Conjunctivochalasis: Difference between revisions
m (New picture) |
|||
| Line 77: | Line 77: | ||
== Clinical diagnosis == | == Clinical diagnosis == | ||
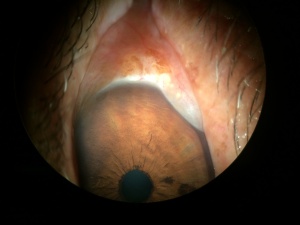
The diagnosis is Clinical. The Conjunctiva will look corrugated or pleated, overlying the palpebral border in some extent, looking loose over the globe. The conjunctival "movement" over the globe will be seen easily pressing it with the eyelid and moving it up and down. The tear film drainage pass from temporal to nasal will be blocked by the conjunctiva bulging, so the natural tear composition will be altered because impaired tear flow. The Patient will have some "vague" complaints but the clear sensation that "something is wrong". | |||
== Diagnostic procedures == | == Diagnostic procedures == | ||
Revision as of 13:54, February 8, 2016
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Conjunctivochalasis is defined as a redundant, nonedematous conjunctiva that causes a wide variety of symptoms ranging from completely asymptomatic, to worsening of an unstable tear film, and when severe, a real mechanical disruption of tear flow.
Due to the fact that conjunctivochalasis can be asymptomatic, it is often overlooked by the physician and it is classified as a normal variant of the eye due to the aging process. However, it must be kept in mind as a possibility for the origin of ocular irritation and tearing; and when severe enough it may be a cause a blurred vision, mucous discharge, dryness, ocular fatigue, subconjunctival hemorrhage, and eye stiffness upon awakening. This redundant conjunctiva can often be seen and frequently overlooked after tightening of lateral canthal tendon in inferior Blepharoplasty.
Conjunctivochalasis is usually bilateral, involving most commonly the inferotemporal conjunctiva, that may cause disruption of the inferior tear meniscus. It may present as loose superior conjunctiva, although it is less common.
The symptoms are nonspecific and the onset may be insidious and uncertain, often confused with dry eye ones. Initial symptoms include foreign body sensation, burning, dry eyes and discomfort. As the entity progress and conjunctival redundancy increases, the puncta can be blocked, leading to epiphora and blurred vision.
Slit biomiocroscopy shows a prolapse of the conjunctiva over the lower lid margin in temporal, medial or nasal regions. This prolapsed conjunctiva causes a disruption of tear movement and outflow through the inferior lacrimal punctum, resulting in epiphora (constant tearing).
Confusion arises in the management of this entity because there are other diseases and conditions that produce tearing and ocular irritation and must be ruled out as a causative agent of the tear flow disruption and tear instability (Dry Eye Syndrome, Keratoconjunctivitis Sicca, ocular allergies, thyroid eye disease, among others).
Disease Entity
Add text here
Disease
Add text here
Etiology
Not determined but associated with age or allergic conjunctivitis (rubbing).
Risk Factors
Add text here
General Pathology
Usually not biopsied.
