All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Hoon Jung, MD,
Joobin Khadamy, MD, FEBO,
S. Grace Prakalapakorn, MD, MPH,
Michael T Yen, MD,
Hashem Abu Serhan
Assigned status Up to Date
by
Michael T Yen, MD on December 29, 2024.
The significance of numbers in routine clinical practice has grown exponentially. They guide disease diagnoses, treatment choices (in terms of kind, dosage, and duration), aid in surgical precision, determine implant specifications, and even influence follow-up schedules. Daily clinic procedures involve various biometric assessments, generating essential numerical data. In the realm of ophthalmology, sometimes, the sole focus for specialists is a single numeric value, such as normal corneal power, acceptable residual stromal bed levels, or specific anatomical reference values. Despite the advancement of search engines, procuring normal value ranges and their clinical implications remains a cumbersome task. Therefore, there's a strong appreciation among clinicians for a centralized repository of reference values in ophthalmology. This initiative aims to collect and present the latest reference values and their clinical relevance across various ophthalmic conditions. The primary source for these numbers is The American Academy of Ophthalmology's Basic and Clinical Science Course™ book series. Continuous contributions from all members are vital to maintain the page's accuracy and relevance.
Eye in Numbers
Adult Eye Volume
| Parameter
|
Measurement
|
| Adult eye volume
|
~6.5–7.0 mL
|
Axial Length (AL)
| Condition
|
Measurement
|
| Normal adult
|
23–25 mm
|
| High myopia (> −6 D)
|
>26 mm
|
| Pathologic myopia (> −8 D)
|
32.5 mm
|
| Microphthalmia
|
<21 mm (adults), <19 mm (1 year of age)
|
| Nanophthalmos
|
<18 mm (highly hyperopic eye)
|
Clinical Pearls for Axial Length:
* The standard Morcher CTR comes in three sizes based on uncompressed diameter, selected according to axial length (AL):
** 12.3 mm (compresses to 10 mm, Morcher 14): AL < 24 mm
** 13 mm (compresses to 11 mm, Morcher 14C): 24 mm < AL < 28 mm
** 14.5 mm (compresses to 12 mm, Morcher 14A): AL > 28 mm
* Implant size calculation: Axial length − 2 mm = implant diameter
** Subtract 1 mm from implant diameter for evisceration and for hyperopia
Transverse Diameter of the Globe
| Parameter
|
Measurement
|
| Transverse diameter (widest point)
|
~24 mm
|
Cornea
Corneal Diameter
| Category
|
Measurement
|
| Adults (horizontal)
|
12–12.5 mm
|
| Adults (vertical)
|
11 mm
|
| At birth
|
9.5–10.5 mm
|
Clinical Pearls for Corneal Diameter:
* To calculate ACIOL size: Horizontal white-to-white distance + 1 mm
* Congenital glaucoma:
** >12 mm horizontally in newborns
** >11.5 mm at birth
** >12.5 mm in 1-year-old children
** >13 mm in other children
* Buphthalmos (“bull’s-eye”): Horizontal corneal diameter >13 mm
* Megalocornea: >13 mm
* Microcornea: <10 mm
Note: Adult size is reached by age 2 years.
Consistency
| Parameter
|
Composition
|
| Corneal dry weight
|
70% type I collagen
|
Corneal Power
| Component
|
Power (D)
|
| Average (air-tear interface)
|
43 D
|
| Anterior
|
48–49 D
|
| Posterior
|
−5.8 to −6 D
|
Note: Posterior corneal surface contributes approximately 0.4 D of against-the-rule astigmatism.
Clinical Pearls for Corneal Power:
* Corneal plana: K < 43 D
* Keratoconus:
** Central K > 47.2 D
** Inferior-superior (I-S) difference: >1.4 D in 3 mm
** Asymmetric K > 0.92 D
* Risk for buttonhole with LASIK: K > 48 D
* Risk for free flap with LASIK: K < 40 D
* Predicting final K after LASIK:
** Myopia: Flattening of 0.80 D per D treated; avoid final K < 35–36 D
** Hyperopia: Steepening of 1.00 D per D treated; avoid final K > 50 D
* Intacs in advanced keratoconus: K > 60.00 D has lower likelihood of functional vision improvement; corneal transplant may be needed
| Asphericity:
|
Q value
|
| Normal cornea is prolate
|
−0.26
|
Corneal Thickness
| Structure/Location
|
Thickness
|
| Central corneal thickness (CCT)
|
540 μm
|
| Near limbus
|
700 μm – 1.0 mm
|
| Limbal relaxing incision (LRI) depth
|
500–550 μm
|
| Epithelium
|
50 μm (10% of corneal thickness)
|
| Bowman layer
|
10 μm (8–14 μm)
|
| Descemet membrane (at birth)
|
3 μm
|
| Descemet membrane (adults)
|
10–12 μm
|
Clinical Pearls for Corneal Thickness:
* Risk for decompensation after intraocular surgery: CCT > 640 μm
* Limbal/corneal relaxing incisions (LRI/CRI) depth: 500–600 μm (90% depth)
* Arcuate or straight incisions (AK) depth: 99% depth (avoid >90° arc due to decreased efficacy and increased instability)
* Radial keratotomy depth: 85–90% corneal thickness
* Phototherapeutic keratectomy (PTK) depth: Ablate pathology in anterior 1/3 (~180 μm)
* Contraindication for LASIK residual stromal bed (RSB): RSB < 250 μm or < 50% of original CCT
* Contraindication for LASIK: CCT < 480 μm
* Intacs: Lamellar channel at ~70% stromal depth (CCT − 50–60 μm)
* Contraindication for ring/ICR: Thickness < 450 μm
* Raindrop Near Vision Inlay: Placed at depth ≥ 200 μm
* Contraindication for crosslinking (CXL): Thickness < 400 μm (some protocols allow > 300 μm)
* LASIK flap thickness:
** Ultrathin: 80–100 μm
** Thin: 120 μm
** Standard: 120–180 μm
* Using same microkeratome blade for fellow eye: Flap 10–20 μm thinner
* Automated therapeutic lamellar keratoplasty: Microkeratome set for 130–450 μm
Endothelial Layer Characteristics
Endothelial Cell Density (ECD)
| Age/Group
|
ECD (cells/mm²)
|
| At birth
|
4000
|
| Young adults
|
3000
|
| Healthy 60 years old
|
2500–1500
|
Endothelial Cell Morphology
| Parameter
|
Normal Range
|
| Mean cell size/area
|
150–350 μm²
|
| Coefficient of variation (CV) index
|
<0.40
|
| Hexagonality (6A)
|
>50%
|
Clinical Pearls for Endothelial Layer:
* Not appropriate for donation: ECD < 2000 cells/mm²
* Risk for decompensation after intraocular surgery: ECD < 1000 cells/mm²
* Contraindication for intraocular surgery: ECD < 500 cells/mm²
* Risk for corneal decompensation after intraocular surgery:
** Polymegathism: CVI > 0.4
** Pleomorphism: Hexagonality < 50%
* Note: ECD decreases approximately linearly until age 60, then at a lower rate, so older adults (70–80 years) may have more cells than expected.
