Müller’s Muscle-Conjunctival Resection (MMCR) Blepharoptosis Repair
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
First described by Putterman and Urist[1] in 1975, Muller's Muscle-Conjunctival Resection (MMCR) was a modification of the Fasanella-Servat[2] procedure, which involves the excision of 3mm of tarsus. MMCR is a posterior eyelid ptosis repair technique, which spares the tarsus. The advantage of this modification is that tarsus can be used in later procedures and the Meibomian glands remain undisturbed. Some argue that the MMCR allows for normal eyelid contour,[1] while some argue that good eyelid contour can still be achieved with a Fasanella-Servat.[3] Over the years, there have been several modifications on the technique originally described and multiple methods for determining amount of resection . The mechanism by which MMCR elevates the lid has been a matter of some contention. Some authors state that the effect of the MMCR is actually from advancement of levator aponeurosis.[4] Other authors question this theory and claim that MMCR lid elevation results from a shortening of the posterior lamella, as well as plication (not resection) of the levator aponeurosis and muscle. This latter claim is based on the easy separation of Muller’s muscle from the aponeurosis, as well as histologic evidence of an intact, levator aponeurosis with plication in cadaver eyelids, which had undergone MMCR.[5][6]
Regardless of mechanism, MMCR remains an effective tool for the repair of certain cases of blepharoptosis. Some argue that a MMCR can give more predictable results compared to levator aponeurotic procedures[1] and is cosmetically valuable, as it leaves no visible scar. Opponents argue that many patients requiring ptosis repair have concurrent dermatochalasis and addressing this ptosis via an anterior approach, such as a levator advancement, more sensibly pairs with concomittant blepharoplasty.
Indications
This procedure is a good choice for a mild to moderate amount of ptosis with good levator function and a response to phenylephrine.[7] Since it is a posterior approach and leaves no visible scar, MMCR is a great option in patients without excess upper eyelid skin.
After the surgeon determines that a patient has ptosis and is medically stable, the surgeon must determine if the patient is a good candidate for MMCR. An ideal candidate for this procedure has a small amount of ptosis (historically, approximately 2-3mm), which improves with phenylephrine testing, and has good levator function (>10mm). If there is excess skin that is to be addressed, blepharoplasty will need to be done in addition to the MMCR.
If the patient has moderate to poor levator function (<10mm), MMCR surgery may not adequately address the ptosis. Instead, the surgeon will need to consider options, such as an external levator resection or frontalis sling, depending on the level of levator function loss.
Phenylephrine test (PE test)
Müller's muscle is a smooth muscle in the upper eyelid that is innervated by the sympathetic nervous system. When the muscle is contracted, it elevates the lid approximately 2.5mm. Phenylephrine is an adrenergic stimulant, which stimulates the sympathetically innervated Müller’s muscle to contract and thus elevate the lid.[8]
To perform the PE test, first measure the MRD1 prior to instilling any drops. Second, place a topical proparacaine or tetracaine drop into the affected eye. Then, a drop of 2.5% or 10% Phenylephrine is placed onto the desired eye and this is repeat every minute for a total of 3 times. [7][8] After 5 minutes after receiving the last drop of phenylephrine, the MRD1 is re-measured . Some surgeons believe that the degree of improvement of the MRD1 from the pre-PE test MRD1 directs the amount to be resected, while others believe the test not necessary.
A comparison between 2.5% and 10% phenylephrine did find a difference in the elevation of the upper lid of less than 0.4 mm between the two concentrations, but such a small difference is not felt to be significant enough to cause a change in the surgical outcome.[9]
Some have found that the PE test is not an absolute guarantee of success and feel that this lack of prediction supports that excision of Muller’s muscle alone is not the sole source of the ptosis correction and that some amount of levator advancement may be in part responsible for the effect seen in this procedure.[10]
Keep in mind that the PE test can be used to unmask contralateral ptosis as well.[7] It is easier to demonstrate this to the patient and discuss the existence and management options of a contralateral ptosis masked by Hering’s law of equal innervation.
