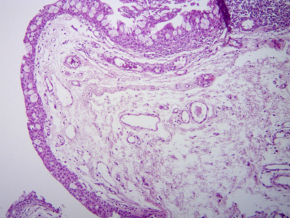
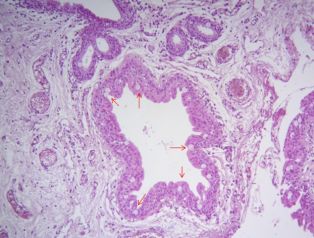
Cyst walls are composed of layers of nonkeratinized lining epithelium and connective tissue.[3]
Pathophysiology
Excessive invagination of the caruncular epithelium or fornix during embryonic development leads to the formation of primary inclusion cysts.[16] The presentation of these cysts varies from birth to old age.[4] Secondary inclusion cysts can occur naturally or under inflammatory conditions of the conjunctiva. Anything that causes detachment of a portion of conjunctival epithelium can cause a secondary inclusion cyst, such as surgery or trauma.[8] Sub-Tenon anesthesia is one such example of surgical trauma that can result in an inclusion cyst.[13]
In addition, it is known that cyst formation involves inflammatory processes, and, therefore, the immune system plays a role. Individual factors, such as autoimmune diseases, can also contribute to changes in the immune response resulting in differing degrees of cyst formation.[15]
Primary Prevention
Primary conjunctival inclusion cysts cannot be prevented, as they are a congenital disease. Avoiding conjunctival inflammatory processes and ocular trauma can reduce the chance of developing a secondary inclusion cyst.
Diagnosis
History
Many patients may be asymptomatic. Symptomatic patients may complain of a "round lesion" on the surface of the eye, which can be associated with an increased cyst size or foreign-body sensation.
Physical Examination
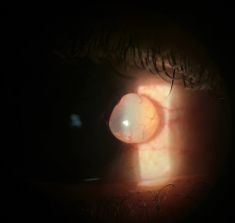
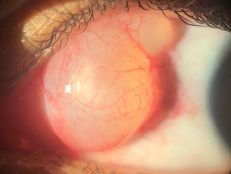
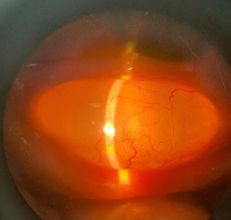
The diagnosis of a conjunctival inclusion cyst is essentially clinical (Figure 3A). Histopathology can confirm the diagnosis, but this is not usually necessary. Slit-lamp examination should include a measurement of the size of the cyst, assessment of the characteristics of its wall(s) and internal content, and whether it transilluminates (Figure 3B). The walls are usually thin and translucent. The fluid is usually clear; however, in rare cases, epithelial cells can deposit at the bottom of the cyst and form a pseudohypopyon (Figure 4). It is also important to evaluate the eye for signs of previous trauma, previous eye surgery, or active inflammatory processes.
Figure 3. Large conjunctival inclusion cyst in the lower conjunctiva.
Symptoms
Small conjunctival inclusion cysts are generally asymptomatic or only cause mild sensations indicating the presence of a foreign body. Larger cysts can cause pain, motility disturbance, visual defect or refractive error, and cosmetic concerns. Sometimes, the conjunctiva around the cysts can become injected due to dry eye or from the friction from the edge of a contact lens.
In a clinical-histopathological study that analyzed different varieties of conjunctival cysts,[4] the most common symptoms in decreasing order were as follows:
- Progressive increase in cyst size
- Cosmetic disfigurement
- Foreign-body sensation
- Proptosis
- Ocular motility restriction
- Blurred vision
Diagnostic Procedures
The diagnosis of a conjunctival inclusion cyst is usually clinical and may be confirmed by pathology; however, some imaging modalities can be useful for diagnosis. Corneal and conjunctival tumors can be visualized by anterior segment optical coherence tomography (AS-OCT) and ultrasound biomicroscopy (UBM), two noninvasive imaging techniques.[17] The use of imaging modalities is helpful for preoperative planning, surgical decision making, and to confirm cyst characteristics. Several studies on the quality of AS-OCT and UBM show that they provide useful information about the internal features, extension, size, and shape of the cysts.