Conjunctiva
| Feature
|
Measurement/Note
|
| Limbus integrity
|
At least 25%–33% must remain intact for normal resurfacing
|
| Giant papillae size
|
>1 mm
|
| Margin of excision with SCC
|
Wide excision (4 mm margin)
|
Clinical Pearls
Note: Limbus integrity is critical in chemical burns or ocular surface tumor surgeries.
Sclera
| Location
|
Thickness (mm)
|
| Posterior to recti insertions (thinnest)
|
0.3
|
| At the equator
|
0.4–0.5
|
| Anterior to muscle insertions
|
0.6
|
| Around optic nerve head (thickest)
|
1.0
|
Clinical Pearls for Sclera:
* The thinnest part (0.3 mm, posterior to recti insertions) is significant in blunt trauma and scleral laceration.
* For drainage of suprachoroidal hemorrhage, sclerotomy is placed 5–6 mm posterior to the limbus, primarily in the inferotemporal quadrant.
Anterior chamber
| Parameter
|
Measurement
|
| Anterior chamber depth (ACD)
|
3 mm
|
| Critical angle for total internal reflection (air-tear interface)
|
46 degrees
|
Clinical Pearls
* If ACD <2.0 mm: Risk factors for angle closure
* If ACD <3.2 mm: Increased risk of endothelial/iris trauma with phakic IOL placement
Aqueous humor
| Parameter
|
Measurement
|
| Total volume
|
260 μL
|
| Daytime production rate
|
2-3 μL/min (renews every 100 min)
|
| Nighttime production rate
|
1 μL/min (renews every 200 min)
|
| Ascorbic acid concentration
|
10-50× plasma levels
|
Chambers
| Chamber
|
Volume
|
| Anterior chamber (AC)
|
200 μL
|
| Posterior chamber (PC)
|
60 μL
|
Clinical pearls:
AC tap/paracentesis Withdraw 0.05-0.1 cc using 27-30G needle near limbus
Phakic IOL
| Parameter
|
Measurement
|
| Vault
|
250-750 μm (0.5-1.5× CCT)
|
Clinical pearls:
* Vault <90 μm increases anterior subcapsular cataract risk
Intraocular pressure (IOP)
| Population
|
Normal range (mmHg)
|
| Adults
|
10-21
|
| 7-year-olds
|
14
|
| Newborns
|
10-12
|
* Pediatric glaucoma: IOP >10-15 mmHg considered abnormal
* Congenital glaucoma infants: Typically 30-40 mmHg (20 mmHg under anesthesia)
Episcleral venous pressure
| Measurement
|
Value
|
| Normal EVP
|
6-9 mmHg
|
Pupil
| Parameter
|
Measurement
|
| Light reflex development
|
≥30 weeks GA
|
| Diameter (light)
|
2-4 mm
|
| Diameter (dark)
|
4-8 mm
|
| Airy-disk size
|
1.2 mm
|
| Anisocoria threshold
|
>1 mm difference
|
Iris
| Parameter
|
Measurement
|
| Thickness
|
0.35-0.45 mm[1]
|
Clinical pearls:
* Abnormal thickness: >0.7 mm
* Iridotomy size: ≥150-200 μm (ideal 500 μm)[2]
Lens
| Parameter
|
Measurement
|
| Refractive index
|
1.4
|
| Dioptric power
|
20 D
|
| Diameter (neonate)
|
6.5 mm
|
| Diameter (adult)
|
8.54-9.70 mm
|
Capsule
| Location
|
Thickness
|
| Anterior
|
14.0-15.5 μm
|
| Posterior (thinnest)
|
2.8-4.0 μm
|
| Post. pre-equatorial (thickest)
|
23 μm
|
Clinical pearls:
* Optimal capsulorhexis: 5.5-6 mm
* Piggyback IOL: 1.2× RE (myopia), 1.5× RE (hyperopia)
Ciliary body
| Feature
|
Count
|
| Ciliary processes
|
70
|
Pars plana
| Population
|
Injection site
|
| Phakic adults
|
3.5-4 mm posterior
|
| Pseudophakic/aphakic
|
3-3.5 mm posterior
|
| 1-6 months
|
1.5 mm
|
| 6-12 months
|
2 mm
|
| 1-2 years
|
2.5 mm
|
| 2-6 years
|
3 mm
|
Ora serrata
| Location
|
Distance from limbus
|
| Nasal
|
5.75 mm
|
| Temporal
|
6.50 mm
|
Clinical pearls:
* Prefer temporal quadrant for intravitreal injections
Vascularization
| Event
|
Timing
|
| Nasal retina maturation
|
36 weeks GA
|
| Temporal retina maturation
|
40 weeks GA*
|
| Full vascularization
|
3 months postnatal
|
| Choroid development
|
16 weeks GA
|
Clinical pearls:
* Begin ROP screening from observing temporal area.