PE Test Formulae
There are several formulas which attempt to correlate the amount of resection to be performed from the PE test results:
- Putterman and Fett:[11] 8.5mm resection if 10% phenylephrine raises the lid to exactly where you want it, adding or subtracting 1mm of resection for every 0.5mm of desired increased of decreased lid height desired, up to a range of 6.5mm to 9.5mm
- Weinstein and Buerger:[12] 8mm resection for each 2mm of desired lid elevation and add or subtract 1mm resection for each 0.25mm height difference change in final lid position
- Dresner:[6] 4mm resection for 1mm of ptosis, 6mm for 1.5mm, 8mm for 2, 10mm for 3mm, 11-12mm for >3mm. If the PE test undercorrects, 1-2mm of additional resection was included. It is hypothesized that perhaps in these cases, the MM has undergone fatty infiltration and is not as responsive.
- Perry et al:[13] 9mm resection + X mm of tarsus excision (x = distance of undercorrection after PE testing). Authors feel that 9mm of resection should result in similar lid height as 10% PE test. Thus, any decrease in height during the PE can be accounted for by tarsal excision (up to a max of 2.5mm of excised tarsus).
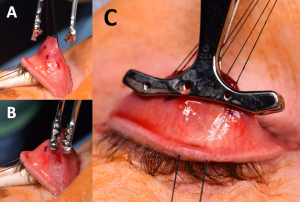 Figure 6A) A Putterman clamp is then placed so that the tented apex of the tented Muller’s/conjunctiva complex is between the clamp. B,C) Care must be taken to ensure the teeth are placed at the superior margin of the tarsus only, and that tarsus has not been inadvertently incorporated into the clamp. Photo courtesy of Adham al Hariri, M.D.
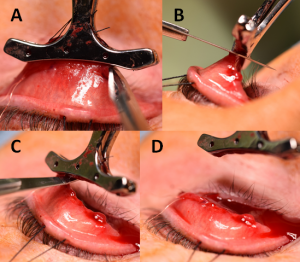
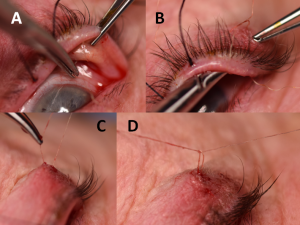
Figure 6A) A Putterman clamp is then placed so that the tented apex of the tented Muller’s/conjunctiva complex is between the clamp. B,C) Care must be taken to ensure the teeth are placed at the superior margin of the tarsus only, and that tarsus has not been inadvertently incorporated into the clamp. Photo courtesy of Adham al Hariri, M.D. Figure 7A,B) 6-0 plain gut suture being used to sew in an anterior to posterior fashion through Müller’s/conjunctiva 1.5-2.0mm below the clamp. This A-P sewing is begun at the lateral edge of the eyelid and sewn to the medial edge, then the course reversed and sewn back in the same manner laterally to finish back at the lateral edge (C,D) Photo courtesy of Adham al Hariri, M.D.
Figure 7A,B) 6-0 plain gut suture being used to sew in an anterior to posterior fashion through Müller’s/conjunctiva 1.5-2.0mm below the clamp. This A-P sewing is begun at the lateral edge of the eyelid and sewn to the medial edge, then the course reversed and sewn back in the same manner laterally to finish back at the lateral edge (C,D) Photo courtesy of Adham al Hariri, M.D.
Surgical Procedure
Step 1[8]
Local anesthesia consists of injecting 2% lidocaine with 1:100,000 Epi for hemostasis into the upper lid palpebral conjunctiva and also the skin of the upper eyelid (Figure 1). General anesthesia can also be used if necessary because, unlike in levator advancements, the procedure does not require the patient to be cooperate intra-operatively for surgical adjustments.
