Myelinated Retinal Nerve Fiber Layer
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Myelinated Retinal Nerve Fiber Layer
Myelinated retinal nerve fiber layers (MRNF) are retinal nerve fibers anterior to the lamina cribrosa that, unlike normal retinal nerve fibers, have a myelin sheath. Clinically, they appear to be gray-white well-demarcated patches with frayed borders on the anterior surface of the neurosensory retina.[1][2] [3]While MRNF are typically located adjacent to the optic disc,[4] they can appear at any location in the retina with retinal nerve fiber layers, such as the fovea.[5] MRNF are present in 0.57 to 1% of the population and can occur bilaterally in approximately 7% of affected patients.[4][6] Most patients with MRNF are asymptomatic; however, some patients have associated ocular findings including axial myopia, amblyopia, and strabismus.[4][6] Though rare, familial cases of MRNF have been reported both in isolation and in combination with ocular and systemic syndromes.[7] MRNF are typically present at birth and are static lesions, but a few cases of acquired and progressive lesions in both childhood and adulthood have been described. Disappearance of MRNF have also been reported after surgery and insults to the optic nerve.[8]
International Classification of Disease
ICD-9 377.49 Other disorders of optic nerve
ICD-10 H35.89 Defect, defective retinal nerve bundle fibers
History
The German pathologist Rudolf Virchow was the first to describe myelinated retinal nerve fibers, writing in 1856 that the “retina was white, very thick and wrinkled. Macula was normal and near the optic disc, though more deeply situated, were thick, opaque, chalk-white spots, which spread around the disc in the shape of a star, so that when I wanted to draw the line between the disc and macula on each side of the two had the same divergence. In the other eye, I found, without much surprise, in the same place, the ring around the disc with a width of 2–2, 5 mm, regressing towards the outside”.[1]
Epidemiology
Elbaz et. al [9]conducted a population-based observational cohort study among white Europeans and found the prevalence of MRNF was 0.4%. MRNF was positively associated with a history of stroke, but had no association with other cardiovascular conditions, age, sex, or ocular factors, such as refractive error, visual acuity, central corneal thickness, and intraocular pressure. Similarly, Nangia et. al [10]reported a prevalence of MRNF to be 0.58% among adult Indians and found no association with age, visual acuity, or intraocular pressure. However, they found MRNF to be significantly associated with hyperopic refractive error.
The Beijing Eye Study [11]reported a similar prevalence of MRNF of 0.4%. The 10-year follow-up found no new MRNF cases, MRNF enlargement in all previously reported cases, and an association between MRNF and higher serum LDL concentration.
Pathophysiology
Axonal myelination in the human central nervous system is a complex, orderly process carried out by oligodendrocyte progenitor cells, which migrate under the influence of neuro-hormonal signals to generate oligodendrocytes that produce myelin. Retinal ganglion cell myelination proceeds from the lateral geniculate nucleus anteriorly toward the globe.[12] Myelination along the visual pathway is first seen in the eighth month of gestation, and typically reaches the posterior globe around the time of birth with virtually all fibers reaching complete myelination by age 7 months.[12] Normally, the myelination process stops at this level; some postulated explanations for this observation are the presence of the structure of the lamina cribrosa, the leakage of plasma proteins from the choroidal circulation inducing the differentiation of oligodendrocytes, and factors from type 1 astrocytes blocking oligodendrocyte migration.[13][14] The prevailing theory suggests that ectopic oligodendrocyte progenitor cells could lead to MRNF, either before the lamina cribrosa is formed or from an insult impairing the lamina cribrosa.[15] Although the exact causes remain unknown, MRNF occur when the myelination process extends past the lamina cribrosa and is visible on fundus examination.
