Optic Disk Melanocytoma and Optical Coherence Tomography Angiography OCT-A
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Optic disk melanocytoma is a benign neoplasm, which seldom exhibits malignant transformation; nevertheless it can show growth and several complications. It is necessary to differentiate it from other neoplasms such as choroidal melanoma and choroidal nevus. Swept-source optical coherence tomography angiography (OCT-A) is a relatively new device that penetrates more deeply into the retinal layers and can be used to assess these lesions as well as identify their imaging features.
Disease
Melanocytoma is a rare benign pigmented neoplasm that may occur anywhere in the uvea. It often affects the optic nerve head, but may even involve the adjacent retina and choroid in some cases. It is believed to be a congenital and non-hereditary lesion.[1][2][3]
History
Historically, melanocytoma was considered a malignant neoplasm by ophthalmologists and pathologists. As a result, some enucleations were performed because of this erroneous belief . Reese in 1933 used the term "melanoma of optic disk" to describe pigmented lesions of the optic nerve head with clinical and histopathological features similar to melanocytoma.[4] Eventually Zimmerman and Garron revealed its benign nature in 1962 after performing a clinicopathological correlation on enucleated eyes with suspected melanoma. The term melanocytoma was first used by them since the tumor cells appeared to be similar to those in ocular melanocytosis. [5]
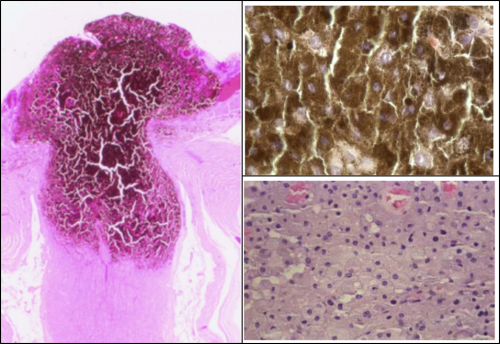
Histopathological features
Melanocytoma are histopathologically composed of highly pigmented round cells with cytoplasmic melanosomes and a deficit of lipofuscin deposits. It may affect anywhere in the uvea but often partially involves the optic nerve head. It may even involve the adjacent retina and choroid in some cases. Cells are of low nuclear-to-cytoplasmic ratio, and immunohistochemical staining is positive for melan A and negative for S100. Initially presumed to be an avascular tumor, OCT-A technology has shown there to be intrinsic microvascular characteristics in melanocytomas.[2][6][7][8]
Pathophysiology
Melanocytoma has a benign course and is derived from uveal melanocytes, such as uveal nevi and malignant melanoma. The pathogenesis of optic disk melanocytoma is unknown, but it is generally assumed to be a congenital lesion. Because of the association of melanin pigment with age, young children may initially have amelanotic lesions which become clinically visible in adulthood. [1][4][9][3]
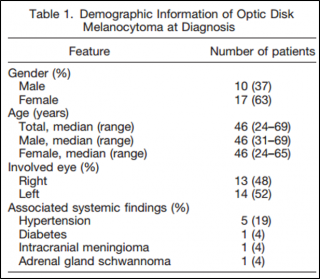
Demographics
Age
The mean age at diagnosis is 50 years, with a range of 1 year to 91 years (similar to the age at diagnosis of uveal melanoma). Amelanotic lesions not clinically evident at birth have been detected that later become pigmented over time.[4][2]
Race and gender
It has no race predilection. Nevertheless, the demographic features found in some studies suggest a preponderance for caucasians (65%). [1] Otherwise, uveal melanoma is infrequent in Asians and African Americans. It seems to be slightly more frequent in women (63% of cases).[4]
Diagnosis
Signs and Symptoms
Visual acuity
Commonly unilateral, asymptomatic and stable. It usually does not cause compromise of visual acuity. However, visual symptoms may be present in 26% of cases and these are associated with exudation with foveal involvement or tumor necrosis.[1][2][6][10] In other cases, decreased vision may be related to central retinal vein obstruction or, more rarely, malignant transformation. [10] Other symptoms can be present, such as flashes of light (4%), floaters (4%) or none (76%).[1] In certain cases of extensive visual loss due to melanocytomas, vision improved over time suggestive of possible transient ischemic change or inflammation.[3]
Pupillary changes
An afferent pupillary defect may be found even in the presence of good visual acuity. It is probably related to compression of the optic disk fibers by the melanocytoma cells.[4][11]
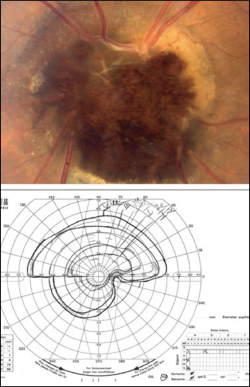
Visual field
The visual field is normal in 10% and abnormal in 90% of patients. Field deficits include temporal islands of vision; enlargement of blind spot related to the amount of tumor extension; arcuate defects associated with compression of axons; and other patterns such as a nasal step (10%), relative nerve fiber bundle defect (20%), or an absolute arcuate defect (20%). One OCT-A study found that absence of the blood vessel network within certain areas of the melanocytoma corresponded with the location of the visual field defect.[12] In fact, the area of the blood vessel network absence was more significantly associated with the visual field deficit than the area of the tumor.