Step 2[1][8][11]
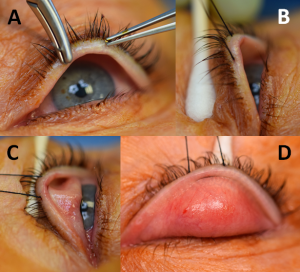
A 4-0 silk traction suture (Figure 2A) is placed in the middle of upper lid at its margin passing through tarsus and skin and the upper lid is then everted over a Desmarres retractor or cotton-tip applicator (Figure 2B,C). This exposes the upper lid tarsal and palpebral conjunctiva (Figure 2D).
Step 3[1][8][11]
The superior border of the everted tarsus is visualized. Some surgeons mark this with electrocautery or a marking pen (Figure 3A).
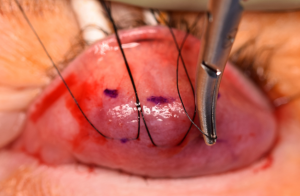
In this example, a 10mm resection is desired. Calipers are used to measure half of the distance (5mm in this example) of the desired resection starting from the superior border of the tarsus (Figure 3B). After measuring this distance, marks are made 5mm (one medial, one lateral and one middle) from the superior border of the tarsus on the palpebral conjunctiva. A 6-0 Silk running suture is then passed superficially through these marks through the conjunctiva and superficial Müller’s muscle (Figure 4). This suture is then pulled ventrally towards the ceiling, elevating conjunctiva and Müller’s muscle (Figure 5).
Some surgeons directly clamp the Putterman Muller's resection clamp onto the area to be resected without placement of this 6-0 silk traction suture, taking care to avoid incorporating tarsus.
With Müller’s muscle firmly adherent to conjunctiva, Müller’s muscle should separate easily from the levator aponeurosis to which it is loosely adherent, ensuring that during the resection very little levator aponeurosis is removed. Thus, it is felt that the main reason this procedure works is that there is shortening of the posterior lamella, advancement of the levator palpebrae superioris muscle and plication (not resection) of the levator aponeurosis.[5][6][11]
Step 4[1][8][11]
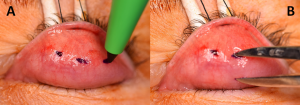
Now elevating the conjunctiva and Müller’s muscle with the suture, a Putterman Müller’s muscle–conjunctival resection clamp is placed at the border of the superior tarsus and clamped shut, sandwiching the conjunctiva and Müller’s muscle (Figure 6A).
This clamp has three needles which penetrate through the squeezed conjunctiva and Müller’s muscle so that they do not slip out of the clamp, ensuring the correct desired amount of tissue will be resected (Figure 6B).
Occasionally, tarsus may inadvertently be incorporated into the clamp, which is not desired (Figure 6C). If the tarsus has been incorporated, the margin of the lid may be distorted. To evaluate for this, the Desmarres retractor or q-tip is removed, the lid is inverted back into normal position, and the contour of the margin is assessed. If the contour is not normal, tarsus may have been inadvertently grasped by the clamp and the clamp readjusted to allow the tarsus to be pulled gently free.
Step 5
With the clamp successfully in place, the clamp is pulled to the ceiling, elevating the tuft of conjunctiva and Müller’s muscle. (Figure 7A-B) A 6-0 plain gut suture is passed through skin laterally right above the upper eyelid crease, full thickness through the lid, exiting the conjunctiva near the lateral edge of the superior border of the tarsus. This 6-0 plain gut is then passed medially in a running fashion 1.5-2.0mm below the inferior margin of the clamp passing full thickness through the conjunctiva and Müller’s muscle. Once the suture reaches the medial edge of the clamp, the suture is then sewn back laterally, again in a running fashion to the lateral edge of the clamp (Figure 7C-D).