Ultrasound Biomicroscopy
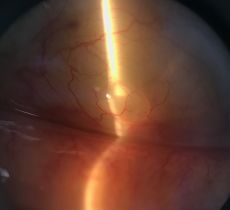
UBM is a high-resolution noninvasive tool of great value in diagnosing anterior chamber cystic lesions. UBM can be used to assess their content (whether hypodense or hyperreflective),[18] differentiating them from solid lesions.[19] Through UBM examination, it is possible to define whether the cyst has primary or secondary origin. Consuelo et al. observed that secondary implantation cysts have relatively thick walls and that their content may be hypodense (translucent) with several particles in suspension (probably desquamating epithelial cells [Figure 4]) or arranged in hyperreflective concentric layers corresponding to keratin lamellae. On the other hand, primary cystic lesions were characterized by a thin, highly reflective wall with hypodense content.[20] Figure 5. Conjunctival cyst after vitreoretinal surgery with silicone oil insertion. Ultrasound biomicroscopy 50 MHZ transducer, immersion technique.

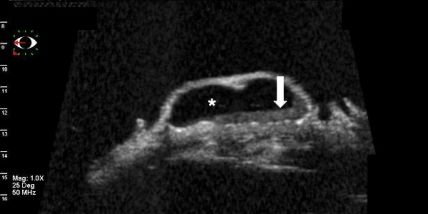
Anterior Segment Optical Coherence Tomography
AS-OCT is ideal for imaging structures from the surface of the eye to the level of the iris.[21] A disadvantage of AS-OCT is that it cannot visualize early pathological changes smaller than 5 μm, such as early dysplasia.[21][22] When comparing AS-OCT and UBM, AS-OCT is the better imaging technique for small cystic structures. This is especially useful for nevi as they often contain small cysts. In contrast, UBM is a better technique to determine tumor margins.
Figure 6. Asymptomatic bulbar conjunctival inclusion cyst at the nasal area.

Comparison of UBM and AS-OCT showed that UBM provided better tumor visualization and better resolution of the posterior margin. UBM also had better resolution for pigmented as well as nonpigmented tumors. However, AS-OCT showed better resolution of the anterior border and better resolution of the anterior segment anatomy. Posterior tumor shadowing was rarely found in UBM images and more common in AS-OCT. Image quality was good in UBM but less so in AS-OCT. The study showed that AS-OCT is superior to UBM for imaging conjunctival lesions, since AS-OCT offers higher resolution and conjunctival lesions are superficial and mostly not pigmented.[17][23]
Laboratory Test
Conjunctival inclusion cysts are diagnosed clinically; therefore, laboratory tests are not required.
Histopathology
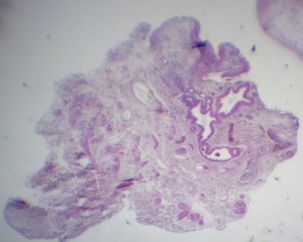
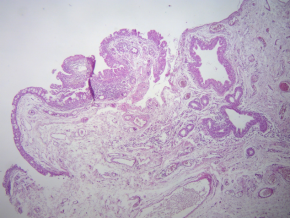
Figure 7. Histological sections of conjunctival inclusion cyst resection. Same patient from Figure 3.
The American Academy of Ophthalmology's Pathology Atlas contains a virtual microscopy image of Conjunctival Inclusion Cyst .
Differential Diagnosis
Benign
|
Premalignant
|
Check Eyewiki´s Conjunctival Epithelium Neoplasms page for differential diagnosis.
Management
Management can involve observation or intervention, depending on the size of the cyst and the patient's complaints.
