Adie Pupil: Difference between revisions
m (→update infobox) |
(Reference formatting to AMA style.) |
||
| (48 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
{{Article | {{Article | ||
|Authors=Alexander.L.Ringeisen, Kevin.Rolnick | |Authors=Alexander.L.Ringeisen, Andrew.G.Lee, Eric.L.Crowell, Junru.Yan, Nita.Bhat, Shruthi.harish, Kevin.Rolni | ||
|Additional contributors=Andrew.G.Lee, Brad.H.Feldman.DEC, Eric.L.Crowell, Kevin.Rolnick, Koushik.Tripathy, Nita.Bhat, Shruthi.harish | |||
|Category=Neuro-ophthalmology/Orbit | |Category=Neuro-ophthalmology/Orbit | ||
|Assigned editor= | |Assigned editor=Nagham.A.Zubidi | ||
|Date reviewed= | |Reviewer=Nagham.A.Zubidi | ||
|Date reviewed=October 8, 2024 | |||
|Article status=Up to Date | |Article status=Up to Date | ||
|Meta description=Adie tonic pupil, known as Adie’s Syndrome or Holmes-Adie Syndrome, is a disorder in which there is parasympathetic denervation of the afflicted pupil resulting in a poor light reaction but better and tonic near constriction. | |||
}} | }} | ||
{{Infobox disease | {{Infobox disease | ||
| Line 10: | Line 13: | ||
| DiseasesDB = 29742 | | DiseasesDB = 29742 | ||
| ICD9 = | | ICD9 = | ||
| ICD10={{ICD10|H|57|0| | | ICD10={{ICD10|H|57|0|5}} | ||
| OMIM = | | OMIM = | ||
| MeshID = D000270 | | MeshID = D000270 | ||
| Line 16: | Line 19: | ||
}} | }} | ||
= Disease Entity = | |||
Tonic Pupil ICD-10: H57.051 (right), H57.052 (left), H57.053 (bilateral) | |||
== Disease == | |||
Adie tonic pupil (Adie syndrome or Holmes-Adie syndrome) is a disorder in which there is parasympathetic denervation of the afflicted pupil resulting in a poor light but better and tonic near constriction. The affected pupil, either unilateral or bilateral, typically initially appears abnormally dilated at rest and has poor or sluggish pupillary constriction in bright light. Constriction is usually more notable with the near reaction, and the pupil typically remains tonically constricted with slow redilation and segmental paralysis of the iris sphincter. Patients may also present with decreased deep tendon reflexes in the full Holmes-Adie syndrome.<ref name="leavitt1">Leavitt JA, Wayman LL, Hodge DO, Brubaker RF. Pupillary response to four concentrations of pilocarpine in normal subjects: application to testing for Adie tonic pupil. ''Am J Ophthalmol.'' 2002;133:333-336.</ref> | |||
The entity is named after William John Adie, an Australian neurologist who extensively described its features. However, it may be noted that the tonic pupil was initially described in 1931 nearly synchronously by Adie, Morgan, Symonds, and Holmes.<ref name="adie2">Adie WJ. Pseudo-Argyll Robertson pupils with absent tendon reflexes: a benign disorder simulating tabes dorsalis. ''Br Med J.'' 1931;1(3673):928-930.</ref><ref name="morgan3">Morgan OG, Symonds CP. Internal ophthalmoplegia with absent tendon-jerks. ''Proc R Soc Med.'' 1931;24(7):867-869.</ref><ref name="holmes4">Holmes G. Partial iridoplegia with symptoms of other diseases of the nervous system. ''Trans Ophthalmol Soc UK.'' 1931;51:209-228.</ref> | |||
[[File:AA0 Addies LN.jpeg|thumb|Left Adie pupil. A, The left pupil reacts poorly to direct light stimulus, whereas the right pupil demonstrates a strong consensual response. B, Both pupils constrict upon fixation on a near target. The response of the left pupil to near effort is better than its response to light (light–near dissociation). C, After refixating on a distant target, the right pupil quickly redilates. The left pupil is slow to redilate (it is smaller than the right pupil), a sign of tonicity. (Courtesy of Lanning B. Kline, MD.) © 2025 American Academy of Ophthalmology<ref>American Academy of Ophthalmology. Left Adie tonic pupil. Accessed March 6, 2025. https://www.aao.org/education/image/left-adie-tonic-pupil </ref>]] | |||
== | == Epidemiology == | ||
Adie tonic pupil has a prevalence of 2 per 1000 population and occurs in a 2.6:1 female-to-male ratio, with an average age of onset of 32 years.<ref name="thompson5">Thompson HS. Adie’s syndrome: some new observations. ''Trans Am Ophthalmol Soc.'' 1977;75:587-626.</ref> Approximately 80% of Adie tonic pupils are unilateral, and bilateral involvement typically has an incidence of 4% per year.<ref name="thompson5"/> | |||
== General Pathology == | |||