Histopathology
Histopathological analysis demonstrates that myelinated fibers are not confined to a patch or fascicle, and single myelinated fibers can be found in between fascicles of unmyelinated fibers.[13] Both myelinated and unmyelinated fibers within a region of MRNF have been shown to be larger in diameter than fibers within normal retina. Also, notably, a decreased population of retinal ganglion cells have been noted to be present within the MRNF along with decreased width of the underlying inner and outer plexiform layers of the retina.[13] There is a relative paucity of cell nuclei and no microscopic evidence of inflammation within the region of MRNF. Although some MRNF may appear macroscopically contiguous with the optic disc, one histological study demonstrated that the region of myelination was not contiguous with that of the optic nerve.[13] In 12% of cases, two distinct lesions were observed.[6] No abnormalities of the cribriform plate have been described in eyes with MRNF.
Genetics
Genetic control of myelination of mature retinal ganglion cells is largely unknown and an active area of research.[16][17]
Familial cases of isolated MRNF have been reported, including a family with two generations of 10 cases and in a mother and daughter with bilateral MRNF.[7][18]
Familial cases associated with other disorders have also been described. An autosomal recessive syndrome consisting of growth retardation, alopecia, pseudoanodontia, and optic atrophy (GAPO syndrome) can also include MRNF, hypertelorism, and glaucoma.[19] A heritable syndrome of vitreoretinal degeneration, posterior subcapsular cataract, skeletal abnormalities, and MRNF has also been described.[20]
A patient with Albright hereditary osteodystrophy was also found to have MRNF.[21]
Diagnosis
Clinical Presentation
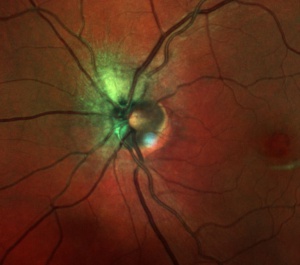
The majority of cases of MRNF are diagnosed incidentally in asymptomatic, healthy individuals by ophthalmoscopy. The appearance is typically one of a distinct peripapillary white striated patch with feathered borders approximately one disc diameter in size or larger (Figure 1).
Figure 1. Multicolor image of myelination of the RNFL.
Ophthalmic Imaging Characteristics
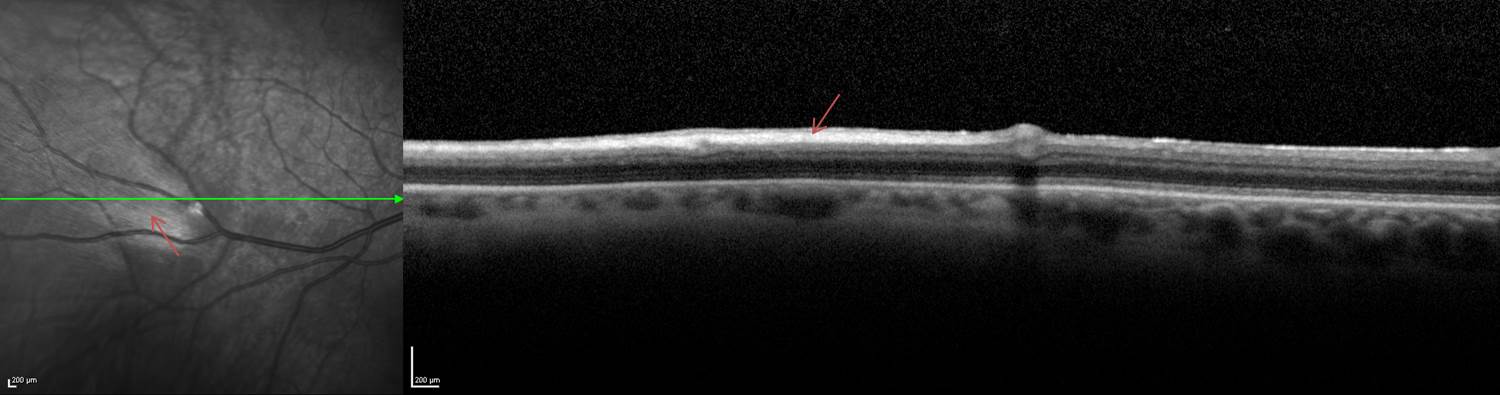
On infrared and red-free imaging, MRNF appears white, which is likely due to the high lipid content of myelin.[22] Myelin blocks detection of underlying fluorescent material, thus appearing dark on fundus autofluorescence (FAF). On optical coherence tomography (OCT), MRNF appears as a thickened and hyperreflective retinal nerve fiber layer (RNFL) (Figure 2). OCT may also show axon displacement towards the vitreous body due to the increased volume of myelin sheaths, [22]along with partial displacement of radial peripapillary capillaries with increased vessel density at the optic nerve head level and decreased density at the radial peripapillary capillary level. [23]
Figure 2. OCT in which red arrows identify the hyperreflective appearance of a myelinated retinal nerve fiber layer.