Vitreous
| Structure
|
Volume
|
| Vitreous cavity
|
5-6 mL
|
| Vitreous body
|
4 mL
|
Clinical pearls: Vitreous sampling
* Pars plana vitrectomy: 0.2-0.5 mL
* Vitreous tap: 0.1-0.3 mL
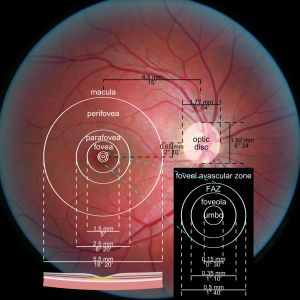
Macula
| Parameter
|
Measurement
|
| Diameter
|
5.5 mm
|
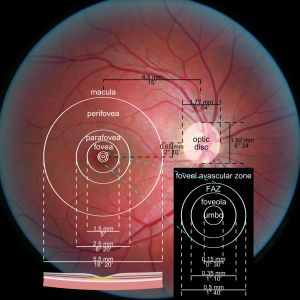
Macula, perifovea, parafovea, fovea, foveola.
* Distance between optic disc-macula >3 DD suggests optic nerve hypoplasia
Fovea
| Feature
|
Measurement
|
| Diameter
|
1.5 mm (5°)
|
| Photostress recovery time
|
>90 seconds indicates maculopathy
|
Clinical pearls:
* Monovision syndrome: 8 prism diopter deviation
* Rhodopsin sensitivity: 510 nm (green light)
Foveal avascular zone (FAZ)
| Parameter
|
Measurement
|
| Diameter
|
500 μm (1:40°)
|
Clinical pearls: Avoid laser therapies in FAZ
Foveola
| Parameter
|
Measurement
|
| Location (temporal to disc)
|
4.0-4.5 mm (15°)
|
| Location (inferior to disc)
|
0.8 mm (2:10°)
|
| Diameter
|
350 μm
|
Umbo
| Parameter
|
Measurement
|
| Diameter
|
150 μm
|
ParaFovea
| Parameter
|
Measurement
|
| Ring width
|
0.5 mm
|
| Outer radius
|
2.5 mm
|
| Inner radius
|
1.5 mm
|
PeriFovea
| Parameter
|
Measurement
|
| Ring width
|
1.5 mm
|
| Outer radius
|
5.5 mm
|
| Inner radius
|
2.5 mm
|
Optic nerve
| Parameter
|
Measurement
|
| Adult axons
|
1.2-1.5 million
|
| Gestational axons (16 weeks)
|
3.7 million
|
| Head diameter
|
1.5-2.2 mm
|
| Cup-to-disc ratio (normal)
|
<0.5
|
| Total length
|
50 mm
|
Clinical pearls:
* NAION risk: Cup-to-disc ratio ≤0.2 ("disc-at-risk")
* Enucleation in retinoblastoma: Excise ≥10 mm ON
* Atrophy timeline: 6 weeks post-damage
Retinal pigment epithelium (RPE)
Clinical pearls:
* PED >600 μm height risks RPE tear post anti-VEGF
* EOG Arden ratio:
- Normal: >2
- Best disease: ≤1.5
Choroid
| Feature
|
Risk Threshold
|
| Nevus thickness
|
>2 mm (melanoma risk)
|
Vascular anatomy
| Structure
|
Count
|
| Short posterior ciliary arteries
|
20
|
| Short posterior ciliary nerves
|
10
|
| Long ciliary arteries/nerves
|
2
|
| Muscle
|
Active Length
|
Tendon Length*
|
| Rectus muscles
|
40 mm
|
4.5-7 mm
|
| Superior oblique
|
32 mm
|
26 mm
|
| Inferior oblique
|
37 mm
|
1 mm
|
| Levator
|
40 mm
|
14-20 mm
|
(*)Shortest tendon (I M SIL Live So):
- IO:1 mm
- MR:4.5 mm (shortest between rectus muscles)
- Overal length:
- Longest: SO (58 mm) >Levator>others>Shortest: IO (38 mm)
Insertion distances
| Muscle
|
Distance from Limbus
|
| MR
|
5.5 mm
|
| IR
|
6.5 mm
|
| LR
|
6.9 mm
|
| SR
|
7.7 mm
|
Arc of contact
| Muscle
|
Contact Length
|
| IO*
|
15 mm
|
| LR
|
12 mm
|
| SO
|
7-8 mm
|
| MR**
|
7 mm
|
(*)IO:(Longest)
(**)MR:(Shortest)
- LR inserts 2 mm more superior than MR.
- EOM penetrate the tenon capsule 10 mm posterior to their insertions.