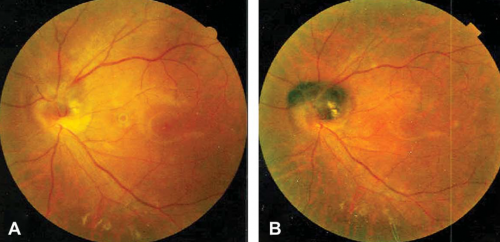
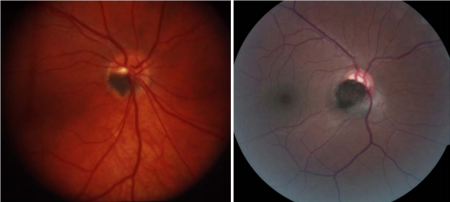
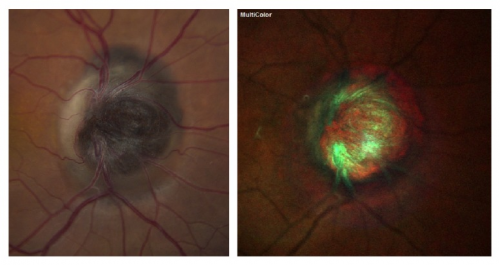
Clinical features
It is usually unilateral, but in children may be bilateral. Clinically, the optic disk melanocytoma appears as a pigmented homogeneous mass with total absence of autofluorescence.[2][6]
However, an amelanotic lesion that becomes pigmented over time has been described.[13]
It can be confined to the disk in 15% of cases. Approximately 50% of melanocytomas involve one quadrant of the optic disk with the inferotemporal quadrant being the most common site (33%) and the nasal side being the least common (12%). Melanocytoma can extend over the margin of the optic nerve head to involve the adjacent choroid in 54% of patients or the adjacent retina in 30%. Commonly remains stable with only rare instances of malignant transformation. In some cases, it can progressively grow, which may lead to vitreous seeding and neovascularization.[2][6][10]
Systemic associations
It usually is an isolated condition, but some studies suggest an association with neurofibromatosis type 2, basal cell carcinoma, and vitiligo which may be coincidental. In other cases, it has been associated with hypertension (8%) and tumors of neural crest origin, such as intracranial meningioma and adrenal gland schwannoma. [1][4]
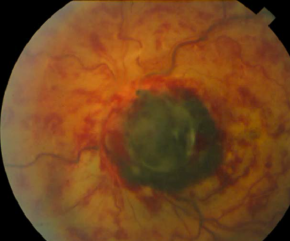
Clinical course
Melanocytomas are generally stable, but 10-15% of them show enlargement over several years. The main predictive risk factor for growth is an initial thickness greater than 1.5 mm. Larger lesions may develop tumor necrosis, ischemic optic neuropathy, or retinal vein obstruction. Malignant transformation is estimated to occur in about 1-2% of patients. Features of malignant transformation include extensive involvement of the optic disk with severe visual loss.