Conditions associated with myelination of the RNFL
MRNF are often isolated but may be associated with ipsilateral myopia, amblyopia, strabismus and other ocular conditions (Table 1). Strabismus was found in 66% with MRNF in one review.[24] Visual acuity is usually not affected; however, if a sufficient number of myelinated fibers are present, a relative scotoma may develop corresponding to the location of the MRNF. These scotomas are typically smaller than the size of the MRNF patch would suggest.[6][25] Visual acuity and prognosis depend on the severity of ocular complications or associated syndromes.
Rarely, bilateral acquired progressive MRNFL may occur in patients without an underlying pathology[26].
Ocular associations with myelination of the RNFL
| Anterior segment: |
|---|
| Refractive and Sensorimotor: |
| Optic nerve associated: |
| Uveal and Retinal: |
|
Systemic associations with myelination of the RNFL
Systemic syndromes that have been associated with MRNF include Turner syndrome,[46] epilepsy,[30] trisomy 21, and craniosynostosis.[47][6]
Conditions associated with acquired and progressive myelination of the RNFL
There are a few case reports of acquired and progressive myelination in childhood, adolescence, and adulthood.[36] These cases are associated with blunt trauma, optic nerve sheath fenestration, optic nerve drusen, family history of optic nerve hypoplasia in an unaffected child, Arnold-Chiari malformation associated with hydrocephalus, neurofibromatosis type I, and Gorlin-Goltz (basal cell nevus) syndrome , and Leber’s hereditary optic neuropathy.[34][36][46][48][49][50][51][52][53]
Conditions associated with loss of myelination of the RNFL
The disappearance of MRNF has also been reported and associated with several neurologic, inflammatory, and retinal diseases. It is hypothesized that the disappearance of the MRNF signals pathologic degeneration of the retinal nerve axons. The neurological disease associations include pituitary adenoma, optic neuritis, acute optic neuropathy, and primary open angle glaucoma.[54][55][56][57][58] Apparent demyelination of a MRNF in a patient with Behçet disease after recurrent episodes of papillitis and vitritis has been described, as has a MRNF in a patient who underwent plaque radiotherapy for choroidal melanoma.[59][60] In addition, retinal conditions such as branch retinal artery occlusion, central retinal artery occlusion, diabetic retinopathy, and pars plana vitrectomy for epiretinal membrane have been associated with disappearance of MRNF.[61][62][63][8]
Management
MRNF are typically benign but can be mistaken for other potentially serious conditions. A complete blood count may be helpful when considering a neoplastic infiltrate. The hyperreflectivity on OCT can mimic findings of retinal vascular occlusion or cotton wool spot, so ophthalmoscopy and fluorescein angiography can aid in distinguishing an embolic phenomenon. In young children, extensive MRNF may be mistaken for retinoblastoma, which must be distinguished by careful ophthalmoscopy (often under anesthesia) and possible additional imaging, such as ocular ultrasound, OCT, and FAF.[22] If gross visual defects are present, formal visual field testing is warranted to rule out a concomitant neuro-ophthalmologic issue, as visual defects in MRNF are usually mild.