Orbit
| Parameter
|
Measurement
|
| Volume
|
<30 cm³
|
| Posterior globe-optic foramen
|
18 mm
|
| Interpupillary distance
|
60-62 mm
|
| Intercanthal distance
|
30-31 mm
|
Clinical pearls:
* Exophthalmos: ≥2 mm asymmetry
* Hypertelorism: IPD >2 SD above mean
* Telecanthus: Intercanthal >2 SD
Ciliary ganglion
| Location
|
Measurement
|
| Anterior to annulus of Zinn
|
1 cm
|
Tear and Tear-Film
| Parameter
|
Measurement
|
| Tear lake volume
|
7-10 µL
|
| Eyedrop retention rate
|
20% (10 µL of 50 µL)
|
| Tear production onset
|
20 days postnatal
|
| Lacrimal gland maturation
|
6 weeks postnatal
|
Clinical pearls:
* One eyedrop bottle = 5 mL ≈ 100 drops (50 µL/drop)
* Atropine 1% example: 0.5 mg/drop → 50 mg/bottle
* Artificial tears ideal properties:
- pH 7.0-8.2
- Osmolarity ≤302 mOsm/L
Tear Composition
| Layer
|
Component
|
Percentage
|
| Aqueous
|
Water
|
98%
|
| Total protein
|
2%
|
| Lysozyme
|
30% of protein
|
| Lactoferrin
|
-
|
| Immunoglobulins
|
IgA, IgG
|
| pH
|
7.2
|
| Osmolarity
|
302 mOsm/L
|
| Basal secretion
|
2 µL/min
|
| Layer
|
Production Rate
|
| Mucin (inner)
|
2-3 mL/day
|
Dry Eye Diagnostics
| Test
|
Normal
|
Abnormal
|
| Dye disappearance test (DDT)
|
≤5 min
|
>5 min (NLDO)
|
| Tear breakup time
|
≥10 sec
|
<10 sec
|
| Tear meniscus height
|
≥0.3 mm
|
<0.2 mm
|
| Phenol red thread
|
≥10 mm/15s
|
<10 mm/15s
|
| MMP-9 level
|
≤40 ng/mL
|
>40 ng/mL
|
Schirmer Tests
| Test
|
Method
|
Interpretation
|
| Basic Secretion
|
Anesthetized
|
<3 mm/5 min = ATD
|
| Schirmer I
|
Non-anesthetized
|
<5.5 mm/5 min = ATD
|
| Schirmer II
|
Nasal stimulation
|
<15 mm/2 min = Reflex defect
|
Key:
ATD = Aqueous Tear Deficiency
NLDO = Nasolacrimal Duct Obstruction
MMP-9 = Matrix Metalloproteinase-9
Developmental Timeline
| Milestone
|
Timing
|
Clinical Significance
|
| First tears
|
20 days
|
NLDO signs appear
|
| Lacrimal function
|
6 weeks
|
Full secretory capacity
|
Eyelid Anatomy
| Structure
|
Measurement
|
| Upper tarsal height
|
11 mm (3× lower tarsus)
|
| Lower tarsal height
|
4 mm
|
| Palpebral fissure height
|
10-11 mm (women: 9-11 mm, men: 7-8 mm)
|
| MRD1
|
3-4 mm
|
| MRD2
|
5 mm
|
| Eyelid length
|
30 mm
|
Clinical pearls:
* MRD1 ↑ with lid retraction, ↓ with ptosis
Arterial Supply
| Vascular Structure
|
Location
|
| Marginal arcade*
|
2-3 mm superior to lash line
|
| Superior peripheral arcade
|
Within/between Müller's muscle & levator aponeurosis
|
Clinical pearls:
(*) Marginal arcade avoid them while performing tarsoraphy.
Upper Lid Crease
| Measurement
|
Distance
|
| Brow to crease
|
10 mm
|
| Crease to margin (women)
|
8-10 mm
|
| Crease to margin (men)
|
6-8 mm
|
Clinical pearls:
** Congenital ptosis: Absent lid crease
**Involutional ptosis: Elevated crease position
Blinking Frequency and Clinical Significance
| Blinking Frequency
|
Normal Range
|
Clinical Significance
|
| Normal
|
12-20 blinks per minute
|
Maintains tear film stability, prevents dryness, and clears debris from the ocular surface.
|
| Reduced (Hypoblinking)
|
<10 blinks per minute
|
Seen in Parkinson’s disease, ocular surface disease, or neurogenic causes; increases risk of dry eye syndrome and exposure keratopathy.
|
| Increased (Hyperblinking)
|
>20-25 blinks per minute
|
Associated with blepharospasm, ocular irritation, tic disorders, or psychological stress.
|
| Asymmetrical Blinking
|
Varies between eyes
|
Suggests facial nerve palsy (e.g., Bell’s palsy) or neuromuscular dysfunction affecting one eyelid.
|
Clinical Pearls:
* Normal blinking occurs every **3-5 seconds**, with complete closure ensuring corneal hydration.
* Incomplete blinking: can lead to exposure keratopathy and is commonly seen in lagophthalmos or after aggressive ptosis surgery.
* Patients with neurogenic hypoblinking (e.g., Parkinson’s) may require lubricating drops or eyelid training exercises to prevent corneal damage.
Levator Function
| Classification
|
Excursion
|
| Normal
|
>12 mm
|
| Fair
|
6-11 mm
|
| Poor
|
<6 mm
|
Levator Function and Surgical Guidelines
| Levator Function
|
Recommended Surgery
|
Indications
|
| Excellent (>12 mm)
|
Mild ptosis: Müller’s muscle resection or small levator advancement
|
Small droop, strong muscle, good phenylephrine test response
|
| Good (8-12 mm)
|
Levator advancement/resection for moderate ptosis
|
Aponeurotic or mild congenital ptosis with functional levator
|
| Fair (5-7 mm)
|
Moderate-to-severe ptosis: Levator resection (maximal if needed)
|
Levator has some function, can attempt resection but results may vary
|
| Poor (<4 mm)
|
Frontalis sling (bypassing weak levator function)
|
Severe congenital ptosis, third-nerve palsy, muscular dystrophy-related ptosis
|
Clinical pearls:
* Levator resection indicated when LF >4 mm
* Normal excursion: ~15 mm (range 12-18 mm)
Meibomian Glands
| Location
|
Gland Count
|
Secretory Rate
|
| Upper eyelid
|
25-40
|
1.0-1.4 μL/min
|
| Lower eyelid
|
20-30
|
0.8-1.2 μL/min
|
Eyelashes
| Parameter
|
Measurement
|
| Upper lid count
|
90-150
|
| Lower lid count
|
70-80
|
| Growth rate
|
0.12-0.15 mm/day
|
| Full regrowth time
|
6 weeks (intact follicle)
|
Clinical pearls:
* Post-epilation recovery: 6-12 weeks for full growth
* Repeated extension use may reduce lash density by 30-50%
* Bimatoprost increases length by 25-30% but may cause periocular pigmentation
Growth Cycle
| Phase
|
Duration
|
Characteristics
|
| Anagen
|
30-45 days
|
Active growth
|
| Catagen
|
2-3 weeks
|
Follicle regression
|
| Telogen
|
30-45 days
|
Resting/shedding
|
Biopsy Guidelines
Clinical pearls: Biopsy size and width of margins should be based on clinical presentation, level of suspicion, and risk factor analysis.