Damage to the parasympathetic ciliary ganglion may result in a tonic pupil. The parasympathetic fibers of the eye travel with the third cranial nerve to synapse at the ciliary ganglion before innervating the iris and the ciliary body. Typically, there are 30 times the number of axons supplying the ciliary body compared to those for the iris. After damage to the ciliary ganglion occurs, a process known as denervation supersensitivity occurs by which postsynaptic receptors are upregulated to facilitate reinnervation. However, the reinnervation process is often aberrant and fibers intended for the ciliary body may end up targeted to the pupil, a process known as aberrant regeneration.<ref name="mcGee6">McGee S. The pupils. In: ''Evidence-Based Physical Diagnosis.'' 3rd ed. Elsevier; 2012:161-180.</ref> As a result, patients develop light–near dissociation of the pupil by which the near accommodation produces more miosis compared to response to light, the reaction which is tonic. The tonic reaction is the result of the iris sphincter supersensitivity to acetylcholine. Roughly 80% of cases are unilateral but can become bilateral (4% chance per year).<ref name="thompson5"/> | |||
== Etiology == | |||
Most cases of tonic pupil are idiopathic and referred to as Adie tonic pupil. However, a tonic pupil can also be caused by viral infection, trauma, vasospasm due to migraine, ocular surgery, and tumors, among other potential causes. The ciliary ganglion can also be affected in other systemic autonomic or peripheral neuropathies to result in the tonic pupil, such as [[Ross_Syndrome|Ross syndrome]] and Harlequin syndrome.<ref name="shin7">Shin RK, Galetta SL, Ting TY, Armstron K, Bird SJ. Ross syndrome plus: beyond horner, Holmes-Adie, and harlequin. ''Neurology.'' 2000;55:1841-1846.</ref> | |||
= Diagnosis = | |||
== Physical Examination == | |||
Patients with Adie tonic pupil typically present with an incidental finding of anisocoria. Initially, the tonic pupil appears larger than the pupil in the unaffected eye. However, it is important to note that the affected pupil tends to become smaller over time with chronic Adie tonic pupil. Slit-lamp examination of the pupil often shows sectoral palsy of the iris sphincter, with vermiform movements of the pupillary margin.<ref name="aao8">American Academy of Ophthalmology. Pupil efferent defects. Anisocoria: Pupil Efferent Defects. Focal Points - Excerpt. Accessed September 26, 2024. https://www.aao.org/education/focalpoints</ref> To correctly form a diagnosis, it is important to examine the degree of anisocoria in the light and in the dark and to examine the pupillary reaction to light and to accommodation. Examination reveals anisocoria greater in the light than in the dark, indicating dysfunction of the parasympathetically innervated iris sphincter muscle in the affected eye (large pupil is abnormal). | |||
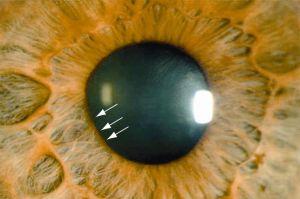
[[File:AA0 54271.jpg|thumb|Sectoral palsy of the iris sphincter in Adie pupil. The pupil is not round. The sphincter contraction is strongest along its superior sector, seen as a puckering or "bunching up" of the iris stroma. The sphincter is paralyzed between the 7 o'clock and 9 o'clock sectors (arrows); the adjacent area of iris stroma appears thinned and flattened. (Courtesy of Rod Foroozan, MD.) © 2025 American Academy of Ophthalmology<ref>American Academy of Ophthalmology. Adie tonic pupil. Accessed March 6, 2025. https://www.aao.org/education/image/adie-tonic-pupil </ref>]] | |||
= | Upon initial examination, patients with Adie tonic pupil will demonstrate increased pupillary constriction to accommodation compared to light, also known as light–near dissociation. However, this finding is not specific to Adie tonic pupil and can also be found in patients with bilateral anterior afferent visual pathway disease, Argyll Robertson pupil, diabetes, or dorsal midbrain lesions.<ref name="lee">Lee AG. Tonic pupil. UpToDate. Accessed September 26, 2024. https://www.uptodate.com/contents/tonic-pupil </ref> The affected pupil can be distinguished from these other causes by testing the tonicity of the constriction. An Adie tonic pupil, due to the acetylcholine sensitivity developed during the reinnervation process, typically has a strong and tonic pupillary response with a slow and sustained relaxation after constriction compared to the normal eye.<ref name="aao8" /> | ||
== Symptoms == | |||
Patients with Adie tonic pupil may present with symptoms related to their sphincter dysfunction, such as photophobia and difficulty adapting to the dark. Ciliary muscle dysfunction may also present with symptoms of blurry vision both for near and far vision and during transitions and anisocoria.<ref name="hopeross9">Hope-Ross M, Buchanan TAS, Archer DB, Allen JA. Autonomic function in Holmes Adie Syndrome. ''Eye (Lond).'' 1990;4(Pt 4):607-612. doi:10.1038/eye.1990.85</ref> | |||