Management of MRNF is focused on serial eye examinations assessing for and treating associated conditions. Myopia should be treated with refractive correction. If significant anisometropia is present, correction with glasses may not be tolerated secondary to aniseikonia, and contact lenses should be prescribed. Childhood amblyopia should be treated to optimize visual development.[4][62] Strabismus should be managed with the usual protocols, and patients often respond well to surgical realignment, although long-term results may be less predictable if significant underlying amblyopia is present. Argon photocoagulation has been described to address retinal vascular complications, such as neovascularization and vitreous hemorrhage.[15]
It is important to recognize the generally benign nature of MRNF to avoid superfluous medical testing. It is helpful to document a MRNF with imaging as certain conditions can be associated with the loss of myelination, as described above. Occasionally MRNF is referred for leukocoria. Careful observation of the feathering of the myelination along the nerve fiber layer can distinguish it from concerning diagnoses that can cause leukocoria, such as retinoblastoma.
References
- ↑ Jump up to: 1.0 1.1 Virchow VR. Zur pathologischen anatomic der netzaut und des scherven. Virchows Arch Pathol Anat. 1856;10:170–193.
- ↑ Gradle HS. The Blind Spot: III. The Relation of the Blind Spot to Medullated Nerve Fibers in the Retina. Journal of the American Medical Association. 1921;77(19):1483–7.
- ↑ Panigrahi A, Singh A, Gupta V. Syndrome of Myelinated Nerve Fibers, Hyperopia, Strabismus, and Amblyopia. Ophthalmol Retina. 2022 Dec;6(12):1153. doi: 10.1016/j.oret.2022.10.003. Epub 2022 Nov 4. PMID: 36344423.
- ↑ Jump up to: 4.0 4.1 4.2 4.3 Kodama T, Hayasaka S, Setogawa T. Myelinated retinal nerve fibers: prevalence, location and effect on visual acuity. Ophthalmologica. Journal international d’ophtalmologie. International journal of ophthalmology. Zeitschrift für Augenheilkunde. 1990;200(2):77–83. Available at: http://www.ncbi.nlm.nih.gov/pubmed/2338989. Accessed July 20, 2013.
- ↑ Ozates S, Teke MY. Ring-shaped myelinated retinal nerve fibers at fovea. Indian J Ophthalmol. 2017;65(7):630-632. doi:10.4103/ijo.IJO_120_17
- ↑ Jump up to: 6.0 6.1 6.2 6.3 6.4 6.5 Straatsma BR, Foos RY, Heckenlively JR, Taylor GN. Myelinated retinal nerve fibers. American journal of ophthalmology. 1981;91(1):25–38. Available at: http://www.ncbi.nlm.nih.gov/pubmed/7234927. Accessed July 20, 2013.
- ↑ Jump up to: 7.0 7.1 Funnell CL, George NDL, Pai V. Familial myelinated retinal nerve fibres. Eye (London, England). 2003;17(1):96–7. Available at: http://www.ncbi.nlm.nih.gov/pubmed/12579180. Accessed July 20, 2013.
- ↑ Jump up to: 8.0 8.1 Williams AJ, Fekrat S. Disappearance of myelinated retinal nerve fibers after pars plana vitrectomy. American journal of ophthalmology. 2006;142(3):521–3. Available at: http://www.ncbi.nlm.nih.gov/pubmed/16935613. Accessed July 20, 2013.
- ↑ Elbaz H, Peto T, Butsch C, et al. PREVALENCE AND ASSOCIATIONS OF MYELINATED RETINAL NERVE FIBERS: Results From the Population-Based Gutenberg Health Study. Retina. 2016;36(12):2364-2370. doi:10.1097/IAE.0000000000001093
- ↑ Nangia V, Jonas JB, Khare A, Bhate K, Agarwal S, Panda-Jonas S. Prevalence of myelinated retinal nerve fibres in adult Indians: the Central India Eye and Medical Study. Acta Ophthalmol. 2014;92(3):e235-e236. doi:10.1111/aos.12118
- ↑ Pan Z, Wei CC, Peng X, et al. Myelinated Retinal Nerve Fiber Progression in a 10-Year Follow-Up. The Beijing Eye Study 2001/2011. Am J Ophthalmol. 2021;230:68-74. doi:10.1016/j.ajo.2021.04.018
- ↑ Jump up to: 12.0 12.1 Magoon EH, Robb RM. Development of Myelin in Human Optic Nerve and Tract: A Light and Electron Microscopic Study. Archives of Ophthalmology. 1981;99(4):655–659. Available at: http://archopht.jamanetwork.com/article.aspx?articleid=633760. Accessed July 22, 2013.