Ophthalmic Instruments
| Device
|
Specification
|
| Goldmann tonometer
|
3.06 mm applanated area
1.25g weight (5.5g total force)
|
| LASIK plume particles
|
0.22 µm size
|
| Surgical mask filtration
|
0.1 µm efficiency
|
Clinical pearls:
* LASIK safety:
** A canister mask will filter these particles down to 0.1 µm.
** The average particles produced in the LASIK plum are 0.22 µm.
** N95 masks filter 95% of 0.3µm particles
Volk Lens Factors
| Lens
|
Magnification Factor
|
Field Width
|
| 60D
|
1.0×
|
70°
|
| 78D
|
1.1×
|
85°
|
| 90D
|
1.3×
|
100°
|
Clinical pearls:
* 60D lens: 1:1 papilla-to-slit beam ratio at 16× magnification
Visual Acuity Testing
| Test
|
Parameter
|
Specification
|
| Pinhole
|
Optimal diameter
|
1.2 mm (corrects ≤3D)
|
| Pinhole
|
Diffraction limit
|
20/40 at 1.0 mm
|
Nystagmus Acuity Estimates
| Type
|
Visual Acuity
|
Characteristics
|
| Vertical OKN
|
≥20/400
|
Vertical nystagmus overlay
|
| Searching
|
<20/200
|
Roving eye movements
|
| Pendular
|
>20/200
|
Sinusoidal oscillation
|
| Jerk
|
20/60-20/100
|
Fast/slow phases
|
Preschool HOVT Norms
| Age
|
Snellen
|
Decimal
|
| 2.5y
|
20/63-20/30
|
0.33-0.66
|
| 5y
|
20/30-20/20
|
0.66-1.0
|
Duochrome Testing
| Source
|
Chromatic Interval
|
Wavelength Difference
|
| Commercial filters
|
0.50D
|
490nm vs 630nm
|
| Human eye (Fraunhofer)
|
1.5-3.0D
|
486nm (F) - 656nm (C)
|
| Human eye (Helmholtz)
|
1.8D
|
Photopic sensitivity peak
|
Clinical pearls:
* 80% patients prefer green focus at 0.25D over red[9][10]
* 1.0D hyperopia correction improves duochrome balance by 40%[11]
Time-Critical Ophthalmic Protocols
Emergency Interventions
| Condition
|
Time Window
|
Specifics
|
| Myocardial Infarction/Stroke/CRAO
|
≤90 min
|
Door-to-balloon/thrombolysis
|
| Sympathetic Ophthalmia
|
4-8 weeks (65% 2-8w, 90% <1y)
|
Latent period post-trauma
|
| Hyphema (Pediatric)
|
4-5 days
|
Surgical intervention threshold
|
| Hyphema (Sickle Cell)
|
>24h IOP >25 mmHg
|
Immediate surgery
|
| Perforating Trauma
|
5-14 days
|
Vitrectomy for PVR prevention
|
Surgical Timing
| Procedure
|
Minimum Wait
|
Details
|
| LASIK Re-treatment
|
3 months
|
Refractive stability required
|
| Surface Ablation Repeat
|
6-12 months
|
Haze resolution period
|
| Nerve Palsy Repair
|
9-12 months
|
Allow spontaneous recovery
|
| **Refractive Surgery Post-Pregnancy**
|
**3 months postpartum + breastfeeding cessation**
|
Hormonal stabilization
|
| Congenital Cataract (Uni)
|
<6 weeks
|
Prevent sensory nystagmus
|
| Congenital Cataract (Bi)
|
<8-10 weeks
|
Sequential within 2w (<2y) /4w (>2y)
|
| Artificial Iris Implant
|
≥16 years
|
Pediatric contraindication
|
Pharmacological Timelines
| Medication
|
Critical Duration
|
Effects
|
| **Topical Steroids**
|
>2w use → 5% IOP >31mmHg at 6w
≥18mo → Permanent damage
|
Monitor IOP q2w, If > 3 drops/d>3mo consider systemic
|
| Systemic Steroids (Immunosuppression)
|
>7.5mg/d >3mo
|
Threshold for alternative therapy
|
| Tetracaine
|
10-20s onset
|
10-20min duration
|
| **Retrobulbar Lidocaine (0.5-2%)**
|
5min onset
|
1-2hr akinesia
|
| Δ9-THC (Marijuana)
|
3-4hr
|
Impractical IOP control
|
Cycloplegics/Mydriatics (ASH-CT Mnemonic)
| Agent
|
Duration
|
Full Effect Onset
|
| **A**tropine
|
7-14d
|
60-120min
|
| **S**copolamine
|
4-7d
|
45min
|
| **H**omatropine
|
3d
|
30min
|
| **C**yclopentolate
|
24hr
|
60min
|
| **T**ropicamide
|
4-6hr
|
30min
|
Diagnostic Protocols
| Test
|
Protocol
|
Positive Criteria
|
| **Tensilon (Edrophonium)**
|
2+4+4mg IV + **Atropine pre-treatment**
|
≥2mm lid elevation
|
| **Neostigmine**
|
1.5mg IM + Atropine 0.6mg IV
|
Improvement in 30-45min
|
| Sleep Test
|
30min nap
|
Lid elevation + resolution
|
| Ice Pack Test
|
2min application
|
≥2mm improvement
|
Specialized Procedures
| Technique
|
Exposure Time
|
Clinical Application
|
| Absolute Alcohol (20%)
|
10–45s
|
Epithelial debridement
|
| Mitomycin C (0.02%)
|
12s–2min
|
Haze prevention
|
| **Photodynamic Therapy**
