All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Nutritional optic neuropathy is an uncommon and unrecognized cause of bilateral, symmetrical and progressive visual loss; which is part of the group of metabolic neuropathies. [1] [2] These optic neuropathies are often triggered by vitamin B complex déficits: vitamin B12 (cobalamin), vitamin B1 (thiamin), vitamin B2 (riboflavin) and vitamin B9 (folic acid); elements that are crucial for the processes of mitochondrial oxidative phosphorylation. The lack of these, causes an interruption of electron transport and, consequently, a reduction in ATP production, in addition to accumulation of free radicals. [1][3]
Epidemiology - History
Nutritional optic neuropathy, although rare, has been documented throughout history, specifically during periods of war and famine, where it is believed to be most prevalent. However, nowadays, there is a group of emerging patients who are at risk of developing this pathology, especially patients who have undergone bariatric surgery, are into restrictive or vegan diets. [1] [4]
Some known cases are: Strachan syndrome related to nutritional deficit in Jamaican sugarcane workers in the 1880s, tropical amblyopia in Nigerians, optic neuropathy in Japanese prisoners during WWII, Cuban epidemic optic neuropathy and Tanzanian epidemic optic neuropathy. [2][5]
Etiology
Vitamins of B complex are water-soluble vitamins that are present in some foods, added to a few food products, and available as dietary supplements. Isolated deficiency of a complex B vitamin is uncommon, it usually coexists with poor diet, alcoholism and malabsorptive disorders. They play a critical role as coenzymes for various enzymatic reactions. Vitamins B12, B6 and B1, called neurotrophic vitamins, are essential to maintain the health of the nervous system, including the optic nerve. [1] [2]
- Vitamin B9: Folate is stored in the liver and doesn’t need to be ingested daily. The main function of folate is to contribute to proper cell division, it works as a coenzyme involved in the synthesis of pyrimidines and purines. In adults, reduced folate levels are related to cognitive dysfunction in elderly patients, visual system compromise in the context of nutritional amblyopia, as well as, optic atrophy and gradual decrease in vision. There is an important association between the lack of serum folate and the development of nutritional optic neuropathy. [1] [6]
- Vitamin B12: Also known as cobalamin, it is involved in metabolism. Human cells cannot synthesize Vitamin B12, however, a typical balanced diet contains an adequate amount of cobalamin. Proper red blood cell formation in the bone marrow, synthesis of myelin in the nervous system and DNA synthesis are some of the most important roles of Vitamin B12 in the human body. [1] [6] [7]
- Vitamin B1: Thiamin is involved in energy metabolism, in the growth, development, and function of cells. People require a continuous supply of Vitamin B1 in their diet because it has a short half-life and is stored in minimal amounts in the liver. [1] [6]
- Vitamin B6: Pyridoxine participates in the biosynthesis of neurotransmitters and in maintaining normal levels of homocysteine, it is also involved in gluconeogenesis, glycogenolysis, immune function, and hemoglobin formation. [6]
- Copper: Copper participates in critical cellular processes, such as oxidative phosphorylation and cellular metabolism. Its deficiency leads to dysfunctional enzymes, particularly various oxidoreductases and monooxygenases because it works as an enzyme cofactor. [8] [9]These copper-dependent enzymes are involved in cellular metabolism processes, such as neurotransmitter conversion, electron transport in oxidative phosphorylation, free radical scavenging, and oxidation of iron for transport. Copper deficiency is a major cause of neuropathy in 10% to 20% of patients after bariatric surgery. [8] [9]
Risk Factors
- Strict vegan or vegetarian diets without supplementation: Strict vegan patients, especially without vitamin supplementation, are at risk of deficiency of vitamin A, and the complex complex B vitamins, particularly: B12, B1, B9. Causing secondary neurological alterations. [2] [10] [11]
- Bariatric surgery: Restrictive procedures that produce malabsorption such as: gastric bypass Roux-en-Y and biliopancreatic diversion with duodenal switch. Vitamin B12, B1 and copper deficiencies are related to optic neuropathy developement 1.5 - 3 years after surgery. Nyctalopia related to vitamin A deficiency has been described. [8] [12] [13] [14]
- Inflammatory bowel diseases: Malabsorptive syndromes, such as celiac disease cause a deficiency especially of vitamin B12 and folates. [12] [15]
- Pernicious anemia: It is characterized by poor absorption of vitamin B12 due to a deficiency of intrinsic factor. It is usually associated with other autoimmune entities such as Sjögren's syndrome, Hashimoto's thyroiditis or celiac disease. Symptoms generated by vitamin B12 deficiency can manifest without anemia and with the presence of neuropsychiatric symptoms. The cause of neurological symptoms is thought to be secondary to the role that vitamin B12 plays in neuronal myelination, which could lead to a reduction in the nerve impulse in the optic nerve. [16]
