All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
H26.40 Cloudy posterior capsule
T85.29X Complication of intraocular lens
Disease
Capsular bag distension syndrome (CBDS) (i.e. capsular block syndrome, capsular bag hyperdistension, capsulorhexis block syndrome) is a rare complication of cataract surgery with in the bag intraocular lens placement where turbid fluid builds up in between the intraocular lens and posterior capsule, eventually leading to a decline in visual acuity for the patient.
Etiology & Epidemiology
One study estimates the occurrence of CBDS to occur in less than 1% (0.73%) of patients undergoing phacoemulsification with posterior chamber intraocular lens (PCIOL)
implantation.[1] Presentation can occur within a few weeks to months, or even years, after cataract surgery.[2]
Risk Factors
One large retrospective study found that eyes with axial lengths greater than 25 mm were at greater risk for CBDS. Patients receiving four-haptic PCIOLs, compared to C-loop IOLs, were also found to be at greater risk. Almost all cases are associated with continuous curvilinear capsulorhexis with an overlap all over the anterior surface of optic .[1]
General Pathology
CBDS occurs when fluid accumulates between the PCIOL and the posterior capsule, leading to distension of the posterior capsule with anterior displacement of the PCIOL. The trapped fluid develops a turbid consistency which leads to decreased visual acuity for the patient and can be associated with either a myopic (more common) or hyperopic shift.[3]
Pathophysiology
CBDS can be classified by time of onset, whether it occurs intraoperatively, early postoperatively (first few weeks), or late postoperatively (months or years).
- Intraoperative CBDS is felt to result from high irrigation pressures during hydrodissection which hyperdistends the posterior capsule, increasing the risk for posterior capsular rupture (PCR). The risk of PCR increases especially in case of violent or aggressive hydrodissection in a small capsulorrhexis.
- Early postoperative CBDS is associated with incomplete viscoelastic removal posterior to the IOL with resulting anterior IOL displacement leading to a myopic shift, anterior chamber shallowing, and IOP elevation.
- Late CBDS classically does not exhibit these symptoms and is only noticed due to the decreased visual acuity recognized by the patient.[4]
There are three distinct types of CBDS:
- noncellular,
- inflammatory, and
- fibrotic.[3]
Non-cellular and inflammatory CBDS occur in the early post-operative timeframe. The fibrotic phase occurs in the late timeframe and is secondary to residual lenticular epithelial cells which undergo metaplasia and proliferate, producing various types of collagen and extracellular matrix that accumulate in the capsular bag.[5] In one case report, retained fluid from a treated late onset CBDS was analyzed and electrophoresis showed large amounts of alpha-crystalline, confirming that the fluid was from residual lens epithelial cells. No gammaglobulins were noted, suggesting antigen-antibody mediated hypersensitivity has no role in the pathophysiology. [6]
Diagnosis
Symptomatic patients will have decreased visual acuity. If significant anterior displacement of the lens-diaphragm exists, IOP may also be elevated.
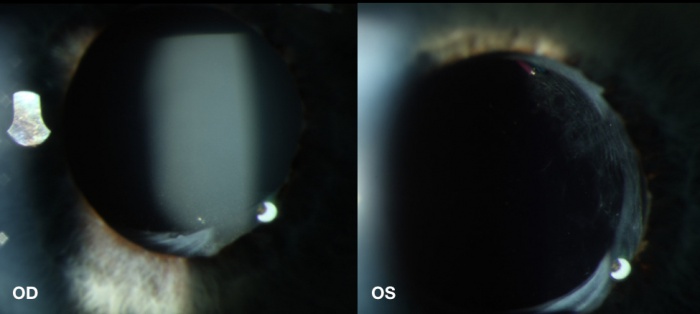
Diagnosis can be made at the slit lamp in the most obvious cases. Turbid, opaque fluid can be visualized between the IOL and posterior capsule (Figure 1). Most of such cases have small capsulorrhexis (5mm or smaller in diameter and an adhesion between the lens optic and anterior capsular rim. When the smoky, turbid fluid is visible between the IOL and clear posterior capsular, a layering effect produces a phenomena known as a retrolenticular pseudohypopyon.[2] Comparing the clarity of the space behind the IOL in the fellow eye makes the opacity much more prevalent. Some cases may have some opacification of the IOL or IOL glistening.[8]
Slit lamp biomicroscopy may also demonstrate shallowing of the anterior chamber, tight apposition of the iris to lens implant, anterior bowing of the iris, or late capsular fibrosis.[2]
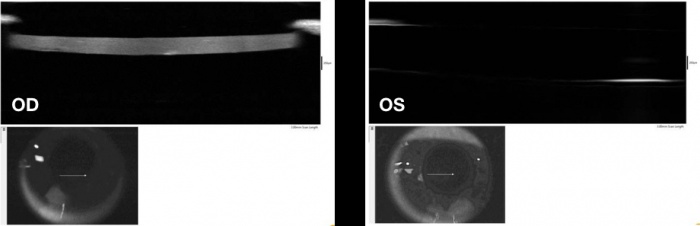
Anterior segment optical coherence tomography (OCT)[10] and anterior ultrasound biomicroscopy (UBM) can help identify early, presymptomatic CBDS (see various types below) as well as better classify capsular distension and/or IOL optic displacement (Figure 2).[11] The Scheimpflug camera can also be used but UBM has been shown to be superior when the capsular bag is very distended. [12][13]
History
Patients will have had cataract surgery with in-the-bag intraocular lens placement ranging from weeks prior to many years (even greater than a decade) prior with gradual fogging or dimming of vision.