|
N/A
|
**5d strict sun avoidance**
|
Clinical Pearls:
1. **Steroid Response Gradation:**
- <2w: Rare IOP spikes
- 6w: 5% >31mmHg
- ≥18mo: 22% permanent damage
2. **MG Crisis Protocol:**
- Neostigmine 1.5mg IM + Atropine 0.6mg IV q4-6h
3. **ONTT Steroid Taper:**
- Prednisone 1mg/kg/day ×11d → 20mg day 12 → 10mg days 13-15
4. **GCA Biopsy:**
- 2-3cm specimen length (skip lesion prevention)
Disease Timelines & Definitions
| Condition
|
Time Criteria
|
Clinical Significance
|
| Apparent Optic Atrophy
|
6 weeks post-injury
|
Final functional assessment window
|
Uveitis Classification
| Type
|
Duration
|
Recurrence Pattern
|
| Acute
|
<3 months
|
Single episode
|
| Recurrent
|
<3 months/episode
|
>3 months between flares
|
| Chronic
|
>3 months
|
Persistent inflammation
|
Diabetic Retinopathy Screening
| Population
|
Initial Exam
|
Pregnancy Protocol
|
| Type 1 DM
|
3-5 years post-diagnosis
|
1st trimester
|
| Type 2 DM
|
At diagnosis
|
1st trimester
|
Clinical pearls:
* 15% of Type 1 DM develop DR within 5 years
* 20% of Type 2 DM have DR at diagnosis
* Monthly exams for proliferative DR in pregnancy
Intraocular Gas Dynamics
| Gas
|
Effective Tamponade
|
Retention Time
|
Key Properties
|
| SF₆
|
6 days
|
13 days (2-3w)
|
Non-expansile concentration
|
| C₂F₆
|
15 days
|
35 days (3-4w)
|
18% concentration expands 2×
|
| C₃F₈
|
30 days
|
65 days (6-8w)
|
14% concentration expands 4×
|
Clinical pearls:
* SF₆: Requires 5-day face-down positioning
* C₃F₈: 20% risk of transient IOP >30mmHg (monitor q4h first day)
* Gas-filled eyes contraindicated for air travel until 10% residual
Gas Selection Guide
| Clinical Scenario
|
Preferred Gas
|
Rationale
|
| Macula-on RD
|
SF₆
|
Short-term tamponade needed
|
| Giant retinal tear
|
C₂F₆
|
Moderate duration support
|
| Proliferative vitreoretinopathy
|
C₃F₈
|
Long-term stabilization
|
Key:
RD = Retinal Detachment
IOP = Intraocular Pressure
w = weeks
DM = Diabetes Mellitus
DR = Diabetic Retinopathy
- When different antiplatelets or anticoagulants should be paused before various intraocular or oculoplastic surgeries:
Timing of Pausing Antiplatelets and Anticoagulants Before Intraocular or Oculoplastic Surgery
| Medication |
Intraocular Surgery (e.g., Cataract, Glaucoma, Vitrectomy) |
Oculoplastic Surgery (e.g., Blepharoplasty, Ptosis repair) |
Comments
|
| Aspirin |
* |
7-10 days before |
*May continue in minor surgeries if risk of thromboembolism is high.
|
| Clopidogrel (Plavix) |
5-7 days before |
5-7 days before |
Consider bridging with low-dose aspirin if thromboembolic risk is high.
|
| Ticagrelor (Brilinta) |
5-7 days before |
5-7 days before |
Bridging therapy might be considered depending on the thromboembolic risk.
|
| Prasugrel (Effient) |
7-10 days before |
7-10 days before |
Typically requires longer cessation than clopidogrel due to higher potency.
|
| Warfarin (Coumadin) |
3-5 days before |
3-5 days before |
INR should be normalized (<1.5); consider bridging with LMWH if high risk.
|
| Dabigatran (Pradaxa) |
2-3 days before |
2-3 days before |
Consider longer cessation (4-5 days) in patients with renal impairment.
|
| Rivaroxaban (Xarelto) |
2-3 days before |
2-3 days before |
Discontinue 2 days before surgery for normal renal function; may require more if renal function is impaired.
|
| Apixaban (Eliquis) |
2-3 days before |
2-3 days before |
May consider 48-hour cessation, longer if impaired renal function.
|
| Edoxaban (Savaysa) |
2-3 days before |
2-3 days before |
Similar considerations as for other direct oral anticoagulants.
|
| Heparin (Unfractionated) |
4-6 hours before |
4-6 hours before |
Short-acting; can be paused closer to the surgery.
|
| Low Molecular Weight Heparin (LMWH) |
24 hours before |
24 hours before |
Enoxaparin typically paused 24 hours prior; consider renal function.
|
| NSAIDs (e.g., Ibuprofen) |
48-72 hours before |
48-72 hours before |
Avoid in cases where bleeding risk is significant.