- Parenteral nutrition without adequate vitamin supplementation: Elemental nutrients are administered intravenously (lipids, amino acids, glucose, vitamins and minerals), as a complementary and non-competitive route to the enteral route. There have been some reports of acute thiamine deficiency as a complication of parenteral nutrition without vitamin supplementation, which could lead to neurological symptoms and signs in this type of patients. [17]
- Malnutrition: Factors that influence malnutrition include living in a developing country, suffering from psychiatric disorders, and having a vegan diet. Optic neuropathy develops from having chronic malnutrition that causes deficiency of several vitamins, including vitamins B1, B9, B12 and copper. [1] [3]
- Alcoholism: Chronic alcoholism is not a direct cause of optic neuropathy, however it is associated with a high incidence of nutritional deficiencies, such as deficiency of vitamin B12 and B9. [4]
Pathophysiology
The exact mechanism by which the nutritional deficit causes optic neuropathy is uncertain, however these vitamins all of these vitamins are involved in the production of ATP, and are crucial for the processes of mitochondrial oxidative phosphorylation. Therefore, their deficit would generate mitochondrial dysfunction, interrupting the transfer of electrons, which would lead to a decrease in ATP, in addition to oxidative stress, due to the accumulation of free radicals, especially the generation of superoxide anion. [2] [7] [17]
Some studies have described intracellular superoxide formation within retinal ganglion cells as a common pathological pathway for cell death. [2] [18]
Diagnosis
Clinical diagnosis
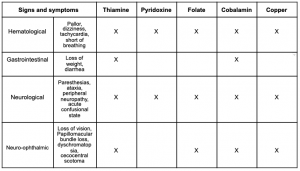
See table 1.
Symptoms
Symptoms of nutritional optic neuropathy are subacute and progressive, and include bilateral, symmetrical visual impairment; painless visual loss, centrocecal scotoma that can be unilateral or bilateral, dyschromatopsia and loss of contrast sensitivity. [1] [3] [19]
Signs
At early stages include normal or hyperaemic optic disc, except in thiamine deficiency where the optic disc is swollen at early stages; temporal optic disc pallor, thinning of the retinal nerve fiber layer thickness (RNFL) in the papillomacular bundle, normal or near normal latency with significantly reduced amplitude of VEP, at late stages diffuse optic disc pallor and thinning of RNFL in all the quadrants is found. There is no relative afferent pupillary defect because nutritional optic neuropathy has a symmetrical presentation. [1] [3] [7] [19]
Physical examination
Physical exam :
- Snellen visual acuity
- Confrontational visual field exam.
- Ishihara test → Dyschromatopsia.
- Amsler grid.
- Direct ophthalmoscopy of the optic nerve and retina.
- Swinging flashlight test.
Diagnostic
Complementary exams:
- Visual Field → Central o cecocentral scotoma.
- Visual Evoked Potentials → Reduced amplitude, normal or near normal latency.
- Retinal nerve fibre layer Optical coherence tomography (OCT) → RNFL thinning.
- Electroretinography → To exclude retinal disease.
- MRI → To exclude compressive or demyelinating diseases.
Laboratory test
Complete cell blood count, peripheral blood smear, and a complete metabolic profile should be performed. Folic acid, vitamin B12, total and indirect bilirubins levels might be diminished; when the values of folic acid or vitamin B12 are low or at the limit, levels of homocysteine and methylmalonic acid (MMA) should be requested. Homocysteine values will be elevated both in vitamin B12 and folic acid deficit, while the levels of MMA will be increased in vitamin B12 deficiency and within normal limits in folic acid deficiency. There are certain conditions that could generate false positives high levels of MMA such as, kidney failure, intestinal bacterial growth, or methylmalonic aciduria. Increased homocysteine could be found in patients with hereditary hyperhomocysteinemia. [20]
Primary prevention
Vitamin supplement therapy is necessary depending on the cause of the deficit. Folic acid treatment is usually administered in patients with increased requirements such as pregnant women and in patients with chronic hemolytic anemia.Long-term and lifelong replacement should be offered to all patients undergoing bariatric surgery or in patients with intestinal malabsorption. Patients who underwent gastric band surgery should receive multivitamin and mineral supplements, such as, folic acid, iron, calcium, thiamine, and vitamin D. In other bariatric surgery procedures, it is recommended to include vitamin B12 and minerals, monitoring serum levels of vitamin B12 in all patients. [13]
Management
Treatment : The mainstay of treatment is treating the cause in this case nutritional or vitamin deficiency.
