All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Traumatic ectopia lentis, or displacement of the lens, can either be complete or partial. Complete dislocation of the lens is also known as luxation while partially displaced lens is known as subluxation.
Etiology
Trauma is the most common cause of a dislocated lens.[1] Other etiologies of lens dislocation include congenital disorders such as congenital aniridia, Ehlers-Danlos syndrome, homocystinuria, or Marfan’s syndrome, which are further described here.
Pathophysiology
The mechanism in blunt traumatic lens dislocation is due to a compressional anterior-posterior force of the cornea and anterior sclera causing rapid compensatory equatorial expansion of the globe. As a result, the zonular fibers, which anchor the lens to the eye, may become stretched or damaged. [2][3] Partial zonular dialysis may lead to subluxation while complete zonular rupture leads to complete luxation. Dislocation can occur anteriorly or posteriorly, each managed differently which is further discussed below.
Diagnosis
History and Physical Exam
Patients with traumatic lens dislocation may present with a wide variety of symptoms, including vision changes, eye pain, and monocular diplopia. Lens dislocation may accompany other sequelae of ocular trauma including open globe injury and retinal tears or detachments, so it is important to conduct a thorough eye exam to rule out other ocular trauma. In patients with elevated intraocular pressure following blunt force trauma to the eye, anterior displacement of the lens should be considered. If possible, an ophthalmologic exam with a slit lamp should be performed. In some instances, the lens may appear to be obviously displaced on dilated eye exam, but in other cases the findings may be more subtle. A shortened posterior chamber or phacodonesis (shaking of the lens with eye movements) may be the only signs indicating a traumatic lens displacement. Additionally, iridodonesis, or vibration of the iris with rapid eye movements, may be suggestive of lens dislocation posteriorly.
Diagnostic Procedures
In cases where a complete ophthalmologic exam is not able to be performed, a computed tomography (CT) scan or ultrasound are common imaging modalities that may be used for diagnosis. CT may be preferable for diagnosis, especially if eye compression needs to be avoided in cases such as suspected globe rupture.[4] The lentiform shape of the lens is easily identified on CT and a “floating lens” sign is indicative of posterior lens dislocation.[5] The “floating lens” sign is described as the combination of the lens located posteriorly in the vitreous on axial CT with the patient supine, and a lens located superiorly in the vitreous on coronal CT with the patient supine and the neck hyperextended. Although considered an alternative, bedside ultrasound is commonly used in emergent presentations to rapidly and accurately diagnose lens dislocation. It is especially useful in resource-limited settings.
Ultrasound biomicroscopy (UBM) can also help identify zonular disruption, with one study finding that 42.9% of patients with blunt ocular trauma had UBM evidence of zonular damage.[6]
Complications
Without lens removal, traumatic lens dislocation can lead to complications such as secondary glaucoma, corneal decompensation, and uveitis.[2] Traumatic lens subluxation can also be associated with other ocular trauma, including traumatic cataract and retinal breaks or detachments.
Secondary glaucoma
Anterior lens subluxation can cause acute angle closure due to pupillary block, with prolonged angle closure leading to chronic angle closure from peripheral anterior synechiae. In one retrospective series[7], 24 of 41 eyes (58.5%) with at least 6 clock hours of traumatic zonulysis had elevated IOP at presentation, of which 54.2% presented with acute angle closure. Other mechanisms of elevated IOP in cases of traumatic lens dislocation include inflammation associated with the dislocated lens, phacolytic glaucoma, and obstruction of the trabecular meshwork by the vitreous prolapse into the anterior chamber[8]. More information about traumatic glaucoma can be found in this article: https://eyewiki.aao.org/Traumatic_Glaucoma.
Malignant glaucoma has also been reported by a traumatic subluxation into the anterior chamber[9].
Corneal decompensation
Anterior lens subluxation may also lead to corneal decompensation as a result of lens-endothelial touch. Corneal decompensation typically presents with corneal edema and decreased visual acuity on exam. There have been cases with incomplete recovery from corneal decompensation from endothelial touch from lens subluxation that may require descement’s stripping endothelial keratoplasty (DSAEK)[10] [11]. In addition, even with lens removal, retained lens fragments may also lead to corneal decompensation and should be on the differential with one case presenting 15 years after cataract removal[12].