== | == Diagnostic Procedures == | ||
The denervated sphincter muscles can show increased sensitivity to diluted pilocarpine (0.125%) due to upregulation of receptors in about 80% of cases. Dilute pilocarpine (0.125% or 0.1%) can be made by diluting readily available commercial 1% solution with sterile saline.<ref name="leavitt1"/> After 30-60 minutes, the affected pupil will constrict more than the normal pupil. This test, however, is not specific for Adie tonic pupil where there is postganglionic parasympathetic denervation. Supersensitivity has also been demonstrated in some preganglionic oculomotor nerve disorders.<ref name="leavitt1"/> Absent supersensitivity does not necessarily rule out a diagnosis of Adie tonic pupil, especially in the acute setting, as regeneration of nerves may not have yet occurred. | |||
== Differential Diagnosis and Additional Tests == | |||
Adie tonic pupil is most commonly an idiopathic condition. When faced with a picture of anisocoria, tonic pupil, or light–near dissociation, it is important to rule out other potentially more serious diagnoses:<ref name="mcGee6"/> | |||
# Orbital trauma | |||
# Orbital tumor | |||
# Intracranial hemorrhage/stroke with third nerve palsy | |||
# Varicella-zoster infection (ophthalmic branch of trigeminal nerve) | |||
# Syphilis (Argyll Robertson pupil; generally bilateral, small, brisk redilation) | |||
# Miller Fisher syndrome | |||
# Charcot-Marie-Tooth disease | |||
# Systemic dysautonomia ([[Ross_Syndrome|Ross syndrome]]) | |||
# Diabetes | |||
# Chronic alcoholism | |||
# Multiple sclerosis | |||
# Herpes zoster | |||
# Neurosarcoidosis | |||
<br> | |||
When considering these additional potential diagnoses, it may be valuable to obtain syphilis serologies and check for a history of diabetes, trauma, or neurologic diseases. | |||
= Management = | |||
== Treatment and Prognosis == | |||
Adie tonic pupil is a benign condition, and patients generally only require reassurance. However, they may experience photophobia and blurry vision. Accommodative paresis can resolve with time, ranging from months to years. However, patients may experience increased light–near dissociation over time because the pupil's reaction to light does not typically recover.<ref name="lee"/> | |||
In general, treatment is not required for Adie tonic pupil, but dilute topical pilocarpine or physostigmine can be used for symptomatic relief in cases with severe photophobia. It must be noted that these medications can precipitate ciliary spasm or brow ache, worsen anisocoria, or induce nearsightedness.<ref name="thompson5" /> In patients with persistent accommodative paresis, frosted bifocal segments may be used to correct vision. If an underlying systemic cause for the tonic pupil is suspected, patients should have treatment directed toward their systemic neuropathies. | |||
= Additional Resources = | = Additional Resources = | ||
* American Academy of Ophthalmology. | * Boyd K, DeAngelis KD. [https://www.aao.org/eye-health/diseases/anisocoria-5 Anisocoria]. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/diseases/anisocoria-5. Accessed November 17, 2022. | ||
* Porter D, DeAngelis KD. [https://www.aao.org/eye-health/diseases/adies-pupil-list Adie's Pupil]. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/diseases/adies-pupil-list. Accessed November 17, 2022. | |||
= References | = References = | ||
<references /> | <references /> | ||
Latest revision as of 11:20, March 25, 2025
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Tonic Pupil ICD-10: H57.051 (right), H57.052 (left), H57.053 (bilateral)
Disease
Adie tonic pupil (Adie syndrome or Holmes-Adie syndrome) is a disorder in which there is parasympathetic denervation of the afflicted pupil resulting in a poor light but better and tonic near constriction. The affected pupil, either unilateral or bilateral, typically initially appears abnormally dilated at rest and has poor or sluggish pupillary constriction in bright light. Constriction is usually more notable with the near reaction, and the pupil typically remains tonically constricted with slow redilation and segmental paralysis of the iris sphincter. Patients may also present with decreased deep tendon reflexes in the full Holmes-Adie syndrome.[1]
The entity is named after William John Adie, an Australian neurologist who extensively described its features. However, it may be noted that the tonic pupil was initially described in 1931 nearly synchronously by Adie, Morgan, Symonds, and Holmes.[2][3][4]