Vitamin B12 is available orally, intranasally, sublingually, subcutaneously, or intramuscularly (IM). In the case of vitamin B12 and folic acid deficiency, the duration of therapy will depend on the cause of the deficiency. Vitamin supplement must be for life in irreversible causes, such as gastric bypass and pernicious anemia. While short-term treatment would be indicated in reversible conditions of malabsorption, for example, inadequate intake due to poor diet, alcoholism or drug-induced. Oral administration is generally effective in patients with a reversible cause and is administered at a dosage of 1000 μg daily for at least 1 month followed by either continuation of the same dose for maintenance, or the dose can be decreased to 100 to 500 μg daily in patients with mild reversible deficiencies. The parenteral formulation is preferably administered IM at a dose of 1000 μg daily for 1 week followed by 1000 μg once a week for 1 month. The maintenance dose for IM or parenteral deep SC injection is 1000 μg monthly and indefinitely, depending on the etiology. Treatment in folic acid deficiency varies between 1 and 5 mg / day. Treatment can last 3-6 months until the cause of the deficiency is corrected. [20] [21]
Prognosis
Visual prognosis depends on the time and severity of the nutritional deficit to which the patient was exposed. The first thing that improves is visual acuity and then color vision, contrary to symptom instauration that is characterized by initial dyschromatopsia followed by visual acuity loss. The Cuban epidemic optic neuropathy (1991-1993) was one of the best and most studied pathologies regarding the impact of nutritional deficit as the origin of optic neuropathy. Many patients experienced vast improvement in their symptoms after therapy, some did not fully regain their vision. [22]
The degree of visual recovery was related to the speed with which treatment was started after diagnosis; the prognosis for recovery was poor if treatment had not been started within 3 months of diagnosis. Recovery of normal vision was rare in patients with severe visual loss (visual acuity of 20/400 or worse). A 2002 study showed that around 10% of affected patients had some residual degree of impairment, visual loss being more common than other neurological symptoms. [23]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Roda, M., di Geronimo, N., Pellegrini, M. and Schiavi, C., 2020. Nutritional Optic Neuropathies: State of the Art and Emerging Evidences. Nutrients, 12(9), p.2653.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Jefferis, J. and Hickman, S., 2019. Treatment and Outcomes in Nutritional Optic Neuropathy. Current Treatment Options in Neurology, 21(1).
- ↑ 3.0 3.1 3.2 3.3 Sadun, A., 2002. Metabolic optic neuropathies. Seminars in Ophthalmology, 17(1), pp.29-32.
- ↑ 4.0 4.1 Margolin, E., & Shemesh, A. (2021). Toxic and Nutritional Optic Neuropathy. Retrieved 29 May 2021, from https://www.ncbi.nlm.nih.gov/books/NBK499979/?report=printable
- ↑ Byrne, E., Horowitz, M., & Dunn, D. (1980). STRACHAN'S SYNDROME 30 YEARS AFTER ONSET. Medical Journal Of Australia, 1(11), 547-548. doi: 10.5694/j.1326-5377.1980.tb135106.