Uveitis
The lens may be a source of inflammation after trauma due to leakage of proteins or capsule breakage. Lens-induced uveitis (LIU), previously referred to as phacoanaphylactic endophthalmitis, usually occurs within 14 days of trauma but reports found it may occur as late as 59 years[13]. Typically unilateral, symptoms include photophobia, ocular pain, and decreased visual acuity. Diagnosis of LIU is clinical although challenging with one study diagnosing six cases of LIU clinically out of 140. In the setting of lens subluxation, LIU is not conservatively managed and is an indication for lens removal[14].
In addition, traumatic anterior uveitis may occur concomitantly, although independent, with lens subluxation as it is unrelated to an immune response to the lens and additional info can be found in this article: https://eyewiki.aao.org/Traumatic_Iritis
Associated ocular trauma
There may be other concomitant globe trauma in patients with lens dislocation, including open globe injury, iridodialysis, hyphema, vitreous hemorrhage, traumatic optic neuropathy, and retinal breaks or detachment. In one study, traumatic lens subluxation and luxation was associated with retinal breaks or detachment in 37.7% of patients requiring vitrectomy, with only 8.9% identified prior to surgery[15], highlighting the importance of a careful exam in the case of traumatic lens dislocation.
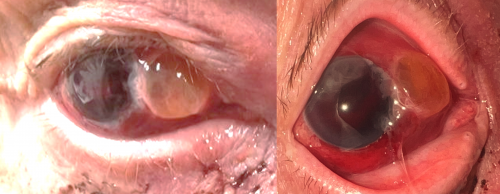
With blunt trauma, there can be indirect rupture of the sclera in blunt trauma, leading to traumatic dislocation of a crystalline lens into the subconjunctival or subtenon’s space. This is a rare finding known as a phacoceole, usually found in older patients in the context of a hard lens and rigid sclera[16].
Management
Anterior dislocation requires urgent lens removal, especially in cases of rising intraocular pressure where lens-induced acute angle closure glaucoma occurs due to pupillary block.[17] Other indications include persistent uveitis and lens-corneal decompensation. Temporizing measures to reduce intraocular pressure such as acetazolamide or peripheral iridotomy can be used prior to lens removal. Zonular status needs to be well established to determine optimal intraocular lens placement.
Posterior dislocation in some cases may be well-tolerated and managed conservatively with an aphakic contact lens. In one case, a 16 year old with good corrected visual acuity and no other significant medical history had been in a motor vehicle accident at the age of 1 with head trauma was found to have bilateral posterior lens subluxation and continued to be treated conservatively. There are some that believe lens removal is warranted to prevent the development of these complications altogether. If the patient is still symptomatic or develops complications such as persistent uveitis or glaucoma, lens removal is indicated.[18]
Methods of removal of a dislocated crystalline lens include phacoemulsification with aid of a capsular tension device, intracapsular cataract extraction, and pars plana lensectomy. The approach is typically dictated by severity of lens subluxation due to zonular disruption. With minimal lens instability, an anterior approach with phacoemulsification with a capsular tension device may be used. If unsafe, extracapsular or intracapsular extraction is also another method of anterior approach. In severe cases of lens subluxation and greater than 180 degrees of zonular disruption or complete dislocation, a posterior approach with simultaneous pars plana lensectomy and vitrectomy is used.
Intraocular lens type, technique, and location is determined on a case-by-case basis with anterior and posterior placement each having their own advantages and disadvantages. These decisions should take into account the severity of zonular dialysis and integrity of the capsular bag.
- ↑ Jarrett WH. Dislocation of the Lens: A Study of 166 Hospitalized Cases. Arch Ophthalmol. 1967;78(3):289–296. doi:10.1001/archopht.1967.0098003029100
- ↑ 2.0 2.1 Shuen JA, Malone M, Burke Z, Baquero A. Traumatic Anterior Dislocation of the Lens. J Emerg Med. 2018;55(4):565-566. doi:10.1016/j.jemermed.2018.07.001
- ↑ Bord SP, Linden J. Trauma to the globe and orbit. Emerg Med Clin North Am. 2008 Feb;26(1):97-123, vi-vii. doi: 10.1016/j.emc.2007.11.006. PMID: 18249259.
