All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
ICD-9:
- 371.8 Other corneal disorders
ICD-10:
- H18.891 Other specified disorders of cornea, right
- H18.892 Other specified disorders of cornea, left
- H18.893 Other specified disorders of cornea, bilateral
Disease
Interface fluid syndrome is a rare, but vision-threatening postoperative complication of LASIK surgery characterized by fluid collection in the flap interface that was first described by Lyle and Jin.[1] Other common nomenclature for IFS includes pressure-induced stromal keratitis (PISK) and pressure-induced interface keratitis.[2] It has also been noted in small incision lenticule (SMILE) surgery and lamellar keratoplasty.[3][4]
Etiology
IFS usually results from increased intraocular pressure (IOP) that is triggered from postoperative steroid use.[2][5] However, any condition that increases IOP is a potential cause of IFS in patients with prior LASIK or SMILE surgery. IFS have been noted in cases of uveitis and Posner Schlossman Syndrome.[6][7] Other inflammatory conditions reported with IFS include CMV endotheliitis, [8]trauma, infectious keratitis,[9] and toxic anterior segment syndrome.[10] IFS has also been noted in cases with corneal endothelial decompensation, such as Fuch’s corneal endothelial dystrophy.[11] It has also been noted many years after DSAEK surgery and[12] vitrectomy. [13]
Incidence
Gab-Alla reported the incidence of IFS in Egyptians to be 2.9%; however, the incidence is likely a lot lower in general population as this study used a more potent topical steroid (dexamethasone) in the post-LASIK management.[14]
Risk Factors
Patients that have underwent surgery that can cause a potential space between stroma and the flap are at risk for IFS. Interface fluid syndrome is most common in LASIK patients, but it has also been noted after SMILE and lamellar keratoplasty.[1][3][2] Other risks factors include high intraocular pressure and endothelial cell dysfunction.[6][7][11][15][16]
Stages
Dawson et al proposed a staging system in 2007:[17]
- Stage 0: Normal LASIK cornea
- Stage 1: mild to moderate swelling of LASIK interface with no to minimal interface haze
- Stage 2: moderate to severe swelling of LASIK interface associated with moderate to severe diffuse, smudgy, nongranular interface haze and occasional small fluid pockets
- Stage 3: confluent, large, diffuse fluid pocket accumulating between LASIK flap and residual stromal bed with scattered surrounding haze.
Pathophysiology
Increased intraocular pressure seems to be essential to mechanism of IFS. A study of human eye bank corneas proposed 2 mechanisms of IFS.[17] The first entails increased intraocular pressure and the second is due to corneal endothelial dysfunction. Increased IOP causes shift of fluid through the endothelium from zones of high pressure to low pressure, and in the case of LASIK, interface space is the area of low pressure and subsequently where fluid collects in patients with IFS.[18] [19]
Diagnosis
History
Patient usually presents with blurred vision a few days to a few months after uncomplicated LASIK surgery. There are cases reported 1 to 16 years after LASIK surgery.[7][15] Patients may also complain of pain and photophobia. The typical presentation is a patient with history of uneventful LASIK surgery who has been on topical steroids for extended period of time.
Physical examination
On exam, the vision can vary from mild impairment to hand motion vision. Intraocular pressure is increased but can be falsely measured normal in patients with IFS.[20][21][22] IOP should be measure peripherally with tonopen or other tonometers that are less likely to be influenced by corneal rigidity. Goldmann applanation tonometry of central cornea may provide falsely low IOP reading due to easy compressibility of fluid-filled space.[23][24] Patient may also have anterior chamber inflammation. Corneal haze is present at interface wound. The amount of fluid at interface wound is variable and an obvious fluid layer may not always be visible at the slit lamp.[25]
Clinical diagnosis
Diagnosis is through clinical history and slit lamp examination and confirmed with OCT. Ancillary testing such as OCT and corneal densitometry may aid with diagnosis and monitoring clinical course.[2][26]
Diagnostic procedures
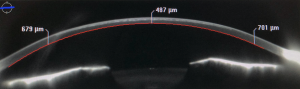
OCT or Optical coherence tomography
It can be useful to confirm interface fluid accumulation in the cap-bed interface and monitor the clinical course.[2]
Automated Scheimpflug densitometry program
One study showed that corneal densitometry can be useful for evaluating and grading IFS.[2]
Laboratory test
There are no specific tests for diagnosing IFS.
Differential diagnosis
- Diffuse Lamellar Keratitis (DLK) – Clinically, the slit lamp findings of DLK are similar to IFS. However, the presence of pain (present) , onset (2-5 days after LASIK), IOP (normal), and presence of inflammation (present) may help differentiate DLK from IFS.[2]
- Microbial Keratitis – IOP is usually normal and presence of infiltrate in infectious keratitis versus haze in IFS
- Epithelial Ingrowth – epithelial cells at interface without any interface fluid. Normal IOP and minimal effect on visual acuity.