Epidemiology
Adie tonic pupil has a prevalence of 2 per 1000 population and occurs in a 2.6:1 female-to-male ratio, with an average age of onset of 32 years.[6] Approximately 80% of Adie tonic pupils are unilateral, and bilateral involvement typically has an incidence of 4% per year.[6]
General Pathology
Damage to the parasympathetic ciliary ganglion may result in a tonic pupil. The parasympathetic fibers of the eye travel with the third cranial nerve to synapse at the ciliary ganglion before innervating the iris and the ciliary body. Typically, there are 30 times the number of axons supplying the ciliary body compared to those for the iris. After damage to the ciliary ganglion occurs, a process known as denervation supersensitivity occurs by which postsynaptic receptors are upregulated to facilitate reinnervation. However, the reinnervation process is often aberrant and fibers intended for the ciliary body may end up targeted to the pupil, a process known as aberrant regeneration.[7] As a result, patients develop light–near dissociation of the pupil by which the near accommodation produces more miosis compared to response to light, the reaction which is tonic. The tonic reaction is the result of the iris sphincter supersensitivity to acetylcholine. Roughly 80% of cases are unilateral but can become bilateral (4% chance per year).[6]
Etiology
Most cases of tonic pupil are idiopathic and referred to as Adie tonic pupil. However, a tonic pupil can also be caused by viral infection, trauma, vasospasm due to migraine, ocular surgery, and tumors, among other potential causes. The ciliary ganglion can also be affected in other systemic autonomic or peripheral neuropathies to result in the tonic pupil, such as Ross syndrome and Harlequin syndrome.[8]
Diagnosis
Physical Examination
Patients with Adie tonic pupil typically present with an incidental finding of anisocoria. Initially, the tonic pupil appears larger than the pupil in the unaffected eye. However, it is important to note that the affected pupil tends to become smaller over time with chronic Adie tonic pupil. Slit-lamp examination of the pupil often shows sectoral palsy of the iris sphincter, with vermiform movements of the pupillary margin.[9] To correctly form a diagnosis, it is important to examine the degree of anisocoria in the light and in the dark and to examine the pupillary reaction to light and to accommodation. Examination reveals anisocoria greater in the light than in the dark, indicating dysfunction of the parasympathetically innervated iris sphincter muscle in the affected eye (large pupil is abnormal).
Upon initial examination, patients with Adie tonic pupil will demonstrate increased pupillary constriction to accommodation compared to light, also known as light–near dissociation. However, this finding is not specific to Adie tonic pupil and can also be found in patients with bilateral anterior afferent visual pathway disease, Argyll Robertson pupil, diabetes, or dorsal midbrain lesions.[11] The affected pupil can be distinguished from these other causes by testing the tonicity of the constriction. An Adie tonic pupil, due to the acetylcholine sensitivity developed during the reinnervation process, typically has a strong and tonic pupillary response with a slow and sustained relaxation after constriction compared to the normal eye.[9]
Symptoms
Patients with Adie tonic pupil may present with symptoms related to their sphincter dysfunction, such as photophobia and difficulty adapting to the dark. Ciliary muscle dysfunction may also present with symptoms of blurry vision both for near and far vision and during transitions and anisocoria.[12]
Diagnostic Procedures
The denervated sphincter muscles can show increased sensitivity to diluted pilocarpine (0.125%) due to upregulation of receptors in about 80% of cases. Dilute pilocarpine (0.125% or 0.1%) can be made by diluting readily available commercial 1% solution with sterile saline.[1] After 30-60 minutes, the affected pupil will constrict more than the normal pupil. This test, however, is not specific for Adie tonic pupil where there is postganglionic parasympathetic denervation. Supersensitivity has also been demonstrated in some preganglionic oculomotor nerve disorders.[1] Absent supersensitivity does not necessarily rule out a diagnosis of Adie tonic pupil, especially in the acute setting, as regeneration of nerves may not have yet occurred.