General Treatment
Excision of a conjunctival inclusion cyst is the definitive treatment, although it is also possible to aspirate the cyst at the slit lamp. After informed consent is obtained, including a review of risks, benefits, and alternatives, the patient is positioned at the slit lamp with their head firmly positioned against the bar. The ocular surface may be cleaned with betadine. Under topical anesthesia of the ocular surface with 0.5% proparacaine, the cyst can be aspirated using a 27- or 30-gauge needle attached to a syringe. Care must be taken not to puncture conjunctival vessels or the globe during the procedure. Postoperative care may include a brief period of restrictions (i.e., swimming), the use of antibiotic drops, and/or a follow-up visit.
Medical Therapy
These cysts may disappear spontaneously; however, persistent cases require treatment. Surgical excision of the cyst is the best treatment, but thermal cautery under slit-lamp visualization[25] or YAG laser of the cyst has also be performed.[9][26]
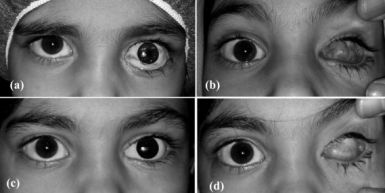
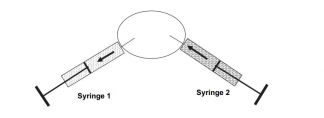
There are reports on the application of trichloroacetic acid (TCA) 20%-25% for superficial conjunctival cysts with high success rates, and reports of TCA 10%-20% injection into conjunctival cysts in ophthalmic and anophthalmic sockets,[27] as well as in children and multiple cysts, with 100% success (Figure 8).[28] Kothari et al. reported 2 cases of conjunctival inclusion cysts following strabismus surgery treated using a paired injection technique. The technique consists of using two 31-gauge insulin syringes, one empty syringe (syringe 1) and the other filled with 0.5 mL 70% isopropyl alcohol (syringe 2), simultaneously. The fluid from the cyst is aspirated into syringe 1 as the cyst is simultaneously filled with the alcohol from syringe 2 to prevent collapse. Once all the alcohol from syringe 2 is injected, aspiration (syringe 1) is stopped. The cyst remains inflated and filled with alcohol throughout the procedure. Thirty seconds later, the cyst is emptied by aspirating the alcohol with syringe 1 (Figure 9). There was no recurrence in a 9-month-follow-up.[24]
Nejat et al. treated 5 eyes with conjunctival cysts using an atmospheric low-temperature plasma (ALTP)–plasma-assisted noninvasive surgery (PANIS) method. First, a plasma spot was applied on the highest point of the cyst, and then other spots were applied in a spiral at the base of the cyst to debulk it. The conjunctival cysts were removed using the white handpiece of the plasma generator device. The authors concluded that ALTP can be used as a new approach for treating conjunctival cysts.[29]
Supplementary video of a case series paper "A Novel Approach to Treatment of Conjunctival Cyst Ablation using Atmospheric Low-Temperature Plasma" published in the open access journal Clinical Ophthalmology by Farhad Nejat, Khosrow Jadidi, Shiva Pirhadi et al.[29]
Surgery
Excision of the conjunctival inclusion cyst can be performed under topical anesthesia with 0.5% proparacaine, associated with subconjunctival infiltration of lidocaine around the cyst. A nontraumatic tweezer can be used to assist in removal of the cyst. A small incision is made and the blunt tip of scissors introduced between the cyst and Tenon capsule to separate the cyst from the surrounding tissue. After blunt dissection around the anterior aspect of the cyst, the next step is to carefully free the base of the cyst. Removing the cyst intact decreases chances of recurrence. If there is no conjunctiva remaining for primary closure over the wound, then the scleral bed may be left open or a conjunctival autograft or amniotic membrane may be used to cover the defect. The excised presumed cyst should be sent to pathology.
Check the videos below for a better understanding:
1) Surgery video from Figure's 1 patient.
2) This video illustrates the removal of a conjunctival inclusion cyst in inferior fornix, similar to the patient's cyst in Figure 2.
Reproduced from Dr. Neeraj Sharma, Aravind Eye Hospital
3) This video demonstrates the simple technique of conjunctival epithelial cyst removal without sutures.
Reproduced from Dr. Manju Meena, Pink City Eye and Retina Centre, Jaipur, India.