Step 6[1][8][11]
A #15 or #11 blade (Figure 8) is used to excise the Müller’s muscle-conjunctivo complex enclosed within the clamp from the lid by cutting the complex between the clamp and the sutures, taking care to avoid incidentally cut the plain gut sutures.
Step 7[1][8][11]
The suture is then passed back through the palpebral conjunctiva, exiting through the skin near where the suture enters. The Desmarres’ retractor or cotton-tip is then used to re-evert the lid and closure of conjunctiva defects is completed via tightening and tying down the 6-0 running plain gut suture to ensure the borders of the conjunctival wound are approximated. To prevent rubbing of the suture knot on the globe surface, the suture knot is externalized onto the skin. The traction suture is then removed from the upper eyelid (Figure 9).
Step 8[8]
If being performed, a blepharoplasty can be completed at this point.
Post-op care
Post-operative care varies. Some surgeons recommend antibiotic ophthalmic ointment onto the eye and to the skin suture(s) three times per day for a total of one week and some surgeons do not use any antibiotic ointment. Most follow up for their first post-operative visit after about one to two weeks.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Putterman AM, Urist MJ. Müller’s muscle-conjunctival resection. Arch Ophthalmol. 1975;93(8):619-623.
- ↑ Fasanella RM, Servat J. Levator resection for minimal ptosis: another simplified operation. Arch Ophthalmol. 1961;65:493-496.
- ↑ Choudhary MM, Chundury R, McNutt SA, Perry JD. Eyelid Contour Following Conjunctival Müllerectomy With or Without Tarsectomy Blepharoptosis Repair. Ophthal Plast Reconstr Surg. 2016 Sep-Oct;32(5):361-5
- ↑ Mercandetti M, Putterman AM, Cohen ME, et al. Internal levator advancement by Müller’s muscle-conjunctival resection: technique and review. Arch Facial Plast Surg. 2001;3:104–10.
- ↑ 5.0 5.1 Marcet MM, Setabutr P, Lemke BN et al. Surgical Microanatomy of the Müller Muscle-Conjunctival Resection Ptosis Procedure. Ophthal Plast Reconstr Surg. 2010Sep-Oct;26(5):360-4
- ↑ 6.0 6.1 6.2 Dresner SC. Further modifications of the Müller’s muscle-conjunctival resection procedure for blepharoptosis. Ophthal Plast Reconstr Surg 1991;7:114–22.
- ↑ 7.0 7.1 7.2 Allen RC, Saylor MA, Nerad JA. The current state of ptosis repair: a comparison of internal and external approaches. Curr Opin Ophthalmol. 2011 Sep;22(5):394-9.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 8.8 Sajja K, Putterman AM. Müller’s Muscle Conjunctival Resection Ptosis Repair in the Aesthetic Patient. Saudi J Ophthalmol. 2011 Jan;25(1):51–60
- ↑ Glatt HJ, Fett DR, Putterman AM. Comparison of 2.5% and 10% phenylephrine in the elevation of upper eyelids with ptosis. Ophthalmic Surg 1990; 21:173–176.
- ↑ Ben Simon GJ, Lee S, Schwarcz RM, McCann JD, Goldberg RA. Müller's muscle-conjunctival resection for correction of upper eyelid ptosis: relationship between phenylephrine testing and the amount of tissue resected with final eyelid position. Arch Facial Plast Surg. 2007 Nov-Dec;9(6):413-7.
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 11.6 Putterman AM, Fett DR. Müller’s muscle in the treatment of upper eyelid ptosis: a ten-year study. Ophthalmic Surg. 1986;17(6):354-360.
- ↑ Weinstein GS, Buerger GF Jr. Modifications of the Müller’s muscle-conjunctival resection operation for blepharoptosis. Am J Ophthalmol. 1982;93(5):647-651
- ↑ Perry JD, Kadakia A, Foster JA. A new algorithm for ptosis repair using conjunctival Müllerectomy with or without tarsectomy. Ophthal Plast Reconstr Surg. 2002; 18(6):426-429.