- ↑ Jump up to: 13.0 13.1 13.2 13.3 FitzGibbon T, Nestorovski Z. Morphological consequences of myelination in the human retina. Experimental eye research. 1997;65(6):809–19. Available at: http://www.ncbi.nlm.nih.gov/pubmed/9441705. Accessed July 20, 2013.
- ↑ Perry VH, Lund RD. Evidence that the lamina cribrosa prevents intraretinal myelination of retinal ganglion cell axons. Journal of neurocytology. 1990;19(2):265–72. Available at: http://www.ncbi.nlm.nih.gov/pubmed/2358833. Accessed July 22, 2013.
- ↑ Jump up to: 15.0 15.1 Ramkumar HL, Verma R, Ferreyra HA, Robbins SL. Myelinated Retinal Nerve Fiber Layer (RNFL): A Comprehensive Review. Int Ophthalmol Clin. 2018 Fall;58(4):147-156. doi: 10.1097/IIO.0000000000000239. PMID: 30239369.
- ↑ Wegner M. A matter of identity: transcriptional control in oligodendrocytes. Journal of molecular neuroscience : MN. 2008;35(1):3–12. Available at: http://www.ncbi.nlm.nih.gov/pubmed/18401762. Accessed May 28, 2013.
- ↑ Howng SYB, Avila RL, Emery B, et al. ZFP191 is required by oligodendrocytes for CNS myelination. Genes & development. 2010;24(3):301–11. Available at: http://genesdev.cshlp.org/content/24/3/301.long. Accessed May 22, 2013.
- ↑ Francois J. Myelinated nerve fibres. In: Heredity in Ophthalmology. St Louis, MO: Mosby; 1961:494–496.
- ↑ Bozkurt B, Yildirim MS, Okka M, Bitirgen G. GAPO syndrome: four new patients with congenital glaucoma and myelinated retinal nerve fiber layer. American journal of medical genetics. Part A. 2013;161(4):829–34. Available at: http://www.ncbi.nlm.nih.gov/pubmed/23494824. Accessed July 20, 2013.
- ↑ Traboulsi EI, Lim JI, Pyeritz R, Goldberg HK, Haller JA. A new syndrome of myelinated nerve fibers, vitreoretinopathy, and skeletal malformations. Archives of ophthalmology. 1993;111(11):1543–5. Available at: http://www.ncbi.nlm.nih.gov/pubmed/8240111. Accessed July 20, 2013.
- ↑ Ramkumar HL, Verma R, Ferreyra HA, Robbins SL. Myelinated Retinal Nerve Fiber Layer (RNFL): A Comprehensive Review. Int Ophthalmol Clin. 2018 Fall;58(4):147-156. doi: 10.1097/IIO.0000000000000239. PMID: 30239369.
- ↑ Jump up to: 22.0 22.1 22.2 Shelton JB, Digre KB, Gilman J, Warner JEA, Katz BJ. Characteristics of myelinated retinal nerve fiber layer in ophthalmic imaging: findings on autofluorescence, fluorescein angiographic, infrared, optical coherence tomographic, and red-free images. JAMA ophthalmology. 2013;131(1):107–9. Available at: http://www.ncbi.nlm.nih.gov/pubmed/23307221. Accessed June 30, 2013.
- ↑ Holló G. Influence of myelinated retinal nerve fibers on retinal vessel density measurement with AngioVue OCT angiography. Int Ophthalmol. 2016;36(6):915-919. doi:10.1007/s10792-016-0207-6
- ↑ Tarabishy AB, Alexandrou TJ, Traboulsi EI. Syndrome of myelinated retinal nerve fibers, myopia, and amblyopia: a review. Survey of ophthalmology. 52(6):588–96. Available at: http://www.ncbi.nlm.nih.gov/pubmed/18029268. Accessed June 18, 2013.