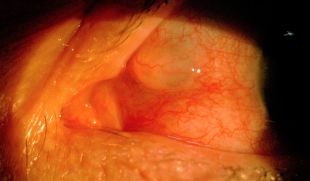
Surgical Follow-up
The follow-up time varies for patients who undergo surgical excision of cysts. Figure 12 shows a patient 2 months after excision.
Complications of Surgical Excision
Because the cysts are thin walled, rupture is common during excision. Recurrence is the main postoperative concern. Careful and intact removal of the cyst is necessary to prevent recurrence.[4]
Prognosis
The prognosis for a conjunctival inclusion cyst is usually very good.
Additional Resources
You can also visit AAO website to check out this multimedia.
- Here is a video showing a large, translucent cyst on the conjunctiva of the eye. This is most likely an epithelial inclusion cyst. These occur when epithelial cells are trapped under the conjunctiva (from prior surgery) and continue to produce mucinoid secretion. This was removed via excision with an attempt to remove the entire cyst wall to prevent recurrence. Reproduced from Tim Root Virtual Eye Professor. https://timroot.com/conjunctival-inclusion-cyst-video/
- For more illustrative photos check Eyerounds.org
References
- ↑ Jump up to: 1.0 1.1 Nath K, Gogi R, Zaidi N, Johri A. Cystic lesions of conjunctiva (a clinicopathogical study). Indian J Ophthalmol. 1983: 31(1):1-4.
- ↑ 2. Lu J, Chu F, Chen K. Conjunctival Inclusion Cyst. Hong Kong Journal of Emergency Medicine. 2013;20(3):184-185.
- ↑ Jump up to: 3.0 3.1 Johnson DW, Bartley GB, Garrity JA, Robertson DM. Massive epithelium-lined inclusion cysts after scleral buckle. Am J Ophthalmol. 1992;113(4): 439-42.
- ↑ Jump up to: 4.0 4.1 4.2 4.3 Thatte S, Jain J, Kinger M, Palod S, Wadhva J, Vishnoi A. Clinical study of histologically proven conjunctival cysts. Saudi J Ophthalmol. 2015;29(2):109-115.
- ↑ Jump up to: 5.0 5.1 Dias VG, Martins MP, Bezzon AKT, Aguni JS, Cavalheiro R. Cisto de inclusão conjuntival gigante associado a pterígio: relato de caso. Arq. Bras. Oftalmol. 2004;67(5):831-833.
- ↑ Jump up to: 6.0 6.1 Lee Seung-Won, Lee Seung-Chan, Jin Kyung-Hyun. Conjunctival inclusion cysts in long standing chronic vernal keratoconjunctivitis. Korean J Ophthalmol. 2007;21(4)
- ↑ Jump up to: 7.0 7.1 Suzuki K, Okisaka S, Nakagami T. The contribution of inflammatory cell infiltration to conjunctival inclusion cyst formation. Nippon Ganka Gakkai Zasshi. 2000;104(3):170-3.
- ↑ Jump up to: 8.0 8.1 8.2 Barishak Robert Y., Barrak E., Lazar M. Episcleral traumatic conjunctival inclusion cyst. BJO. 1977;61:29–301
- ↑ Jump up to: 9.0 9.1 9.2 Narayanappa S, Dayananda S, Dakshayini M, Gangasagara SB, Prabhakaran VC. Conjunctival inclusion cysts following small incision cataract surgery. Indian Journal of Ophthalmology. 2010;58(5):423-425.
- ↑ Jump up to: 10.0 10.1 Metz HS, Searl S, Rosenberg P, Sterns G. Giant orbital Cyst after strabismus surgery. J AAPOS. 1999;3(3):185-7.
- ↑ Jump up to: 11.0 11.1 Jünemann A, Holbach LM. Epitheliale Riesenimplantationszyste 50 jahre nach Enukleation ohne Orbitaimplantat. Kin Monatsbl Augenheilkd. 1998;212 (2):127-8.