Local complications
Optic disk melanocytoma can show ischemic necrosis, disk edema (25%), intraretinal edema (16%), subretinal fluid (14%), yellow intraretinal exudation (12%), focal hemorrhage (5%), vitreous seeds (4%), and retinal vein obstruction (3%).[4]
Clinical diagnosis
Patients typically have no relevant past or familiar history and may be noted on a routine eye exam to have a pigmented mass on the optic nerve head. The visual acuity usually is normal. Slit-lamp examination of the anterior segment is normal and ocular melanocytosis usually is not observed. Fundus examination shows a pigmented dark brown lesion entirely covering or partially obscuring the optic nerve head and may extend over the margin with adjacent retinal or choroidal involvement in some cases. Swelling of the optic disk margin may be observed. Associated evidence of exudation, vitreous seeds or hemorrhage may sometimes be found as well.
Imaging diagnosis
Melanocytoma usually is diagnosed based on ophthalmoscopic features. Imaging may be helpful to confirm its benign nature and distinguish it from other lesions and neoplasms. Several imaging modalities have been used for optic disk melanocytoma diagnosis and follow-up.
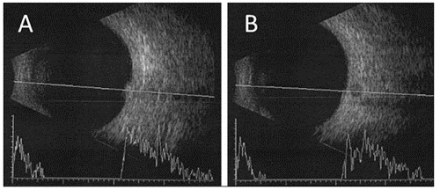
Ultrasonography
Ultrasound has been largely used for assessment of tumors that involve the optic disk and choroid. A dome-shaped appearance is a frequent feature in melanocytoma, and its high internal reflectivity indicates a benign lesion. Conversely, low internal reflectivity may be indicative of a high-risk for growth and malignant transformation.[4] Although ultrasonography is a useful guide to determining malignancy, it does not detect neovascularization, tumor extension into the retrolaminar portion and other findings such as intraretinal edema. Use of this imaging modality should be complemented with other diagnostic aids.
Fundus Autofluorescence
Fundus autofluorescence, including shortwave autofluorescence (SWAF: excitation at 488nm and emission >510nm) and infrared autofluorescence (IRAF: excitation at 785nm and emission 805-840nm), noninvasive imaging modalities have been used to visualize the melanocytic lesion. Studies have demonstrated the utility of fundus autofluorescence in distinguishing an optic disc melanocytoma from a nevus or melanoma. Melanocytomas may show sharply demarcated hypoautofluorescence on SWAF, and show well-defined hyperautofluorescence on IRAF.[3]
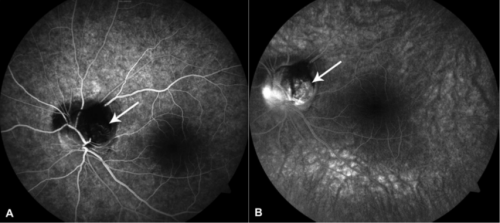
Fluorescein and Indocyanine Green Angiography
Other studies, such as fluorescein and indocyanine green angiography, show a diffuse hypofluorescent lesion and hyperfluorescent areas related to subretinal fluid and disk edema. [1][2][6][13][4]However, these studies are more invasive due to the need to inject intravenous dye and often provide less additional information than other imaging techniques.
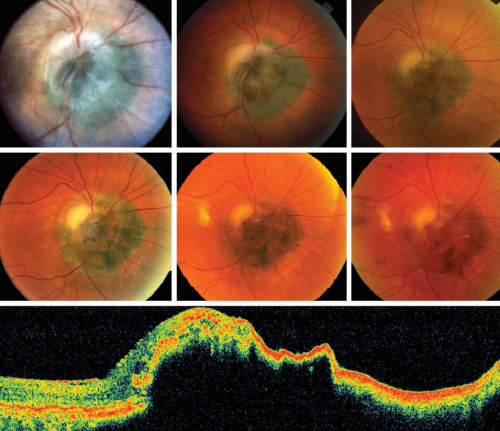
Optical coherence Tomography (OCT)
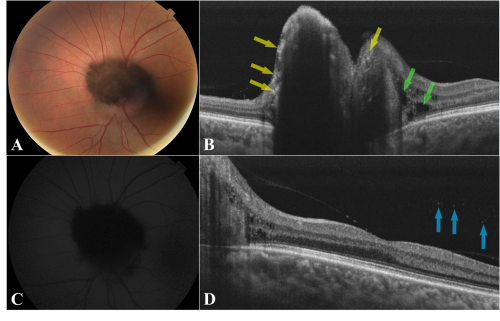
OCT captures high resolution cross sectional images through the lesion and adjacent structures. The identification of a nodular elevation with dense posterior shadowing, areas of irregular hyperreflectivity overlaying the tumor, and even thin hyperreflective lines delineating the vessels and anterior side of the tumor using spectral-domain OCT has been largely documented in the literature. It has also been observed that thicker tumors typically had thinner anterior hyper-reflective borders and denser shadowing.[1][2][6][4][3] Currently, there are few reports of melanocytoma features based on swept-source OCT. B-scan OCT images have identified multiple irregular hyperreflective dots on the anterior surface overlying the tumor, with or without perivascular distribution. These hyperreflective dots may correspond to melanin-phagocytizing activity of macrophages.[2] [6] This phagocytizing activity may induce the formation of subretinal and intraretinal fluid in adjacent retinal tissue.