|
- Discontinuing aspirin before cataract surgery is a practice driven by theoretical risks of bleeding, despite strong evidence from large-scale studies and meta-analyses showing that continuing aspirin does not significantly increase serious complications but poses real thrombotic risks and unnecessary healthcare disruptions.[3] [4]
Critical Ophthalmic Dosages
Antimalarials
| Parameter
|
Hydroxychloroquine
|
Chloroquine
|
| Daily Dose
|
5.0 mg/kg (actual body weight)
|
2.3 mg/kg (actual body weight)
|
| Cumulative Toxicity Threshold
|
>1000 g total
|
>460 g total
|
| High-Risk Duration
|
>5 years
|
>5 years
|
Clinical pearls:
* Use actual body weight for all BMI categories
* Annual retinal screening mandatory after 5 years of use
* Discontinue if retinal toxicity suspected
Toxoplasmosis Management
Prophylaxis
| Scenario
|
Regimen
|
Duration
|
| Paramacular recurrence
|
TMP-SMX 800/160mg q3d
|
Long-term
|
| Perioperative (LASIK/Phaco)
|
TMP-SMX 800/160mg daily
|
2 days pre-op → 1 week post-op
|
Adult Treatment
| Medication
|
Loading Dose
|
Maintenance
|
Adjuncts
|
| Pyrimethamine
|
200mg Day 1
|
50mg daily ×4wk
|
Folinic acid 15mg BIW
|
| Sulfadiazine
|
2g Day 1
|
1g QID ×4wk
|
Hydration + NaHCO₃
|
Alternate Regimens
| Option
|
Dose
|
Frequency
|
| Azithromycin
|
500mg
|
Daily ×4wk
|
| Clindamycin
|
300-450mg
|
q6h ×4wk
|
| TMP-SMX DS
|
1 tablet
|
BID ×4wk
|
Vision-Threatening Lesions
| Medication
|
Dose
|
Administration
|
| Prednisone
|
1-1.5 mg/kg/day
|
4-week taper
|
| Triamcinolone
|
40mg
|
Single periocular injection
|
Clinical pearls:
* Start steroids 72h after antimicrobial initiation
* Prepare TMP-SMX DS as double-strength tablets (160/800mg)
Congenital Toxoplasmosis
| Medication
|
Dose
|
Frequency
|
| Pyrimethamine
|
1mg/kg
|
q3d ×3wk
|
| Sulfadiazine
|
50-100mg/kg
|
BID ×3wk
|
| Folinic Acid
|
3mg
|
BIW during treatment
|
Clinical pearls:
* Pregnancy management: Spiramycin 1g TID for acute maternal infection
* Corticosteroid taper duration: 2-4 weeks based on response
Herpesviridae Therapy
HSV Treatment
| Medication
|
Acute Therapy
|
Prophylaxis
|
| Acyclovir
|
400mg 5×/day
|
400mg BID
|
| Valacyclovir
|
1000mg TID
|
500-1000mg daily
|
| Famciclovir
|
250mg TID
|
250mg BID
|
HZO Treatment
| Medication
|
Dose
|
Duration
|
| Acyclovir
|
800mg 5×/day
|
10-14 days
|
| Valacyclovir
|
1g TID
|
10-14 days
|
| Famciclovir
|
500mg TID
|
10-14 days
|
Clinical pearls:
* Recurrent HZO: Extend antiviral course to 21 days
* Topical steroids: Prednisolone 1% q2-6h based on severity
* Chronic prophylaxis: Reduce dose by 50% after 6 months
Intracameral Medications
| Medication
|
Concentration
|
Volume
|
Preparation Notes
|
| Cefuroxime
|
1 mg
|
0.1 mL
|
Standard reconstitution
|
| Moxifloxacin
|
150 µg/0.1 mL
|
0.3-0.4 mL
|
3 mL Vigamox + 7 mL BSS[5]
|
Clinical pearls:
* Inject moxifloxacin as final surgical step
* Maintain strict aseptic technique during dilution
Intravitreal Injections
| Medication
|
Dose
|
Indication
|
Notes
|
| Bevacizumab
|
1.25 mg/0.05 mL
|
Off-label use
|
0.675 mg/0.03 mL for ROP
|
| Ranibizumab
|
0.5 mg/0.05 mL
0.3 mg/0.05 mL
|
nAMD/RVO
DR/DME
|
Myopic CNVM
|
| Aflibercept
|
2.0 mg/0.05 mL
|
VEGF-mediated diseases
|
-
|
| Brolucizumab
|
6 mg/0.05 mL
|
nAMD
|
-
|
| Faricimab
|
6 mg/0.05 mL
|
DME/nAMD
|
-
|
| Triamcinolone
|
2 mg/0.05 mL
4 mg/0.1 mL
|
Off-label
|
Use Triesence®/Trivaris® for FDA-approved
|
| Ganciclovir
|
4 mg/0.1 mL
|
CMV retinitis
|
2 mg/0.05 mL twice weekly ×14d
|
| Clindamycin
|
1 mg/0.1 mL
|
Toxoplasmosis
|
-
|
| Foscarnet
|
2.4 mg/0.1 mL
|
Viral retinitis
|
1.2 mg/0.05 mL dose
|
| Fomivirsen
|
330 mcg/0.05 mL
|
CMV retinitis
|
-
|
| Methotrexate
|
400 mcg/0.1 mL
|
Intraocular lymphoma
|
-
|
| Vancomycin
|
1 mg/0.1 mL
|
Endophthalmitis
|
-
|
| Ceftazidime
|
2.25 mg/0.1 mL
|
Bacterial infections
|
-
|
| Amikacin
|
0.4 mg/0.1 mL
|
Gram-negative coverage
|
-
|
| Amphotericin B
|
5 mcg/0.1 mL
|
Fungal infections
|
-
|
| Voriconazole
|
50-100 mcg/0.1 mL
|
Fungal endophthalmitis
|
-
|
| Dexamethasone
|
0.4 mg/0.1 mL
|
Inflammation
|
-
|
Clinical pearls:
* Use 30G needles for all intravitreal injections
* Confirm needle position in mid-vitreous
* Monitor IOP post-injection