Symptoms
Symptoms include a gradual decrease in visual acuity. Patients often describe their vision as foggier or dimmer than the fellow eye. Rarely, symptoms can also include eye pain, irritation, and/or eye redness when CBDS either leads to an inflammatory reaction in the anterior chamber or even more rarely is associated with Propionibacterium acnes endophthalmitis.
Clinical diagnosis
One study of 17 eyes of 16 patients with CBDS identified four types of CBDS[4]:
- Type 1: Transparent capsule and transparent liquid in the capsular bag, barely noticeable via slit lamp biomicroscopy but clearly seen on anterior segment OCT
- Type 2: Homogenous milky fluid in the capsular bag and a transparent posterior capsule
- Type 3: Transparent or semitransparent liquid accumulation and posterior capsular opacification
- Type 4: Opaque contents and posterior capsular opacification +/- Soemmering’s ring
Differential diagnosis
- Posterior capsular opacification
- Chronic endophthalmitis (P. acnes endophthalmitis)
- Chronic endophthalmitis associated with CBDS
- Pupillary block glaucoma
Management
General treatment
Treatment most commonly entails Nd:YAG laser posterior and/or anterior capsulotomy. YAG allows for quick release of the trapped fluid and returning the IOL to its previous position, resolving the patient’s myopic shift and visual blurring.[5] Openings are most commonly made in the posterior capsule. However, if the posterior capsule is clear one can elect to create a small opening in the anterior capsule just peripheral to the edge of the lens implant, after which fluid will vent into the anterior chamber where it is quickly cleared through normal aqueous humor turnover. If this latter approach is taken, some clinicians recommend short course of topical steroids due to the higher risk of post-op inflammation.[2] The liberated lens matters may also cause an increase in intraocular pressure which however, usually responds to medical therapy.
In early, asymptomatic cases clinicians can also elect to observe. If cortical masses protruding from the anterior capsule lead to inflammation, topical anti-inflammatory medications can be utilized and surgical aspiration may be necessary or even pars plana vitrectomy with posterior capsulotomy. If P. acnes chronic endophthalmitis is suspected in conjunction with CBDS, pars plana vitrectomy, removal of the debris as much as possible and total capsulotomy may be necessary.[14]
Vlasenko et al.[4] recommend the following treatments for the previously mentioned CBDS types:
- Type 1: Follow-up
- Type 2: If symptomatic, YAG Capsulotomy; if not, observe
- Type 3: YAG Capsulotomy
- Type 4: YAG Capsulotomy, unless inflammatory symptoms develop, then consider topical anti-inflammatories and surgical aspiration
Some surgeons advocate bimanual irrigation and aspiration for all cases of late CBDS, with the logic being that this allows culture of the fluid to test for P. acnes as well as preventing the spread of any bacterium into the vitreous cavity. Indeed, cases of P. acnes endophthalmitis have been noted after simple YAG capsulotomy without the presence of any turbid fluid from CBDS. In one reported case of bimanual irrigation and aspiration for CBDS where culture revealed P. acnes, no anterior chamber cell and flare was seen on the pre-operative exam.[15] However, these cases are exceedingly rare and most surgeons, in the absence of any inflammatory symptoms or signs, elect for simple YAG capsulotomy.