Other findings are related to local complications. Some authors have theorized that choroidal involvement could be assumed based on upward displacement of retinal pigment epithelium, significant retinal nerve fiber layer loss or choroidal hyperreflectivity[14] [15][15]. However, the choroidal vasculature cannot be visualized directly due to dense posterior shadowing from the melanocytoma which limits identification of underlying structures.
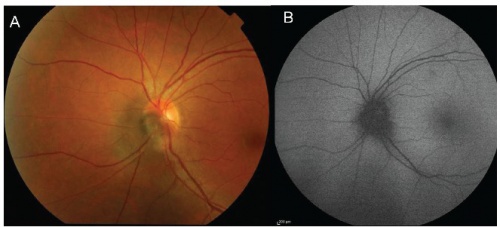
Swept-source optical coherence tomography angiography (OCT-A)
OCT–A has increasingly become a useful noninvasive technique for the assessment of different ophthalmic diseases. Currently, few reports exist regarding optic disk melanocytoma features using swept-source OCT- A. This new technology may become a good alternative for following these lesions, perhaps improving the tumor extension detection, identification of progression and finally differentiating it from other neoplasms, including choroidal malignant melanoma.
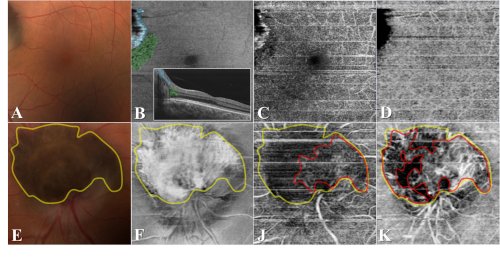
OCT-A allows the visualization of vasculature using the motion contrast principle, providing a high definition image of different layers including the choroid.[16] It has the capacity to visualize capillaries on the tumor surface which do not appear on other imaging modalities like fluorescein angiography or indocyanine green angiography. Quantification of the microvascular flow rate, which has been demonstrated to be different in melanocytoma versus melanoma, offers further novel diagnostic utility.[7] OCT-A may represent an important advantage by helping to determine the tumor's depth despite the posterior dense shadowing observed on OCT B- scan.
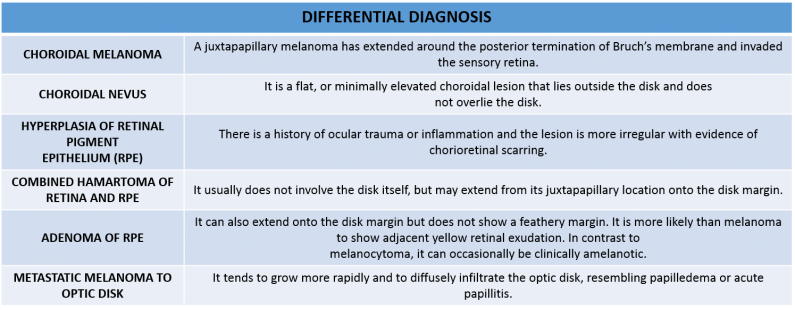
Differential diagnosis
Melanocytoma usually is diagnosed using ophthalmoscopic features. Nevertheless, the imaging is necessary to confirm its benign nature and distinguish it from other lesions and neoplasms such as malignant melanoma, choroidal nevus, optic nerve glioma, capillary hemangioma or metastases.[1]
Management
This lesion does not require any type of treatment. Clinical and imaging follow-up should be performed annually.