Management
Timely diagnosis of IFS is crucial to preventing permanent vision loss. Although IFS typically occurs 1-3 days postoperatively, IFS has been known to occur several years after LASIK, so it is important to able to discern IFS.[7][15] [27][28],[29] Post-LASIK patients on chronic topical steroids should have their IOP monitored vigilantly and artificially low or normal IOP may be measured in corneas of IFS, so unconventional methods of measuring IOP should be used. In IFS with large fluid clefts, the cushioning effect of the interface fluid will give falsely low IOP readings. Peripheral IOP measurement or dynamic contour tonometry may be necessary. Due to the consequence of steroids on the pathophysiology, IFS must be differentiated from DLK as the treatment for DLK (steroids) will worsen IFS.
In most cases, management generally consists of cessation of topical steroids and starting IOP lowering agents. In some cases, surgical intervention was needed to lower the IOP.[11],[30] Shajari et al presented a case of IFS after LASIK that was managed with Descemet's membrane endothelial keratoplasty.[11]
IFS is commonly seen after LASIK; however, it can occur in many different types of corneal lamellar surgery. With the increasing popularity of SMILE, IFS should also be on the differential for post-SMILE complications.[3]
Complications
Glaucomatous optic neuropathy leading to decreased visual field and central visual acuity if not detected early and appropriately managed.[19]
Prognosis
If diagnosed early and appropriately managed, patients do well without any loss of visual acuity.
References
- ↑ 1.0 1.1 Lyle W.A., Jin G.J. Interface fluid associated with diffuse lamellar keratitis and epithelial ingrowth after laser in situ keratomileusis. J Cataract Refract Surg. 1999;25:1009–1012.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Randleman J.B., Shah R.D. LASIK interface complications: etiology, management, and outcomes. J Refract Surg. 2012;28:575–586.
- ↑ 3.0 3.1 3.2 Zheng K., Han T., Li M. Corneal densitometry changes in a patient with interface fluid syndrome after small incision lenticule extraction. BMC Ophthalmol. 2017;17(1):34
- ↑ Ramappa M., Bhalekar S., Chaurasia S., Mulay K., Trivedi R.H., Wilson M.E. Presumed allograft stromal rejection after deep anterior lamellar keratoplasty in a boy presenting with interface fluid syndrome. J AAPOS. 2013;17(5):554–557.
- ↑ Bamashmus M.A., Saleh M.F. Post-LASIK interface fluid syndrome caused by steroid drops. Saudi J Ophthalmol. 2013;27(2):125–128.
- ↑ 6.0 6.1 Goto S., Koh S., Toda R. Interface fluid syndrome after laser in situ keratomileusis following herpetic keratouveitis. J Cataract Refract Surg. 2013;39(8):1267–1270.
- ↑ 7.0 7.1 7.2 7.3 Jia Z, Zhao S, Wei R, Huang Y, Zhang C, Yang R. Interface fluid syndrome: A potential lifelong complication after LASIK. A case report. Am J Ophthalmol Case Rep. 2018;11:23-25.
- ↑ Tendolkar S, Murthy SI, Chandran K, Joseph J. Acute interface fluid syndrome after laser in situ keratomileusis in a case of cytomegalovirus (CMV) endotheliitis and secondary glaucoma. BMJ Case Rep. 2021 Apr 30;14(4):e236742. doi: 10.1136/bcr-2020-236742. PMID: 33931424; PMCID: PMC8098761.
- ↑ Kanduri V, Madduri B, Mohan N, Fernandes M. Multi-drug resistant Burkholderia cepacia keratitis following laser in situ keratomileusis complicated by interface fluid syndrome. Indian J Ophthalmol. 2020 Jul;68(7):1443-1444. doi: 10.4103/ijo.IJO_1633_19. PMID: 32587186; PMCID: PMC7574062.
- ↑ Galvis V, Berrospi RD, Tello A, Santaella G. Interface Fluid Syndrome (IFS) following Toxic Anterior Segment Syndrome (TASS): not related to high intraocular pressure but to endothelial failure. Saudi J Ophthalmol. 2019 Jan-Mar;33(1):88-93. doi: 10.1016/j.sjopt.2018.06.003. Epub 2018 Jul 7. PMID: 30930670; PMCID: PMC6424685.
- ↑ 11.0 11.1 11.2 11.3 Shajari M., Rafiezadeh P., Pavlovic I. Management of interface fluid syndrome after LASIK by descemet membrane endothelial keratoplasty in a patient with Fuchs' corneal endothelial dystrophy. J Refract Surg. 2017;33(5):347–350.