- ↑ Jump up to: 25.0 25.1 Miller NR. Clinical neuro-ophthalmology. 4th ed. (Wilkins W and, ed.). Baltimore; 1982:367–9.
- ↑ Alexis JA, Lock JH, Cheong TZ, Gollschewsky JR. Without a Cause: Bilateral Acquired Progressive Myelinated Retinal Nerve Fiber Layers. J Neuroophthalmol. 2023 Dec 5. doi: 10.1097/WNO.0000000000002051. Epub ahead of print. PMID: 38048173.
- ↑ Williams TD. Medullated retinal nerve fibers: speculations on their cause and presentation of cases. American journal of optometry and physiological optics. 1986;63(2):142–51. Available at: http://www.ncbi.nlm.nih.gov/pubmed/3953757. Accessed July 22, 2013.
- ↑ Duke-Elder S. Congenital deformities. In: Duke-Elder S, ed. St. Louis: Mosby, CV; 1963:646–651.
- ↑ Leozappa M, Ciani S, Ferrari TM. Corneal cross-linking for the treatment of keratoconus in a patient with ipsilateral myelinated retinal nerve fiber layer. Case REp Ophthalmol 2011;2:99-104
- ↑ Jump up to: 30.0 30.1 30.2 Kiso K. Beitrage zur Kenntis von der Vererbung der markhaltigen Sehnervenfasern der netzhaut. Graefes Arch Clin Exp Ophthalmol. 1928;120:154–174.
- ↑ Jump up to: 31.0 31.1 31.2 Straatsma BR, Heckenlively JR, Foos RY, Shahinian JK. Myelinated retinal nerve fibers associated with ipsilateral myopia, amblyopia, and strabismus. American journal of ophthalmology. 1979;88(3 Pt 1):506–10. Available at: http://www.ncbi.nlm.nih.gov/pubmed/484678. Accessed July 21, 2013.
- ↑ Schmidt D, Meyer JH, Brandi-Dohrn J. Wide-spread myelinated nerve fibers of the optic disc: do they influence the development of myopia? International ophthalmology. 20(5):263–8. Available at: http://www.ncbi.nlm.nih.gov/pubmed/9112197. Accessed July 21, 2013.
- ↑ Merritt JC. Myelinated nerve fibers associated with afferent pupillary defect and amblyopia. Journal of pediatric ophthalmology. 14(3):139– 40. Available at: http://www.ncbi.nlm.nih.gov/pubmed/915641. Accessed July 27, 2013.
- ↑ Jump up to: 34.0 34.1 Ali BH, Logani S, Kozlov KL, Arnold AC, Bateman B. Progression of retinal nerve fiber myelination in childhood. American Journal of Ophthalmology. 1994;118:515–517.
- ↑ Gharai S, Prakash G, Kumar D, Jacob S, Agarwal A, Arora V. Spectral domain optical coherence tomographic characteristics of unilateral peripapillary myelinated retinal nerve fibers involving the macula. Journal of AAPOS. 2010;14(5):432–434.
- ↑ Jump up to: 36.0 36.1 36.2 Jean-Louis G, Katz BJ, Digre KB, Warner JE, Creger DD. Acquired and progressive retinal nerve fiber layer myelination in an adolescent. American journal of ophthalmology. 2000;130(3):361–2. Available at: http://www.ncbi.nlm.nih.gov/pubmed/11020421. Accessed July 20, 2013.
- ↑ Eide N. Retinal break in an area with medullated nerve fibres. Acta ophthalmologica. 1986;64(3):271–3. Available at: http://www.ncbi.nlm.nih.gov/pubmed/3751515. Accessed July 21, 2013.