- ↑ Jump up to: 12.0 12.1 Johnson DW, Bartley GB, Garrity JA, Robertson DM. Massive epithelium-lined inclusion cysts after scleral buckle. Am J Ophthalmol. 1992;113(4): 439-42.
- ↑ Jump up to: 13.0 13.1 Vishwanath M.R., Jain A. Inclusion cyst after subtenon. Br J Anaesthesia. 2005;95:825–826.
- ↑ Stedman TL. Cyst. In: Stedman TL. Stedman's medical dictionary. 26th ed. Baltimore: Williams & Wilkins; 1995. p.429.
- ↑ Jump up to: 15.0 15.1 Dias VG, Martins MP, Bezzon AKT, Aguni JS, Cavalheiro R. Cisto de inclusão conjuntival gigante associado a pterígio: relato de caso. Arquivos Brasileiros de Oftalmologia 2004; 67(5): 831-833.
- ↑ Imaizumi M, Nagata M, Matsumoto CS, Nakalruka K, Kachima K. Primary conjunctival epithelial cyst of orbit. Int Ophthalmol. 2007;27:269–271.
- ↑ Jump up to: 17.0 17.1 Janssens K, Mertens M, Lauwers N, de Keizer RJ, Mathysen DG, De Groot V. To Study and Determine the Role of Anterior Segment Optical Coherence Tomography and Ultrasound Biomicroscopy in Corneal and Conjunctival Tumors. J Ophthalmol. 2016;2016:1048760.
- ↑ Allemann N. Biomicroscopia ultra-sônica. Arq Bras Oftalmol. 1995;58:283-5
- ↑ Pavlin CJ. Practical application of ultrasound biomicroscopy. Can J Ophthalmol 1995;30:225-9.
- ↑ Consuelo ABD, Chojniak MMM, Allemann N. Ultrasound biomicroscopy and secondary epithelial downgrowth cysts of anterior chamber. Arq. Bras. Oftalmol.1998;61( 6 ): 656-661.
- ↑ Jump up to: 21.0 21.1 Garcia JPS, Rosen RB. Anterior segment imaging: optical coherence tomography versus ultrasound biomicroscopy. Ophthalmic Surgery Lasers and Imaging. 2008;39(6):476–484.
- ↑ Salim S. The role of anterior segment optical coherence tomography in glaucoma. Journal of Ophthalmology. 2012;2012:9.
- ↑ Bianciotto C, Shields CL, Guzman JM, et al. Assessment of anterior segment tumors with ultrasound biomicroscopy versus anterior segment optical coherence tomography in 200 cases. Ophthalmology. 2011;118(7):1297–1302.
- ↑ Jump up to: 24.0 24.1 Kothari M. A novel method for management of conjunctival inclusion cysts following strabismus surgery using isopropyl alcohol with paired injection technique. J AAPOS. 2009 Oct;13(5):521-2.
- ↑ Hawkins AS, Hamming NA. Thermal cautery as a treatment for conjunctival inclusion cyst after strabismus surgery. J AAPOS. 2001 Feb;5(1):48-9.
- ↑ de Bustros S, Michels RG. Treatment of acquired epithelial inclusion cyst of the conjunctiva using the YAG laser. Am J Ophthalmol. 1984 Dec 15;98(6):807-8.
- ↑ Gallagher D, Power B, Hughes E, Fulcher T. Management of orbital conjunctival epithelial inclusion cyst using trichloroacetic acid (20%) in an outpatient setting. Orbit. 2020 Apr;39(2):147-149. doi: 10.1080/01676830.2019.1611882. Epub 2019 May 20. PMID: 31106628.
- ↑ Bagheri A, Shahraki K, Yazdani S. Trichloroacetic acid 10% injection for treatment of conjunctival inclusion cysts. Orbit. 2020 Apr;39(2):107-111.
- ↑ Jump up to: 29.0 29.1 Nejat F, Jadidi K, Pirhadi S, Adnani SY, Nabavi NS, Nejat MA. A Novel Approach to Treatment of Conjunctival Cyst Ablation Using Atmospheric Low-Temperature Plasma. Clin Ophthalmol. 2020;(14):2525-2532.