Differential Diagnosis and Additional Tests
Adie tonic pupil is most commonly an idiopathic condition. When faced with a picture of anisocoria, tonic pupil, or light–near dissociation, it is important to rule out other potentially more serious diagnoses:[7]
- Orbital trauma
- Orbital tumor
- Intracranial hemorrhage/stroke with third nerve palsy
- Varicella-zoster infection (ophthalmic branch of trigeminal nerve)
- Syphilis (Argyll Robertson pupil; generally bilateral, small, brisk redilation)
- Miller Fisher syndrome
- Charcot-Marie-Tooth disease
- Systemic dysautonomia (Ross syndrome)
- Diabetes
- Chronic alcoholism
- Multiple sclerosis
- Herpes zoster
- Neurosarcoidosis
When considering these additional potential diagnoses, it may be valuable to obtain syphilis serologies and check for a history of diabetes, trauma, or neurologic diseases.
Management
Treatment and Prognosis
Adie tonic pupil is a benign condition, and patients generally only require reassurance. However, they may experience photophobia and blurry vision. Accommodative paresis can resolve with time, ranging from months to years. However, patients may experience increased light–near dissociation over time because the pupil's reaction to light does not typically recover.[11]
In general, treatment is not required for Adie tonic pupil, but dilute topical pilocarpine or physostigmine can be used for symptomatic relief in cases with severe photophobia. It must be noted that these medications can precipitate ciliary spasm or brow ache, worsen anisocoria, or induce nearsightedness.[6] In patients with persistent accommodative paresis, frosted bifocal segments may be used to correct vision. If an underlying systemic cause for the tonic pupil is suspected, patients should have treatment directed toward their systemic neuropathies.
Additional Resources
- Boyd K, DeAngelis KD. Anisocoria. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/diseases/anisocoria-5. Accessed November 17, 2022.
- Porter D, DeAngelis KD. Adie's Pupil. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/diseases/adies-pupil-list. Accessed November 17, 2022.
References
- ↑ 1.0 1.1 1.2 Leavitt JA, Wayman LL, Hodge DO, Brubaker RF. Pupillary response to four concentrations of pilocarpine in normal subjects: application to testing for Adie tonic pupil. Am J Ophthalmol. 2002;133:333-336.
- ↑ Adie WJ. Pseudo-Argyll Robertson pupils with absent tendon reflexes: a benign disorder simulating tabes dorsalis. Br Med J. 1931;1(3673):928-930.
- ↑ Morgan OG, Symonds CP. Internal ophthalmoplegia with absent tendon-jerks. Proc R Soc Med. 1931;24(7):867-869.
- ↑ Holmes G. Partial iridoplegia with symptoms of other diseases of the nervous system. Trans Ophthalmol Soc UK. 1931;51:209-228.
- ↑ American Academy of Ophthalmology. Left Adie tonic pupil. Accessed March 6, 2025. https://www.aao.org/education/image/left-adie-tonic-pupil
- ↑ 6.0 6.1 6.2 6.3 Thompson HS. Adie’s syndrome: some new observations. Trans Am Ophthalmol Soc. 1977;75:587-626.
- ↑ 7.0 7.1 McGee S. The pupils. In: Evidence-Based Physical Diagnosis. 3rd ed. Elsevier; 2012:161-180.
- ↑ Shin RK, Galetta SL, Ting TY, Armstron K, Bird SJ. Ross syndrome plus: beyond horner, Holmes-Adie, and harlequin. Neurology. 2000;55:1841-1846.
- ↑ 9.0 9.1 American Academy of Ophthalmology. Pupil efferent defects. Anisocoria: Pupil Efferent Defects. Focal Points - Excerpt. Accessed September 26, 2024. https://www.aao.org/education/focalpoints
- ↑ American Academy of Ophthalmology. Adie tonic pupil. Accessed March 6, 2025. https://www.aao.org/education/image/adie-tonic-pupil
- ↑ 11.0 11.1 Lee AG. Tonic pupil. UpToDate. Accessed September 26, 2024. https://www.uptodate.com/contents/tonic-pupil
- ↑ Hope-Ross M, Buchanan TAS, Archer DB, Allen JA. Autonomic function in Holmes Adie Syndrome. Eye (Lond). 1990;4(Pt 4):607-612. doi:10.1038/eye.1990.85