- ↑ Assayag E, Smadja D, Roditi E, Zadok D, Abulafia A, Weill Y. Interface Fluid Syndrome 2 Decades After Laser-Assisted In situ Keratomileusis. Eye Contact Lens. 2021 Feb 2.
- ↑ Bourdon H, Jaillant R, Baudouin C, Trinh L. Delayed interface fluid syndrome following vitrectomy. J Fr Ophtalmol. 2021 Mar;44(3):e163-e164. doi: 10.1016/j.jfo.2020.05.023. Epub 2020 Dec 14.
- ↑ Incidence of interface fluid syndrome after laser in situ keratomileusis in Egyptian patients. Clin Ophthalmol. 2017;11:613-618.
- ↑ 15.0 15.1 15.2 Ortega-Usobiaga J, Martin-Reyes C, Llovet-Osuna F, Damas-Mateache B, Baviera-Sabater J. Interface fluid syndrome in routine cataract surgery 10 years after laser in situ keratomileusis. Cornea. 2012;31(6):706–707.
- ↑ McLeod S.D., Mather R., Hwang D.G., Margolis T.P. Uveitis-associated flap edema and lamellar interface fluid collection after LASIK. Am J Ophthalmol. 2005;139(6):1137–1139.
- ↑ 17.0 17.1 Dawson D.G., Schmack I., Holley G.P., Waring G.O., 3rd, Grossniklaus H.E., Edelhauser H.F. Interface fluid syndrome in human eye bank corneas after LASIK: causes and pathogenesis. Ophthalmology. 2007;114(10):1848–1859.
- ↑ Moya Calleja T., Iribarne Ferrer Y., Sanz Jorge A., Sedó Fernandez S. Steroid-induced interface fluid syndrome after LASIK. J Refract Surg. 2009;25(2):235–239.
- ↑ 19.0 19.1 Hamilton D.R., Manche E.E., Rich L.F., Maloney R.K. Steroid-induced glaucoma after laser in situ keratomileusis associated with interface fluid. Ophthalmology. 2002;109:659–665.
- ↑ Park HJ, Uhm KB, Hong C. Reduction in intraocular pressure after laser in situ keratomileusis. Journal of cataract and refractive surgery. 2001;27:303–309.
- ↑ Wheeldon CE, Hadden OB, Niederer RL, McGhee CN. Presumed late diffuse lamellar keratitis progressing to interface fluid syndrome. Journal of cataract and refractive surgery. 2008;34:322–326.
- ↑ Fogla R, Rao SK, Padmanabhan P. Interface fluid after laser in situ keratomileusis. J Cataract Refract Surg. 2001;27(9):1526–1528.
- ↑ Levy Y., Zadok D., Glovinsky Y., Krakowski D., Nemet P. Tono-Pen versus Goldmann tonometry after excimer laser photorefractive keratectomy. J Cataract Refract Surg. 1999;25(4):486–491.
- ↑ Kohlhaas M., Spoerl E., Boehm A.G., Pollack K. A correction formula for the real intraocular pressure after LASIK for the correction of myopic astigmatism. J Refract Surg. 2006;22(3):263–267.
- ↑ Belin MW, Hannush SB, Yau CW, Schultze RL. Elevated intraocular pressure-induced interlamellar stromal keratitis. Ophthalmology. 2002;109:1929–1933.
- ↑ Senthil S., Rathi V., Garudadri C. Misleading Goldmann applanation tonometry in a post-LASIK eye with interface fluid syndrome. Indian J Ophthalmol. 2010;58(4):333–335.
- ↑ Smith RJ, Maloney RK. Diffuse lamellar keratitis. A new syndrome in lamellar refractive surgery. Ophthalmology 1998;105:1721–6.
- ↑ Kuo CY, Chang YF, Chou YB, Hsu CC, Lin PY, Liu CJ. Delayed onset of pressure-induced interlamellar stromal keratitis in a patient with recurrent uveitis: A case report. Medicine (Baltimore). 2017;96(48):e8958.
- ↑ Lee V, Sulewski ME, Zaidi A, et al. Elevated intraocular pressure-induced interlamellar stromal keratitis occurring 9 years after laser in situ keratomileusis. Cornea 2012;31:87–9.
- ↑ Luceri S1, Baksoellah Z, Ilyas A, Baydoun L, Melles GR. Interface Fluid Syndrome after laser in situ keratomileusis because of Fuchs endothelial dystrophy revesred by Descemet membrane Endothelial keratoplasty. Cornea. 2016 Dec;35(12):1658-1661.