- ↑ Hubbard GB, Thomas MA, Grossniklaus HE. Vitreomacular traction syndrome with extensively myelinated nerve fibers. Archives of ophthalmology. 2002;120(5):670–1. Available at: http://www.ncbi.nlm.nih.gov/pubmed/12003629 Accessed July 21, 2013.
- ↑ Karadimas P, Kapetanios A, Panayotidhou E, Bouzas EA. Epiretinal membrane occurring with myelinated retinal nerve fibers and vascular abnormalities. Retina (Philadelphia, Pa.). 2003;23(6):880–1. Available at: http://www.ncbi.nlm.nih.gov/pubmed/14707848. Accessed July 21, 2013.
- ↑ Jump up to: 40.0 40.1 Berliner ML. Medullated nerve fibers associated with choroiditis: report of a case with preliminary studies on the cause of the apparance of medullated nerve fibers in the retina. Archives of Ophthalmology. 1931;6(3):404–413. Available at: http://archopht.jamanetwork.com/article.aspx?articleid=609280. Accessed July 23, 2013.
- ↑ Jackson E. Uveitis with opaque optic nerve fibers. Am. J. Ophthal. 1918;1(448).
- ↑ Jump up to: 42.0 42.1 Rosen B, Barry C, Constable IJ. Progression of myelinated retinal nerve fibers. American Journal of Ophthalmology. 1999;127(4):471–473. Available at: http://dx.doi.org/10.1016/S0002-9394(98)00377-8. Accessed July 24, 2013.
- ↑ Mehta JS, Raman J, Gupta N, Sinha A. Retinal vascular anomalies in acquired myelinated nerve fibres. Acta ophthalmologica Scandinavica. 2003;81(3):311–2. Available at: http://www.ncbi.nlm.nih.gov/pubmed/12780415. Accessed July 21, 2013.
- ↑ Jump up to: 44.0 44.1 Leys AM, Leys MJ, Hooymans JM, et al. Myelinated nerve fibers and retinal vascular abnormalities. Retina (Philadelphia, Pa.). 1996;16(2):89–96. Available at: http://www.ncbi.nlm.nih.gov/pubmed/8724950. Accessed July 20, 2013.
- ↑ Jump up to: 45.0 45.1 Silvestri G, Sehmi K, Hamilton P. Retinal vascular abnormalities. A rare complication of myelinated nerve fibers? Retina (Philadelphia, Pa.). 1996;16(3):214–8. Available at: http://www.ncbi.nlm.nih.gov/pubmed/8789859. Accessed July 21, 2013.
- ↑ Jump up to: 46.0 46.1 Aaby AA, Kushner BJ. Acquired and progressive myelinated nerve fibers. Archives of ophthalmology. 1985;103:542–544.
- ↑ Garcia GA, Tian JJ, Apinyawasisuk S, Kim S, Akil H, Sadun AA. Clues from Crouzon: Insights into the potential role of growth factors in the pathogenesis of myelinated retinal nerve fibers. J Curr Ophthalmol. 2016;28(4):232-236. Published 2016 Aug 27. doi:10.1016/j.joco.2016.07.008
- ↑ Parulekar M V, Elston JS. Acquired retinal myelination in neurofibromatosis 1. Archives of ophthalmology. 2002;120(5):659–5. Available at: http://www.ncbi.nlm.nih.gov/pubmed/12003622. Accessed July 21, 2013.
- ↑ Baarsma GS. Acquired medullated nerve fibres. The British journal of ophthalmology. 1980;64(9):651. Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1043786&tool=pmcentrez&rendertype=abstract. Accessed July 21, 2013.
- ↑ Kushner BJ. Optic nerve decompression. Arch Ophthalmol. 1979;97:1459–1461.
- ↑ De Jong PT, Bistervels B, Cosgrove J, de Grip G, Leys A, Goffin M. Medullated nerve fibers. A sign of multiple basal cell nevi (Gorlin’s) syndrome. Archives of ophthalmology. 1985;103(12):1833–6. Available at: http://www.ncbi.nlm.nih.gov/pubmed/4074174. Accessed July 21, 2013.