- ↑ 6.0 6.1 6.2 6.3 Ods.od.nih.gov. 2021. Office of Dietary Supplements - Vitamin B12. [online] Available at: <https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional/
- ↑ 7.0 7.1 7.2 Shipton, M., & Thachil, J. (2015). Vitamin B12 deficiency – A 21st century perspective. Clinical Medicine, 15(2), 145-150. doi: 10.7861/clinmedicine.15-2-145
- ↑ 8.0 8.1 8.2 Shah, A., & Tamhankar, M. (2014). OPTIC NEUROPATHY ASSOCIATED WITH COPPER DEFICIENCY AFTER GASTRIC BYPASS SURGERY. RETINAL Cases & Brief Reports, 8(1), 73-76. doi: 10.1097/icb.0000000000000008
- ↑ 9.0 9.1 Winston, G., & Jaiser, S. (2008). Copper deficiency myelopathy and subacute combined degeneration of the cord – Why is the phenotype so similar?. Medical Hypotheses, 71(2), 229-236. doi: 10.1016/j.mehy.2008.03.027
- ↑ Milea, D., Cassoux, N., & LeHoang, P. (2000). Blindness in a Strict Vegan. New England Journal Of Medicine, 342(12), 897-898. doi: 10.1056/nejm200003233421217
- ↑ Nightingale, L., & Paviour, D. (2009). Nutritional optic and peripheral neuropathy: a case report. Cases Journal, 2(1), 7762. doi: 10.4076/1757-1626-2-7762
- ↑ 12.0 12.1 Rapoport, Y., & Lavin, P. (2016). Nutritional Optic Neuropathy Caused by Copper Deficiency After Bariatric Surgery. Journal Of Neuro-Ophthalmology, 36(2), 178-181. doi: 10.1097/wno.0000000000000333
- ↑ 13.0 13.1 Mechanick, J., Apovian, C., Brethauer, S., & Garvey, W. (2020). Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures – 2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Surgery For Obesity And Related Diseases, 16(2), 175-247. doi: 10.1016/j.soard.2019.10.025
- ↑ Moss, H. (2016). Bariatric Surgery and the Neuro-Ophthalmologist. Journal Of Neuro-Ophthalmology, 36(1), 78-84. doi: 10.1097/wno.0000000000000332
- ↑ Biller, J., & Ferro, J. (2014). Neurologic aspects of systemic disease (pp. 595 a 605).
- ↑ Oo T. H. (2019). Diagnostic difficulties in pernicious anemia. Discovery medicine, 28(155), 247–253. 17. Ferrie, S. (2012). Case Report of Acute Thiamine Deficiency Occurring as a Complication of Vitamin-Free Parenteral Nutrition. Nutrition In Clinical Practice, 27(1), 65-68. doi: 10.1177/0884533611433332 18. Lieven, C., Hoegger, M., Schlieve, C., & Levin, L. (2006). Retinal Ganglion Cell Axotomy Induces an Increase in Intracellular Superoxide Anion. Investigative Opthalmology & Visual Science, 47(4), 1477. doi: 10.1167/iovs.05-0921 19. Means, R., & Fairfield, K. (2021). UpToDate. Retrieved 29 May 2021, from https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-vitamin-b12-and-folate-deficiency
- ↑ 17.0 17.1 Ferrie, S. (2012). Case Report of Acute Thiamine Deficiency Occurring as a Complication of Vitamin-Free Parenteral Nutrition. Nutrition In Clinical Practice, 27(1), 65-68. doi: 10.1177/0884533611433332
- ↑ Lieven, C., Hoegger, M., Schlieve, C., & Levin, L. (2006). Retinal Ganglion Cell Axotomy Induces an Increase in Intracellular Superoxide Anion. Investigative Opthalmology & Visual Science, 47(4), 1477. doi: 10.1167/iovs.05-0921
- ↑ 19.0 19.1 Means, R., & Fairfield, K. (2021). UpToDate. Retrieved 29 May 2021, from https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-vitamin-b12-and-folate-deficiency
- ↑ 20.0 20.1 Vallurupalli Anusha (2021) Pernicious Anemia/Megaloblastic Anemia. Conn's Current Therapy 2021, 457-460. Elsevier, Inc.
- ↑ Bensky, M., Ayalon-Dangur, I., Ayalon-Dangur, R., & Naamany, E. (2019). Comparison of sublingual vs. intramuscular administration of vitamin B12 for the treatment of patients with vitamin B12 deficiency. Drug Delivery And Translational Research, 9(3), 625-630. doi: 10.1007/s13346-018-00613-y
- ↑ Sharma, P., & Sharma, R. (2011). Toxic optic neuropathy. Indian journal of ophthalmology, 59(2), 137–141. https://doi.org/10.4103/0301-4738.77035
- ↑ Feibel, R., & Arch, J. (2018). Cuban Epidemic Optic Neuropathy (1991-1993) and José Saramago's Novel Blindness (1995). American Journal Of Ophthalmology, 193, xix-xxvii. doi: 10.1016/j.ajo.2018.06.006