Pathophysiology
No true etiology has been determined. Francis et al,. In a prospective clinical and histopathological study of 29 patients, 22 showed normal conjunctival histology, while 4 specimens showed inflammatory changes, and 3 specimens showed elastosis. They concluded and hypothesized that the etiology is multifactorial, including local trauma, UV radiation and delayer tear clearance as triggers of the disease. Watanabe et al. Demonstrated microscopic telangiectasia of the subconjunctiva in 4 of 39 specimens taken from patients with severe conjunctivochalasis, with no evidence of inflammation. They also noted fragmented elastic fibers and sparse assemblages of collagen fibers in 44 specimens. They concluded that mechanical forces between the lower eyelid and conjunctiva gradually impaired lymphatic flow, resulting in lymphatic dilation and clinically redundant conjunctiva. Even though there is little to none histopathologic evidence to support inflammation as a major contributor to conjunctivochalasis, mechanistic evidence suggest a shift in the normal balance of the conjunctival matrix metalloproteinases (MMPs) and tissue inhibitors (TIMPs); enzymes that degrade extracellular matrix. Li et al. Showed overexpression of MMP-1 and MMP-3 mRNA in tissue cultured conjunctivochalasis fibroblasts, versus normal human conjunctival fibroblasts. Further studies showed that inflammatory mediators TNF-å and IL-1ß may increase the expression of MMP-1 and MMP-3 in conjunctivochalasis fibroblasts. Other inflammatory cytokines were also found in increased amounts in tear film of conjunctivochalasis patients (IL6 and IL8). After these observations, thy concluded that the interaction of MMPs and their inhibitors, in a broken equilibrium may lead to a manifestation of a redundant conjunctiva with increased laxity. Huan et al studied whether conjunctivochalasis interferes with tear flow from the fornix to the tear meniscus and depletes de fornix tear reservoir. It was a study of 24 patients con conjunctivochalasis (8 asymptomatic and 16 symptomatic); of which 9 of them underwent operative correction. The studied found that the recovery rate of the tear meniscus was signifcantly slower in symptomatic than asymptomatic patients when compared to normal subjects. Deepening of the inferior fornix by removing degenerated Tenon’s and perform a fornix reconstruction with amniotic membrane improved the recovery rate in symptomatic patients. They concluded then that the tear reservoir in the fornix rapidly replenishes the meniscus under normal circumstances, but patients with conjunctivochalasis are affected not only in the formation of normal tear meniscus, but blocking the normal tear movement from the fornix.
Primary prevention
Not known.
Diagnosis
Clinical
History
Add text here
Physical examination
Slit biomiocroscopy shows a prolapse, pleating or folding of the conjunctiva over the lower lid margin in temporal, medial or nasal regions. Redundant or pleated conjuntiva may easily be seen over the lower lid margin and make the diagnosis.
Signs
Add text here
Symptoms
You can hear a miriad of vague symptoms like sore, tired, uncomfortable eyes, stinging, burning sensation etc. the most important clue is that the symptoms are vague and the treatments have been several without clear results.
Clinical diagnosis
The diagnosis is Clinical. The Conjunctiva will look corrugated or pleated, overlying the palpebral border in some extent, looking loose over the globe. The conjunctival "movement" over the globe will be seen easily pressing it with the eyelid and moving it up and down. The tear film drainage pass from temporal to nasal will be blocked by the conjunctiva bulging, so the natural tear composition will be altered because impaired tear flow. The Patient will have some "vague" complaints but the clear sensation that "something is wrong".
Diagnostic procedures
OCT images from the anterior segment may be helpful to evaluate the tear meniscus and gross anatomy of the lateral canthus
Laboratory test
None are necessary
Differential diagnosis
Dry eye Syndrome, Sjögren Disease, Meibomian Gland Dysfunction, among others
Management
Management must be individualize according to the severity and discomfort of each patient. No treatment is needed if the patient is asymptomatic. If a patient becomes mildly symptomatic, the clinical can start therapy with trials of lubrication and courses of topical corticosteroids. If patients continue to be in discomfort despite the medical management, surgical options can be taken into account.
The most commonly employed procedure is conjunctival excision and resection, incising in a semilunar manner 5 mm posterior to the limbus; or performing a elliptical excision of the redundant conjunctiva and closed with an absorbable suture or with fibrin glue.There are several other techniques described as conjunctival fixation to the sclera with a 6-0 Vicryl suture, the use of a amniotic membrane, among others
General treatment
Artificial tears may give a temporary relieve
Medical therapy
Artificial tears and topical steroids may be helpful if mild presentation
Medical follow up
Add text here
Surgery
.Another procedure has been described using the thermocautery. Where under topical anesthesia, the redundant conjunctiva is grasped gently with a forceps and them cautery is applied over this redundant conjunctiva to cause a contraction of the tissue to allow a correct tear outflow
Surgical follow up
Complications
Dry eye symptoms, burning sensation, and when pain when severe presentation
Prognosis
Good with the correct treatment according to each patient's symptoms
Additional Resources
Add text here
References
Holland, E; Mannis, M; Barry, W. “Ocular Surface Disease” (2013) Saunders Elsevier
Huang, Y; Sheha, H; Tseng, S”Conjunctivochalasis Interferes with Tear Flor from Fornix to Tear Meniscus” (2013). Ophthalmology. 120:1681-1687. Elsevier