- ↑ Verma R, Goyal D, Goel S. Myelinated Retinal Nerve Fiber Layer in Idiopathic Intracranial Hypertension: A Rare and Challenging Scenario. Neurol India. 2023 Sep-Oct;71(5):1120-1121. doi: 10.4103/0028-3886.388079. PMID: 37929501.
- ↑ Gicquel JJ, Salama B, Mercié M, Bonneau D, Dighiero P. Myelinated retinal nerve fibres loss in Leber's hereditary optic neuropathy. Acta Ophthalmol Scand. 2005;83(4):517-518. doi:10.1111/j.1600-0420.2005.00470.
- ↑ A. S. Schwund Markhaltiger Nervenfasern in der Netzhaut bei intzundlicher Atrophie des Sehnervern in Folges eines Tumor oerebri. Z. Augenheilkd. 1905;13:739–50.
- ↑ Gupta A, Khandalavala B, Bansal RK, Jain IS, Grewal SP. Atrophy of myelinated nerve fibers in pituitary adenoma. Journal of clinical neuro-ophthalmology. 1990;10(2):100–2. Available at: http://www.ncbi.nlm.nih.gov/pubmed/2141848. Accessed July 21, 2013.
- ↑ Sharpe JA, Sanders MD. Atrophy of myelinated nerve fibres in the retina in optic neuritis. The British journal of ophthalmology. 1975;59(4):229–32. Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1042599&tool=pmcentrez&rendertype=abstract. Accessed July 20, 2013.
- ↑ Schachat AP, Miller NR. Atrophy of myelinated retinal nerve fibers after acute optic neuropathy. American journal of ophthalmology. 1981;92(6):854–6. Available at: http://www.ncbi.nlm.nih.gov/pubmed/7315937. Accessed July 20, 2013.
- ↑ Katz SE, Weber PA. Photographic documentation of the loss of medullated nerve fibers of the retina in uncontrolled primary open angle glaucoma. Journal of glaucoma. 1996;5(6):406–9. Available at: http://www.ncbi.nlm.nih.gov/pubmed/8946297. Accessed July 22, 2013.
- ↑ Chavis PS, Tabbara KF. Demyelination of retinal myelinated nerve fibers in Behcet’s disease. Documenta ophthalmologica. Advances in ophthalmology. 1998;95(2):157–64. Available at: http://www.ncbi.nlm.nih.gov/pubmed/10431799. Accessed July 21, 2013.
- ↑ Mashayekhi A, Shields CL, Shields JA. Disappearance of retinal myelinated nerve fibers after plaque radiotherapy for choroidal melanoma. Retina (Philadelphia, Pa.). 2003;23(4):572–3. Available at: http://www.ncbi.nlm.nih.gov/pubmed/12972781. Accessed July 20, 2013.
- ↑ Teich SA. Disappearance of myelinated retinal nerve fibers after a branch retinal artery occlusion. American journal of ophthalmology. 1987;103(6):835–7. Available at: http://www.ncbi.nlm.nih.gov/pubmed/3591888. Accessed July 20, 2013.
- ↑ Jump up to: 62.0 62.1 R. B. Schwund markhaltiger Nervenfasern in der Netzhaut nach Embolie der Art. Centralies retinae. Albrecht von Graefes Arch. Ophthalmol. 1922;107(10).
- ↑ Gentile RC, Torqueti-Costa L, Bertolucci A. Loss of myelinated retinal nerve fibres in diabetic retinopathy. The British journal of ophthalmology. 2002;86(12):1447. Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1771408&tool=pmcentrez&rendertype=abstract. Accessed July 20, 2013.
Acknowledgements
The authors thank Penny Coppernoll-Blach and the UCSD Library staff for their help in facilitating the literature review necessary for this paper. Special thanks to Giulio Barteselli and Gabriel Balea for the ophthalmic photography presented here. We thank Christopher Rugaber, OD, Faculty of Optometry, Rangsit University, Pathum Thani,Thailand for his valuable suggestions to improve this wiki page.