- ↑ Netland KE, Martinez J, LaCour OJ 3rd, Netland PA. Traumatic anterior lens dislocation: a case report. J Emerg Med. 1999;17(4):637-639. doi:10.1016/s0736-4679(99)00052-9
- ↑ Vyas S, Krishna S, Kumar A, Khandelwal N. 'Floating lens sign' in traumatic lens dislocations. Middle East Afr J Ophthalmol. 2015 Jan-Mar;22(1):129-30. doi: 10.4103/0974-9233.148365. PMID: 25624690; PMCID: PMC4302470.
- ↑ McWhae JA, Crichton AC, Rinke M. Ultrasound biomicroscopy for the assessment of zonules after ocular trauma. Ophthalmology. 2003 Jul;110(7):1340-3. doi: 10.1016/S0161-6420(03)00464-0. PMID: 12867388.
- ↑ Chee SP, Jap A. Management of traumatic severely subluxated cataracts. Am J Ophthalmol. 2011 May;151(5):866-871.e1. doi: 10.1016/j.ajo.2010.10.035. Epub 2011 Feb 18. PMID: 21310378.
- ↑ Inatani M, Tanihara H, Honjo M, Kido N, Honda Y. Secondary glaucoma associated with crystalline lens subluxation. J Cataract Refract Surg. 2000 Oct;26(10):1533-6. doi: 10.1016/s0886-3350(00)00471-5. PMID: 11033403.
- ↑ Sarrafpour S, Davies I, Ahmed O, Liu J, Teng CC. Cataract Surgery in Malignant Glaucoma from Complete Subluxation of Lens into Anterior Chamber. J Curr Glaucoma Pract. 2021 Sep-Dec;15(3):164-167. doi: 10.5005/jp-journals-10078-1320. PMID: 35173401; PMCID: PMC8807931.
- ↑ Wu S, Yu X, Dai Q, Fu Y, Lin X. Corneal decompensation due to spontaneous absorption of lens and anterior dislocation of lens capsule: A case report. Medicine (Baltimore). 2019 Dec;98(50):e18417.
- ↑ Moshirfar M, Stagg BC, Muthappan V, Vasavada SA. Traumatic dislocation of implanted collamer phakic lens: a case report and review of the literature. Open Ophthalmol J. 2014 May 30;8:24-6. doi: 10.2174/1874364101408010024. PMID: 24959305; PMCID: PMC4066362.
- ↑ Kang HM, Park JW, Chung EJ. A retained lens fragment induced anterior uveitis and corneal edema 15 years after cataract surgery. Korean J Ophthalmol. 2011 Feb;25(1):60-2. doi: 10.3341/kjo.2011.25.1.60. Epub 2011 Jan 17. PMID: 21350698; PMCID: PMC3039198.
- ↑ Nche EN, Amer R. Lens-induced uveitis: an update. Graefes Arch Clin Exp Ophthalmol. 2020 Jul;258(7):1359-1365. doi: 10.1007/s00417-019-04598-3. Epub 2020 Jan 6. PMID: 31907641; PMCID: PMC7223998.
- ↑ Thach AB, Marak GE Jr, McLean IW, Green WR. Phacoanaphylactic endophthalmitis: a clinicopathologic review. Int Ophthalmol. 1991 Jul;15(4):271-9. doi: 10.1007/BF00171031. PMID: 1917323.
- ↑ Ke G, Zhou E, Zhu K, Wei Y, Wang Z, Jia Y, Wang S, Gu Y. Retinal break associated with traumatic lens dislocation or subluxation requiring vitrectomy. Graefes Arch Clin Exp Ophthalmol. 2020 Mar;258(3):693-697. doi: 10.1007/s00417-019-04530-9. Epub 2019 Nov 28. PMID: 31781882.
- ↑ Yurdakul NS, Uğurlu S, Yilmaz A, Maden A. Traumatic subconjunctival crystalline lens dislocation. J Cataract Refract Surg. 2003 Dec;29(12):2407-10. doi: 10.1016/s0886-3350(03)00332-8. PMID: 14709305.
- ↑ Stürmer, J. (2018). Lens-Induced Angle-Closure Glaucoma. In: Schmidt-Erfurth, U., Kohnen, T. (eds) Encyclopedia of Ophthalmology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-540-69000-9_316
- ↑ Salehi-Had, Hani MD; Turalba, Angela MD Management of Traumatic Crystalline Lens Subluxation and Dislocation, International Ophthalmology Clinics: Winter 2010 - Volume 50 - Issue 1 - p 167-179 doi: 10.1097/IIO.0b013e3181c567de