Fortified Ocular Topicals
| Medication
|
Concentration
|
Preparation Method
|
| Bacitracin
|
10,000 IU/mL
|
Reconstitute powder with sterile water
|
| Cefazolin
|
50 mg/mL (5%)
|
500mg vial + 10mL sterile saline
|
| Ceftriaxone
|
50 mg/mL (5%)
|
1g vial diluted in 20mL artificial tears
|
| Ceftazidime
|
50 mg/mL (5%)
|
1g vial + 10mL BSS + 10mL vehicle
|
| Vancomycin
|
50 mg/mL (5%)
|
500mg vial + 10mL sterile water
|
| Linezolid
|
2 mg/mL (0.2%)
|
IV solution diluted 1:10 with saline
|
| Gentamicin
|
14 mg/mL (1.4%)
|
80mg injectable + 5mL commercial drops
|
| Tobramycin
|
14 mg/mL (1.4%)
|
Same as gentamicin
|
| Amikacin
|
40 mg/mL (4%)
|
500mg vial + 12.5mL vehicle
|
| Clarithromycin
|
10 mg/mL (1%)
|
500mg tablet dissolved in 50mL vehicle
|
| Azithromycin
|
10 mg/mL (1%)
|
Reconstitute powder with sterile water
|
| Co-trimoxazole
|
16/80 mg/mL (TMP/SMX)
|
80/400mg tablet in 50mL vehicle
|
Clinical pearls:
* Refrigerate at 4°C; discard after 7 days (14 days for vancomycin)
* Use preservative-free artificial tears as base vehicle
* Shake suspensions vigorously before administration
* Monitor corneal epithelium daily with aminoglycosides
* TMP/SMX ratio maintained at 1:5 (16mg:80mg)
References:
2022-2023 Basic and Clinical Science Course, Section 01: Update on General Medicine by Herbert J. Ingraham , ISBN: 9781681045412 , Publication Date: 2022-08-30
2022-2023 Basic and Clinical Science Course, Section 02: Fundamentals and Principles of Ophthalmology by Vikram S. Brar Section 2 , ISBN: 9781681045429, Publication Date: 2022-08-30
022-2023 Basic and Clinical Science Course, Section 03: Clinical Optics and Vision Rehabilitation by Scott E. Brodie , ISBN: 9781681045436, Publication Date: 2022-06-20
2022-2023 Basic and Clinical Science Course, Section 04: Ophthalmic Pathology and Intraocular Tumors by Nasreen A. Syed ISBN: 9781681045443, Publication Date: 2022-06-20
2022-2023 Basic and Clinical Science Course, Section 05: Neuro-Ophthalmology by M. Tariq Bhatti, ISBN: 9781681045450, Publication Date: 2022-06-20
2022-2023 Basic and Clinical Science Course, Section 06: Pediatric Ophthalmology and Strabismus by Arif O. Khan, ISBN: 9781681045467, Publication Date: 2022-06-20
2022-2023 Basic and Clinical Science Course, Section 07: Oculofacial Plastic and Orbital Surgery by Bobby S. Korn, ISBN: 9781681045474, Publication Date: 2022-06-20
2022-2023 Basic and Clinical Science Course, Section 08: External Disease and Cornea by Robert W. Weisenthal, ISBN: 978168104548, Publication Date: 2022-06-20
2022-2023 Basic and Clinical Science Course, Section 09: Uveitis and Ocular Inflammation by H. Nida Sen, ISBN: 9781681045498, Publication Date: 2022-06-20
2022-2023 Basic and Clinical Science Course, Section 10: Glaucoma by Angelo P. Tanna, ISBN: 9781681045504, Publication Date: 2022-06-20
2022-2023 Basic and Clinical Science Course, Section 11: Lens and Cataract by Linda M. Tsai, ISBN: 9781681045511, Publication Date: 2022-06-20
2022-2023 Basic and Clinical Science Course, Section 12: Retina and Vitreous by Stephen J. Kim, ISBN: 9781681045528, Publication Date: 2022-06-20
2022-2023 Basic and Clinical Science Course, Section 13: Refractive Surgery by M. Bowes Hamill Restricted Resource, ISBN: 9781681045535, Publication Date: 2022-06-20
Nixon HK. Preparation of fortified antimicrobial eye drops. Kerala J Ophthalmol [serial online] 2018 [cited 2022 Dec 23];30:152-4. Available from: http://www.kjophthal.com/text.asp?2018/30/2/152/239986
https://eyewiki.aao.org/Herpes_Simplex_Uveitis#Medical_therapy
https://www.aao.org/current-insight/management-of-ocular-toxoplasmosis
- ↑ Li et al. 2021
- ↑ Fleck 1990
- ↑ Abo Zeid M, Elrosasy A, Alkheder A, et al. Do We Need to Hold Aspirin Before Cataract Surgery? A Systematic Review and Meta-Analysis of 65,196 Subjects. Semin Ophthalmol. Published online November 1, 2024. doi:10.1080/08820538.2024.2420969
- ↑ Benzimra JD, Johnston RL, Jaycock P, et al. The Cataract National Dataset electronic multicentre audit of 55,567 operations: antiplatelet and anticoagulant medications. Eye (Lond). 2009;23(1):10-16. doi:10.1038/sj.eye.6703069
- ↑ https://eyewiki.aao.org/Intracameral_Medications_Following_Cataract_Surgery