Medical follow up
Optic disk melanocytoma requires a clinical and imaging assessment to characterize the principal features and distinguish it from other pathologies. Different studies such as color fundus photography and OCT annually should be considered. OCT-A is a non invansive alternative to assess the tumor's depth and presence of intraretinal edema, choroidal involvement and vitreous seeds without a contrast medium.
Complications
Melanocytoma can progressively enlarge and may lead to vitreous seeding and neovascularization in some cases. [1][4]
Prognosis
Optic disk melanocytoma is a benign neoplasm, which seldom exhibits malignant transformation. Nevertheless, it can show growth and several complications. 10% - 15% of them show subtle enlargement over several years.[1]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Shields JA, Demirci H, Mashayekhi A, Shields C. Melanocytoma of optic disc in 115 cases: the 2004 Samuel Johnson Memorial Lecture, part 1. Ophthalmology. 2004;111:1739-46
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Lee E, Sanjay S. Optic Disc Melanocytoma Report of 5 Patients From Singapore With a Review of the Literature. Asia Pac J Ophthalmol (Phila) 2015;4:273-8
- ↑ 3.0 3.1 3.2 3.3 3.4 Furuta M. (2019) Optic Disc Melanocytoma. In: Rojanaporn D. (eds) Ocular Oncology. Retina Atlas. Springer, Singapore. https://doi-org.proxy.libraries.rutgers.edu/10.1007/978-981-13-2336-2_14
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 Shields JA, Demirci H, Mashayekhi A, et al. Melanocytoma of the optic disc: a review. Surv Ophthalmol. 2006;51:93–104.
- ↑ Zimmerman LE, Garron LK. Melanocytoma of the optic disc. Int Ophthalmol Clin.1962;2:431-40.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 Zhang P, Hui YN, Xu WQ, et al. Infrared autofluorescence, short-wave autofluorescence and spectral-domain optical coherence tomography of optic disk melanocytomas. Int J Ophthalmol, 2016;9:713-6.
- ↑ 7.0 7.1 Raval V, Reddy R, Kaliki S, Das T, Singh A. Optic nerve head melanocytoma: Optical coherence tomography/angiography features. Indian journal of ophthalmology. 2021;69(2):332-336. doi:10.4103/ijo.IJO_710_20
- ↑ Goto H, Yamakawa N, Komatsu H. Histopathology and immunohistochemistry of choroidal melanocytoma demonstrated by local resection: A case report. American journal of ophthalmology case reports. 2021;23:101147-.doi:10.1016/j.ajoc.2021.101147
- ↑ Eldaly H, Eldaly Z. Melanocytoma of the Optic Nerve Head, Thirty-Month Follow-Up. Semin Ophthalmol. 2015;30:464-9.
- ↑ 10.0 10.1 10.2 Lee CS, Bae JH, Jeon IH, et al. Melanocytoma of the optic disk in the Korean population. Retina. 2010;30:1714-20.
- ↑ Al-Rashaed S, Abboud EB, Nowilaty SR. Characteristics of optic disc melanocytomas presenting with visual dysfunction. Middle East Afr J Ophthalmol. 2010;17:242-5.
- ↑ Kwak JJ, Lee DH, Lee SC, Lee CS. Evaluation of blood vessel network formation and visual field defect in optic disc melanocytoma. Br J Ophthalmol. 2021 Sep 27:bjophthalmol-2021-319630. doi: 10.1136/bjophthalmol-2021-319630. Epub ahead of print. PMID: 34580073.
- ↑ 13.0 13.1 Mohmad Z, Kah TA, Yong KC, et al. Melanocytoma of the optic nerve head - a diagnostic dilemma. Clin Pract. 2011;1:e60.
- ↑ Saxena S, Sharma B, Bhasker SK. Three-dimensional spectral-domain optical coherence tomography of melanocytoma of the optic nerve head. J Ocul Biol Dis Infor.2010;3:112-6.
- ↑ 15.0 15.1 Okubo A, Unoki K, Yoshikawa H, et al. Hyperreflective dots surrounding the central retinal artery and vein in optic disc melanocytoma revealed by spectral domain optical coherence tomography. Jpn J Ophthalmol. 2013;57:108-12.
- ↑ Koustenis A Jr, Harris A, Gross J, et al. Optical coherence tomography angiography: an overview of the technology and an assessment of applications for clinical research. Br J Ophthalmol 2017;101:16-20.