Surgical follow up
Clinicians should watch for post-operative inflammation as rare cases of P. acnes endophthalmitis have been reported following Nd:YAG treatment for other indications, possibly due to release of a sequestered low-virulent organism.[16]
Complications
YAG capsulotomy is generally safe, with documented complications including a transient rise in intraocular pressure, lens subluxation or dislocation, lens pitting, or retinal detachment.[17]
Prognosis
Prognosis is excellent with only a few YAG laser applications usually needed for resolution of the turbid fluid. Patient’s achieve a brisk return to baseline visual acuity.
References
- ↑ Jump up to: 1.0 1.1 Kim HK, et al. Capsular block syndrome after cataract surgery: clinical analysis and classification. J Cataract Refract Surg. 2008;34:357–63.
- ↑ Jump up to: 2.0 2.1 2.2 2.3 Burk, R. Capsular Bag Distension Syndrome. 12 January 2015. Available at: http://odpcli.com/articles/capsular-bag-distension-syndrome. Accessed August 26, 2018.
- ↑ Jump up to: 3.0 3.1 Killoran E, Haugsdal J, Oetting TA. Capsular Block Syndrome: An Unusual Presentation. EyeRounds.org. July 6, 2016; Available from: http://EyeRounds.org/cases/238-Capsular-Block-Syndrome.htm
- ↑ Jump up to: 4.0 4.1 4.2 Vlasenko A, Malyugin B, Verzin A, Uzunyan D. Capsular bag distention syndrome: case series and management strategies. European society of cataract and refractive surgeons. 10 October 2017.
- ↑ Jump up to: 5.0 5.1 Wendrix G, Zeyen T. Late-onset capsular bag distension syndrome after cataract surgery: 2 case- reports. Bull Soc Belge Ophtalmol. 2006;301:67–9.
- ↑ Eifrig DE Capsulorhexis-related lacteocrumenasia. J Cataract Refract Surg 1997;23:450–4
- ↑ Photo courtesy of Danny A. Mammo M.D. and Amanda Maltry M.D
- ↑ Tripathy K, Sridhar U. Optical coherence tomography of intraocular lens glistening. Indian J Ophthalmol. 2019;67(1):138–139. doi:10.4103/ijo.IJO_1031_18
- ↑ Photo courtesy of Danny A. Mammo M.D. and Amanda Maltry M.D
- ↑ Tripathy K. Posterior Capsular Cyst on Anterior Segment OCT. Ophthalmology. 2018;125(9):1324. doi:10.1016/j.ophtha.2018.06.033
- ↑ Das K. Delayed capsular bag distension syndrome. Oman Journal of Ophthalmology. 2010;3(3):155-156. doi:10.4103/0974-620X.71905.
- ↑ Jain R, Grewal D, Gupta R, Grewal SPS Scheimpflug imaging in late capsular bag distention syndrome after phacoemulsification. Am J Ophthalmol 2006;142:1083–5
- ↑ Kucukevcilioglu, M., Hurmeric, V., Erdurman, F.C., Ceylan, O.M. Imaging late capsular block syndrome: ultrasound biomicroscopy versus Scheimpflug camera. J Cataract Refract Surg 2011;37:2071-2074.
- ↑ Aldave AJ, Stein JD, Deramo VA, Shah GK, Fischer DH, Maguire JI. Treatment strategies for postoperative Propionibacterium acnes endophthalmitis. Ophthalmology. 1999;106(12):2395-401.
- ↑ Management of late postoperative capsular block syndrome with accumulation of Propionibacterium acnes. Mojzis, Peter et al. Canadian Journal of Ophthalmology , Volume 49 , Issue 3 , e76 - e77
- ↑ Chaudhry M, Baisakhiya S, Bhatia MS. A rare complication of Nd-YAG capsulotomy: propionibacterium acnes endopthalmitis. Nepal J Ophthalmol. 2011;3(1):80-2.
- ↑ Karahan E, Er D, Kaynak S. An Overview of Nd:YAG Laser Capsulotomy . Medical Hypothesis, Discovery and Innovation in Ophthalmology. 2014;3(2):45-50.

